Abstract
Background
Although immunotherapy with immune checkpoint inhibitors (ICIs) has become a standard therapeutic strategy in colorectal cancer (CRC) exhibiting microsatellite instability-high, limited patients benefit from this new approach. To increase the efficacy of ICIs in CRC patients, it is crucial to control the function of immunosuppressive cells in the tumor microenvironment. M2-tumor-associated macrophages (TAMs) are key immunosuppressive cells and promote tumor growth, angiogenesis, and epithelial-mesenchymal transition. In the present study, we focused on the VEGF signaling pathway in M2-TAMs to control their inhibitory function.
Methods
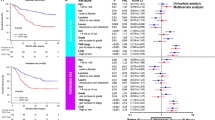
We evaluated the population of M2-TAMs, the VEGF receptor 2 (VEGFR2) expression on M2-TAMs, and the correlation between HIF-1α-positive cells and VEGFR2 expression levels on M2-TAMs in CRC using the analysis of The Cancer Genome Atlas colorectal adenocarcinoma dataset (n = 592), the flow cytometry of freshly resected surgical specimens of CRC (n = 20), and the immunofluorescence staining of formalin-fixed paraffin-embedded whole tissue samples of CRC (n = 20). Furthermore, we performed a functional assay of M2 macrophages through the VEGF/VEGFR2 signaling pathway in vitro.
Results
The population of M2-TAMs and their VEGFR2 expression significantly increased in the tumor compared to the normal mucosa in the CRC patients. HIF1-α-positive cells significantly correlated with the VEGFR2 expression level of M2-TAMs. M2 macrophages induced by cytokines in vitro produced TGF-β1 through the VEGF/VEGFR2 signaling pathway.
Conclusions
Our results suggest that anti-VEGFR2 therapy may have therapeutic potential to control the immune inhibitory functions of M2-TAMs in CRC, resulting in enhanced efficacy of immunotherapy with ICIs.




Similar content being viewed by others
Abbreviations
- CRC:
-
Colorectal cancer
- EMT:
-
Epithelial-mesenchymal transition
- FFPE:
-
Formalin-fixed paraffin-embedded
- HIF:
-
Hypoxia-inducible factor
- HPD:
-
Hyper progressive disease
- ICIs:
-
Immune checkpoint inhibitors
- KDR:
-
Kinase insert domain receptor
- TAMs:
-
Tumor-associated macrophages
- TCGA:
-
The Cancer Genome Atlas
- VEGFR2:
-
VEGF receptor 2
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Cercek A, Roxburgh CSD, Strombom P, Smith JJ, Temple LKF, Nash GM, Guillem JG, Paty PB, Yaeger R, Stadler ZK, Seier K, Gonen M, Segal NH, Reidy DL, Varghese A, Shia J, Vakiani E, Wu AJ, Crane CH, Gollub MJ, Garcia-Aguilar J, Saltz LB, Weiser MR (2018) Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2018.0071
Gollins S, Sebag-Montefiore D (2016) Neoadjuvant treatment strategies for locally advanced rectal cancer. Clin Oncol 28(2):146–151. https://doi.org/10.1016/j.clon.2015.11.003
Overman MJ, Lonardi S, Wong KYM, Lenz HJ, Gelsomino F, Aglietta M, Morse MA, Van Cutsem E, McDermott R, Hill A, Sawyer MB, Hendlisz A, Neyns B, Svrcek M, Moss RA, Ledeine JM, Cao ZA, Kamble S, Kopetz S, Andre T (2018) Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer. J Clin Oncol 36(8):773–779. https://doi.org/10.1200/jco.2017.76.9901
Overman MJ, McDermott R, Leach JL, Lonardi S, Lenz HJ, Morse MA, Desai J, Hill A, Axelson M, Moss RA, Goldberg MV, Cao ZA, Ledeine JM, Maglinte GA, Kopetz S, Andre T (2017) Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 18(9):1182–1191. https://doi.org/10.1016/S1470-2045(17)30422-9
