Abstract
Purpose
Adequate monitoring of changes in tumor load is fundamental for the assessment of the course of disease and response to treatment. There is an ongoing debate on the utility of RECIST v1.1 in gastroenteropancreatic neuroendocrine tumors (GEP-NETs).
Methods
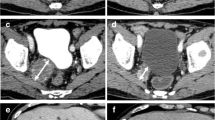
In this retrospective real-life cohort study, Choi-criteria were compared with RECIST v1.1. The agreement between both criteria and the association with survival endpoints were evaluated.
Results
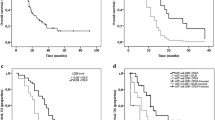
Seventy-five patients were included with a median follow-up of 35 months (range 8–53). Median progression-free survival (mPFS) according to RECIST v1.1 was 15 months (range 2–50) compared to 14 months (range 2–50) in Choi. According to RECIST, 33 (44%) patients were classified as having stable disease (SD), 40 (53%) as progressive disease (PD) and two (3%) patients as partial response (PR), compared to 9 (12%) patients classified as SD, 50 (67%) as PD and 16 (21%) as PR according to Choi-criteria. Overall concordance between the criteria was moderate (Cohen’s Kappa = 0.408, p < 0.001) and agreement varied between 57 and 69% at each consecutive scan (p < 0.001). Survival analysis showed significant differences in overall survival (OS) for RECIST v1.1 categories PD and non-PD (log-rank p = 0.02), however, in Choi no significant differences in OS were found (p = 0.27).
Conclusion
RECIST v1.1 had a better clinical utility and prognostic value compared to Choi-criteria. Still, RECIST were also not sufficient to adequately predict OS. This outlines the need for new tools that provides accurate information on the disease course and treatment response to support precise prognostication in patients with GEP-NETs.
Graphical abstract






Similar content being viewed by others
References
Cives M, Strosberg JR. Gastroenteropancreatic Neuroendocrine Tumors. CA Cancer J Clin. 2018 Nov;68(6):471–87.
Modlin I, Oberg K, Chung D. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008;9(January):61–72.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017. DOI: https://doi.org/10.1001/jamaoncol.2017.0589
Knigge U, Capdevila J, Bartsch DK, Baudin E, Falkerby J, Kianmanesh R, et al. ENETS Consensus Recommendations for the Standards of Care in Neuroendocrine Neoplasms: Follow-Up and Documentation. Neuroendocrinology. 2017; pp 310–9.
Halfdanarson TR, Strosberg JR, Tang L, Bellizzi AM, Bergsland EK, O TM, et al. The North American Neuroendocrine Tumor Society Consensus Guidelines for Surveillance and Medical Management of Pancreatic Neuroendocrine Tumors. 2020. DOI: https://doi.org/10.1097/MPA.0000000000001597
Pavel M, O’Toole D, Costa F, Capdevila J, Gross D, Kianmanesh R, et al. ENETS Consensus Guidelines Update for the Management of Distant Metastatic Disease of Intestinal, Pancreatic, Bronchial Neuroendocrine Neoplasms (NEN) and NEN of Unknown Primary Site. Neuroendocrinology. 2016;103(2):172–85.
Strosberg JR, Halfdanarson TR, Bellizzi AM, Chan JA, Dillon JS, Heaney AP, et al. The north American neuroendocrine tumor society consensus guidelines for surveillance and medical management of midgut neuroendocrine tumors. Pancreas. 2017;46(6):707–14.
van Treijen MJC, van der Zee D, Heeres BC, Staal FCR, Vriens MR, Saveur LJ, et al. Blood Molecular Genomic analysis predicts the disease course of GEP NET patients: a validation study of the predictive value of the NETest®. Neuroendocrinology. 2020. DOI: https://doi.org/10.1159/000509091
Hofland J, Zandee WT, de Herder WW. Role of biomarker tests for diagnosis of neuroendocrine tumours. Nat Rev Endocrinol. 2018;14(11):656–69.
Öberg K, Califano A, Strosberg JR, Ma S, Pape U, Bodei L, et al. A meta-analysis of the accuracy of a neuroendocrine tumor mRNA genomic biomarker (NETest) in blood. Ann Oncol. 2020. DOI: https://doi.org/10.1016/j.annonc.2019.11.003
Sundin A, Arnold R, Baudin E, Cwikla JB, Eriksson B, Fanti S, et al. ENETS Consensus Guidelines for the Standards of Care in Neuroendocrine Tumors: Radiological, Nuclear Medicine and Hybrid Imaging. Neuroendocrinology. 2017. DOI: https://doi.org/10.1159/000471879
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Schwartz LH, Litière S, Vries E De, Ford R, Mandrekar S, Shankar L, et al. RECIST 1.1 – Update and Clarification: From the RECIST Committee. 2017;132–7.
Faivre S, Ronot M, Dreyer C, Serrate C, Hentic O, Bouattour M, et al. Imaging response in neuroendocrine tumors treated with targeted therapies: The experience of sunitinib. Target Oncol. 2012 Jun;7(2):127–33.
