Abstract
Objective
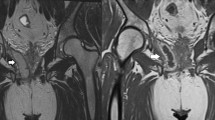
The purpose of this article is to review MRI technique, relevant anatomy, and MRI classification systems for the assessment of perianal fistulising disease. We present a stepwise approach to the assessment of perianal fistulas on MRI utilizing a systematic reporting format.
Conclusion
MRI is invaluable for the assessment of perianal fistulas. A systematic report can help communicate the anatomy of complex fistulising disease to assist with optimal management.










Similar content being viewed by others
References
European Society of Radiology (2018) ESR paper on structured reporting in radiology. Insights Imaging 9:1–7. https://doi.org/10.1007/s13244-017-0588-8
Poullos PD, Tseng JJ, Melcher ML, et al. (2018) Structured reporting of multiphasic CT for Hepatocellular Carcinoma: effect on Staging and Suitability for Transplant. Am J Roentgenol. 210:766–774. https://doi.org/10.2214/AJR.17.18725
Wildman-Tobriner B, Allen BC, Bashir MR, et al. (2017) Structured reporting of CT enterography for inflammatory bowel disease: effect on key feature reporting, accuracy across training levels, and subjective assessment of disease by referring physicians. Abdom Radiol (NY) 42:2243–2250. https://doi.org/10.1007/s00261-017-1136-1
Lather JD, Che Z, Saltzman B, Bieszczad J (2018) Structured Reporting in the Academic Setting: What the Referring Clinician Wants. J Am Coll Radiol . https://doi.org/10.1016/j.jacr.2017.12.031
de Miguel Criado J, del Salto LG, Rivas PF, del Hoyo LF, Velasco LG, de las Vacas MI, Marco Sanz AG, Paradela MM, Moreno EF (2012) MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics 32:175-94, https://doi.org/10.1148/rg.321115040
Tolan DJ (2016) Magnetic Resonance Imaging for Perianal Fistula. Semin Ultrasound CT MR 37:313–322. https://doi.org/10.1053/j.sult.2016.04.004
Szurowska E, Wypych J, Izycka-Swieszewska E (2007) Perianal fistulas in Crohn’s disease: mRI diagnosis and surgical planning: MRI in fistulazing perianal Crohn’s disease. Abdom Imaging 32:705–718. https://doi.org/10.1007/s00261-007-9188-2
Hellers G, Bergstrand O, Ewerth S, Holmström B (1980) Occurrence and outcome after primary treatment of anal fistulae in Crohn’s disease. Gut 21:525–527
Sheedy SP, Bruining DH, Dozois EJ, Faubion WA, Fletcher JG (2017) MR Imaging of Perianal Crohn Disease. Radiology 282:628–645. https://doi.org/10.1148/radiol.2016151491
Schwartz DA, Wiersema MJ, Dudiak KM, et al. (2001) A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn’s perianal fistulas. Gastroenterology 121:1064–1072
Beets-Tan RG, Beets GL, van der Hoop AG, et al. (2001) Preoperative MR imaging of anal fistulas: does it really help the surgeon? Radiology 218:75–84. https://doi.org/10.1148/radiology.218.1.r01dc0575
Mahjoubi B, Haizadch Kharazi H, Mirzaei R, Moghimi A, Changizi A (2006) Diagnostic accuracy of body coil MRI in describing the characteristics of perianal fistulas. Colorectal Dis 8:202–207. https://doi.org/10.1111/j.1463-1318.2005.00899.x
Singh K, Singh N, Thukral C, Singh KP, Bhalla V (2014) Magnetic resonance imaging (MRI) evaluation of perianal fistulae with surgical correlation. J Clin Diagn Res 8:RC01-4. https://doi.org/10.7860/JCDR/2014/7328.4417
Siddiqui MR, Ashrafian H, Tozer P, et al. (2012) A diagnostic accuracy meta-analysis of endoanal ultrasound and MRI for perianal fistula assessment. Dis Colon Rectum 55:576–585. https://doi.org/10.1097/DCR.0b013e318249d26c
Gustafsson UM, Kahvecioglu B, Aström G, Ahlström H, Graf W (2001) Endoanal ultrasound or magnetic resonance imaging for preoperative assessment of anal fistula: a comparative study. Colorectal Dis 3:189–197
Hori M, Oto A, Orrin S, Suzuki K, Baron RL (2009) Diffusion-weighted MRI: a new tool for the diagnosis of fistula in ano. J Magn Reson Imaging 30:1021–1026. https://doi.org/10.1002/jmri.21934
Yoshizako T, Kitagaki H (2013) A pictorial review of the impact of adding diffusion-weighted MR imaging to other MR sequences for assessment of anal fistulae. Jpn J Radiol 31:371–376. https://doi.org/10.1007/s11604-013-0204-x
Dohan A, Eveno C, Oprea R, et al. (2014) Diffusion-weighted MR imaging for the diagnosis of abscess complicating fistula-in-ano: preliminary experience. Eur Radiol 24:2906–2915. https://doi.org/10.1007/s00330-014-3302-y
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63:1–12
Marks CG, Ritchie JK (1977) Anal fistulas at St Mark’s Hospital. Br J Surg 64:84–91
Halligan S, Stoker J (2006) Imaging of fistula in ano. Radiology 239:18–33. https://doi.org/10.1148/radiol.2391041043
Morris J, Spencer JA, Ambrose NS (2000) MR imaging classification of perianal fistulas and its implications for patient management. Radiographics 20:623–635. https://doi.org/10.1148/radiographics.20.3.g00mc15623
Van Assche G, Vanbeckevoort D, Bielen D, et al. (2003) Magnetic resonance imaging of the effects of infliximab on perianal fistulizing Crohn’s disease. Am J Gastroenterol 98:332–339. https://doi.org/10.1111/j.1572-0241.2003.07241.x
Jayarajah U, Samarasekera DN (2017) Predictive accuracy of Goodsall’s rule for fistula-in-ano. Ceylon Med J 62:97–99. https://doi.org/10.4038/cmj.v62i2.8474
Beaulieu R, Bonekamp D, Sandone C, Gearhart S (2013) Fistula-in-ano: when to cut, tie, plug, or sew. J Gastrointest Surg. 17:1143–1152. https://doi.org/10.1007/s11605-012-2126-9
Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, Steele SR. Dis Colon Rectum. 59:1117–1133
Schroder O, Blumenstein I, Schulte-Bockholt A, Stein J (2004) Combining infliximab and methotrexate in fistulizing Crohn’s disease resistant or intolerant to azathioprine. Aliment Pharmacol Ther. 19:295–301
Disclosures
Each author has stated no conflicts of interest to disclose. This manuscript has not been published elsewhere and is not under consideration by another journal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thipphavong, S., Costa, A.F., Ali, H.A. et al. Structured reporting of MRI for perianal fistula. Abdom Radiol 44, 1295–1305 (2019). https://doi.org/10.1007/s00261-018-1839-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1839-y