Shibuya KC, Goel VK, Xiong W, Sham JG, Pollack SM, Leahy AM, Whiting SH, Yeh MM, Yee C, Riddell SR, Pillarisetty VG (2014) Pancreatic ductal adenocarcinoma contains an effector and regulatory immune cell infiltrate that is altered by multimodal neoadjuvant treatment. PLoS ONE 9(5):e96565. https://doi.org/10.1371/journal.pone.0096565
De Monte L, Reni M, Tassi E, Clavenna D, Papa I, Recalde H, Braga M, Di Carlo V, Doglioni C, Protti MP (2011) Intratumor T helper type 2 cell infiltrate correlates with cancer-associated fibroblast thymic stromal lymphopoietin production and reduced survival in pancreatic cancer. J Exp Med 208(3):469–478. https://doi.org/10.1084/jem.20101876
Qian BZ, Pollard JW (2010) Macrophage diversity enhances tumor progression and metastasis. Cell 141(1):39–51. https://doi.org/10.1016/j.cell.2010.03.014
Condeelis J, Pollard JW (2006) Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell 124(2):263–266. https://doi.org/10.1016/j.cell.2006.01.007
Pollard JW (2004) Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer 4(1):71–78. https://doi.org/10.1038/nrc1256
Yang L, Zhang Y (2017) Tumor-associated macrophages: from basic research to clinical application. J Hematol Oncol 10(1):58. https://doi.org/10.1186/s13045-017-0430-2
Nakajima S, Koh V, Kua LF, So J, Davide L, Lim KS, Petersen SH, Yong WP, Shabbir A, Kono K (2016) Accumulation of CD11c+CD163+ adipose tissue macrophages through upregulation of intracellular 11beta-HSD1 in human obesity. J Immunol 197(9):3735–3745. https://doi.org/10.4049/jimmunol.1600895
Hinshaw DC, Shevde LA (2019) The tumor microenvironment innately modulates cancer progression. Can Res 79(18):4557–4566. https://doi.org/10.1158/0008-5472.Can-18-3962
Mantovani A, Sica A (2010) Macrophages, innate immunity and cancer: balance, tolerance, and diversity. Curr Opin Immunol 22(2):231–237. https://doi.org/10.1016/j.coi.2010.01.009
Biswas SK, Gangi L, Paul S, Schioppa T, Saccani A, Sironi M, Bottazzi B, Doni A, Vincenzo B, Pasqualini F, Vago L, Nebuloni M, Mantovani A, Sica A (2006) A distinct and unique transcriptional program expressed by tumor-associated macrophages (defective NF-kappaB and enhanced IRF-3/STAT1 activation). Blood 107(5):2112–2122. https://doi.org/10.1182/blood-2005-01-0428
Batlle E, Massague J (2019) Transforming growth factor-beta signaling in immunity and cancer. Immunity 50(4):924–940. https://doi.org/10.1016/j.immuni.2019.03.024
Kikuchi T, Mimura K, Ashizawa M, Okayama H, Endo E, Saito K, Sakamoto W, Fujita S, Endo H, Saito M, Momma T, Saze Z, Ohki S, Shimada K, Yoshimura K, Tsunoda T, Kono K (2020) Characterization of tumor-infiltrating immune cells in relation to microbiota in colorectal cancers. Cancer Immunol Immunother 69(1):23–32. https://doi.org/10.1007/s00262-019-02433-6
Wheeler KC, Jena MK, Pradhan BS, Nayak N, Das S, Hsu CD, Wheeler DS, Chen K, Nayak NR (2018) VEGF may contribute to macrophage recruitment and M2 polarization in the decidua. PLoS ONE 13(1):e0191040. https://doi.org/10.1371/journal.pone.0191040
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, Cerami E, Sander C, Schultz N (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6(269):pl1. https://doi.org/10.1126/scisignal.2004088
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, Jacobsen A, Byrne CJ, Heuer ML, Larsson E, Antipin Y, Reva B, Goldberg AP, Sander C, Schultz N (2012) The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov 2(5):401–404. https://doi.org/10.1158/2159-8290.Cd-12-0095