Dromain C, de Baere T, Lumbroso J, Caillet H, Laplanche A, Boige V, et al. Detection of liver metastases from endocrine tumors: A prospective comparison of somatostatin receptor scintigraphy, computed tomography, and magnetic resonance imaging. J Clin Oncol. 2005. DOI: https://doi.org/10.1200/JCO.2005.01.013
Sharma MR, Maitland ML, Ratain MJ, Fojo AT, Noonan A. RECIST: No longer the sharpest tool in the oncology clinical trials toolbox - Point/Counterpoint. Cancer Res. 2012;72(20):5145–50.
de Mestier L, Dromain C, d’Assignies G, Scoazec J-Y, Lassau N, Lebtahi R, et al. Evaluating digestive neuroendocrine tumor progression and therapeutic responses in the era of targeted therapies: state of the art. Endocr Relat Cancer. 2014 Apr;21(3):R105–20.
Lamarca A, Barriuso J, Kulke M, Borbath I, Lenz HJ, Raoul JL, et al. Determination of an optimal response cut-off able to predict progression-free survival in patients with well-differentiated advanced pancreatic neuroendocrine tumours treated with sunitinib: An alternative to the current RECIST-defined response. Br J Cancer. 2018;118(2):181–8.
Merino-Casabiel X, Aller J, Arbizu J, García-Figueiras R, González C, Grande E, et al. Consensus document on the progression and treatment response criteria in gastroenteropancreatic neuroendocrine tumors. Clin Transl Oncol. 2018 Dec;20(12):1522–8.
Choi H, Charnsangavej C, Faria SC, Macapinlac HA, Burgess MA, Patel SR, et al. Correlation of Computed Tomography and Positron Emission Tomography in Patients With Metastatic Gastrointestinal Stromal Tumor Treated at a Single Institution With Imatinib Mesylate: Proposal of New Computed Tomography Response Criteria. J Clin Oncol. 2007 May;25(13):1753–9.
Luo Y, Chen J, Huang K, Lin Y, Chen M, Xu L, et al. Early evaluation of sunitinib for the treatment of advanced gastroenteropancreatic neuroendocrine neoplasms via CT imaging: RECIST 1.1 or Choi Criteria? BMC Cancer. 2017 Feb;17. https://doi.org/10.1186/s12885-017-3150-7
Solis-Hernandez MP, Carmona-Bayonas A, Calvo-Temprano D, Nunez B, Custodio A, Alonso T, et al. Radiological Changes in the Treatment of Pancreatic Neuroendocrine Tumors (PNET) with Sunitinib: RECIST vs CHOI Criteria. CRIPNET-GETNE Study. Neuroendocrinology. 2017;105(1):174.
Huizing DMV, Aalbersberg EA, Versleijen MWJ, Tesselaar MET, Walraven I, Lahaye MJ, et al. Early response assessment and prediction of overall survival after peptide receptor radionuclide therapy. Cancer Imaging. 2020 Aug;20(1). https://doi.org/10.1186/s40644-020-00335-w
Weber EM, Titman AC. Quantifying the association between progression-free survival and overall survival in oncology trials using Kendall’s τ. Stat Med. 2019 Feb;38(5):703–19.
Oberg K, Krenning E, Sundin A, Bodei L, Kidd M, Tesselaar M, et al. A Delphic consensus assessment: imaging and biomarkers in gastroenteropancreatic neuroendocrine tumor disease management. Endocr Connect. 2016;5(5):174–87.
Solis-Hernandez M aP, Fernandez del Valle A, Carmona-Bayonas A, Garcia-Carbonero R, Custodio A, Benavent M, et al. Evaluating radiological response in pancreatic neuroendocrine tumours treated with sunitinib: comparison of Choi versus RECIST criteria (CRIPNET_ GETNE1504 study). Br J Cancer. 2019. https://doi.org/10.1038/s41416-019-0558-7
Luo Y, Chen J, Huang K, Lin Y, Chen M, Xu L, et al. Early evaluation of sunitinib for the treatment of advanced gastroenteropancreatic neuroendocrine neoplasms via CT imaging: RECIST 1.1 or Choi Criteria? BMC Cancer. 2017. https://doi.org/10.1186/s12885-017-3150-7
Gu D, Hu Y, Ding H, Wei J, Chen K, Liu H, et al. CT radiomics may predict the grade of pancreatic neuroendocrine tumors: a multicenter study. Eur Radiol. 2019. DOI: https://doi.org/10.1007/s00330-019-06176-x
Kidd M, Drozdov I, Modlin I. Blood and tissue neuroendocrine tumor gene cluster analysis correlate, define hallmarks and predict disease status. Endocr Relat Cancer. 2015;22(4):561–75.
Acknowledgements
We would like to thank Marieke Ten Holter-Pieterman MA, MEd and Carla Pieterman, MD, PhD for proof-reading the manuscript.
Author information
Authors and Affiliations
Contributions
MJCT and JMHS performed the analysis and wrote the manuscript with input from all authors. DZ and BCH reassessed all imaging studies. GDV, MM and METT supervised the project. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported. No funding was received for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
van Treijen, M.J.C., Schoevers, J.M.H., Heeres, B.C. et al. Defining disease status in gastroenteropancreatic neuroendocrine tumors: Choi-criteria or RECIST?. Abdom Radiol 47, 1071–1081 (2022). https://doi.org/10.1007/s00261-021-03393-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03393-1