Nakayama Y, Mimura K, Tamaki T, Shiraishi K, Kua LF, Koh V, Ohmori M, Kimura A, Inoue S, Okayama H, Suzuki Y, Nakazawa T, Ichikawa D, Kono K (2019) PhosphoSTAT1 expression as a potential biomarker for antiPD1/antiPDL1 immunotherapy for breast cancer. Int J Oncol 54(6):2030–2038. https://doi.org/10.3892/ijo.2019.4779
Kikuchi T, Mimura K, Okayama H, Nakayama Y, Saito K, Yamada L, Endo E, Sakamoto W, Fujita S, Endo H, Saito M, Momma T, Saze Z, Ohki S, Kono K (2019) A subset of patients with MSS/MSI-low-colorectal cancer showed increased CD8(+) TILs together with up-regulated IFN-gamma. Oncol Lett 18(6):5977–5985. https://doi.org/10.3892/ol.2019.10953
Nakayama Y, Mimura K, Kua LF, Okayama H, Min AKT, Saito K, Hanayama H, Watanabe Y, Saito M, Momma T, Saze Z, Ohki S, Suzuki Y, Ichikawa D, Yong WP, Kono K (2020) Immune suppression caused by PD-L2 expression on tumor cells in gastric cancer. Gastric Cancer. https://doi.org/10.1007/s10120-020-01079-z
Zarif JC, Hernandez JR, Verdone JE, Campbell SP, Drake CG, Pienta KJ (2016) A phased strategy to differentiate human CD14+monocytes into classically and alternatively activated macrophages and dendritic cells. Biotechniques 61(1):33–41. https://doi.org/10.2144/000114435
Onozawa H, Saito M, Saito K, Kanke Y, Watanabe Y, Hayase S, Sakamoto W, Ishigame T, Momma T, Ohki S, Takenoshita S (2017) Annexin A1 is involved in resistance to 5-FU in colon cancer cells. Oncol Rep 37(1):235–240. https://doi.org/10.3892/or.2016.5234
Okano M, Kumamoto K, Saito M, Onozawa H, Saito K, Abe N, Ohtake T, Takenoshita S (2015) Upregulated Annexin A1 promotes cellular invasion in triple-negative breast cancer. Oncol Rep 33(3):1064–1070. https://doi.org/10.3892/or.2015.3720
Thar Min AK, Okayama H, Saito M, Ashizawa M, Aoto K, Nakajima T, Saito K, Hayase S, Sakamoto W, Tada T, Hanayama H, Saze Z, Momma T, Ohki S, Sato Y, Motoyama S, Mimura K, Kono K (2018) Epithelial-mesenchymal transition-converted tumor cells can induce T-cell apoptosis through upregulation of programmed death ligand 1 expression in esophageal squamous cell carcinoma. Cancer Med. https://doi.org/10.1002/cam4.1564
Ashizawa M, Okayama H, Ishigame T, Thar Min AK, Saito K, Ujiie D, Murakami Y, Kikuchi T, Nakayama Y, Noda M, Tada T, Endo H, Fujita S, Sakamoto W, Saito M, Saze Z, Momma T, Ohki S, Mimura K, Kono K (2019) miRNA-148a-3p regulates immunosuppression in DNA mismatch repair-deficient colorectal cancer by targeting PD-L1. Mol Cancer Res 17(6):1403–1413. https://doi.org/10.1158/1541-7786.Mcr-18-0831
Etzerodt A, Tsalkitzi K, Maniecki M, Damsky W, Delfini M, Baudoin E, Moulin M, Bosenberg M, Graversen JH, Auphan-Anezin N, Moestrup SK, Lawrence T (2019) Specific targeting of CD163(+) TAMs mobilizes inflammatory monocytes and promotes T cell-mediated tumor regression. J Exp Med 216(10):2394–2411. https://doi.org/10.1084/jem.20182124
Komohara Y, Jinushi M, Takeya M (2014) Clinical significance of macrophage heterogeneity in human malignant tumors. Cancer Sci 105(1):1–8. https://doi.org/10.1111/cas.12314
Laoui D, Van Overmeire E, Di Conza G, Aldeni C, Keirsse J, Morias Y, Movahedi K, Houbracken I, Schouppe E, Elkrim Y, Karroum O, Jordan B, Carmeliet P, Gysemans C, De Baetselier P, Mazzone M, Van Ginderachter JA (2014) Tumor hypoxia does not drive differentiation of tumor-associated macrophages but rather fine-tunes the M2-like macrophage population. Can Res 74(1):24–30. https://doi.org/10.1158/0008-5472.Can-13-1196
Colegio OR, Chu NQ, Szabo AL, Chu T, Rhebergen AM, Jairam V, Cyrus N, Brokowski CE, Eisenbarth SC, Phillips GM, Cline GW, Phillips AJ, Medzhitov R (2014) Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature 513(7519):559–563. https://doi.org/10.1038/nature13490
Mantovani A, Marchesi F, Malesci A, Laghi L, Allavena P (2017) Tumour-associated macrophages as treatment targets in oncology. Nat Rev Clin Oncol 14(7):399–416. https://doi.org/10.1038/nrclinonc.2016.217
Massague J (2008) TGFbeta in cancer. Cell 134(2):215–230. https://doi.org/10.1016/j.cell.2008.07.001
Wrzesinski SH, Wan YY, Flavell RA (2007) Transforming growth factor-beta and the immune response: implications for anticancer therapy. Clin Cancer Res 13(18 Pt 1):5262–5270. https://doi.org/10.1158/1078-0432.Ccr-07-1157
Flavell RA, Sanjabi S, Wrzesinski SH, Licona-Limon P (2010) The polarization of immune cells in the tumour environment by TGFbeta. Nat Rev Immunol 10(8):554–567. https://doi.org/10.1038/nri2808
Moore KW, de Waal MR, Coffman RL, O'Garra A (2001) Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol 19:683–765. https://doi.org/10.1146/annurev.immunol.19.1.683
Fukumura D, Kloepper J, Amoozgar Z, Duda DG, Jain RK (2018) Enhancing cancer immunotherapy using antiangiogenics: opportunities and challenges. Nat Rev Clin Oncol 15(5):325–340. https://doi.org/10.1038/nrclinonc.2018.29
Lo Russo G, Moro M, Sommariva M, Cancila V, Boeri M, Centonze G, Ferro S, Ganzinelli M, Gasparini P, Huber V, Milione M, Porcu L, Proto C, Pruneri G, Signorelli D, Sangaletti S, Sfondrini L, Storti C, Tassi E, Bardelli A, Marsoni S, Torri V, Tripodo C, Colombo MP, Anichini A, Rivoltini L, Balsari A, Sozzi G, Garassino MC (2019) Antibody-Fc/FcR interaction on macrophages as a mechanism for hyperprogressive disease in non-small cell lung cancer subsequent to PD-1/PD-L1 blockade. Clin Cancer Res 25(3):989–999. https://doi.org/10.1158/1078-0432.Ccr-18-1390
Gordon SR, Maute RL, Dulken BW, Hutter G, George BM, McCracken MN, Gupta R, Tsai JM, Sinha R, Corey D, Ring AM, Connolly AJ, Weissman IL (2017) PD-1 expression by tumour-associated macrophages inhibits phagocytosis and tumour immunity. Nature 545(7655):495–499. https://doi.org/10.1038/nature22396
Funding
No relevant funding.
Author information
Authors and Affiliations
Contributions
KM and KK contributed to the study conception and design. HO, WS, SF, HE, MS, ZS, TM, and SO contributed to the acquisition of patient samples. AKTM and SN performed flow cytometry and in vitro assay. AKTM, SN, and KS performed immunofluorescence staining. AKTM, KM, SN, HO, KS, WS, SF, HE, MS, ZS, TM, SO, and KK performed analysis and interpretation of results. AKTM, KM, and KK drafted the manuscript. All the authors are aware of and agree to the contents of the paper, as well as them being listed as authors on the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted in accordance with the ethical principles of the 1964 Declaration of Helsinki and its later amendments and was approved by the Fukushima Medical University Research Ethics Committee (Reference Nos. 2289 and 29316).
Informed consent
Written informed consent was obtained from all patients included in the study for the use of their specimens and clinical data for research and publication prior to collecting the specimens at Fukushima Medical University Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Min, A.K.T., Mimura, K., Nakajima, S. et al. Therapeutic potential of anti-VEGF receptor 2 therapy targeting for M2-tumor-associated macrophages in colorectal cancer. Cancer Immunol Immunother 70, 289–298 (2021). https://doi.org/10.1007/s00262-020-02676-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-020-02676-8