Abstract
Purpose
To compare the accuracy of a Kinect-Optical navigation system with an electromagnetic (EM) navigation system for percutaneous liver needle intervention.
Materials and methods
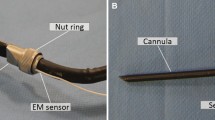
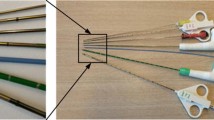
Five beagles with nine artificial tumors were used for validation. The Veran IG4 EM navigation system and a custom-made Kinect-Optical navigation system were used. Needle insertions into each tumor were conducted with these two guidance methods. The target positioning error (TPE) and the time cost of the puncture procedures were evaluated.
Results
A total of 18 needle insertions were performed to evaluate the navigation accuracy of the two guidance approaches. The targeting error was 6.78 ± 3.22 mm and 8.72 ± 3.5 mm for the Kinect-Optical navigation system and the EM navigation system, respectively. There is no statistically significant difference in the TPE between the Kinect-Optical navigation system and the EM navigation system (p = 0.229). The processing time with the Kinect-Optical system (10 min) is similar to that of the Veran IG4 system (12 min).
Conclusions
The accuracy of the Kinect-Optical navigation system is comparable to that of the EM navigation system.



Similar content being viewed by others
References
McGahan JP, Dodd GD III (2001) Radiofrequency ablation of the liver: current status. Am J Roentgenol 176(1):3–16
Goldberg SN, Grassi CJ, Cardella JF, et al. (2009) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 20(7):S377–S390
Krücker J, Xu S, Glossop N, et al. (2007) Electromagnetic tracking for thermal ablation and biopsy guidance: clinical evaluation of spatial accuracy. J Vasc Interv Radiol 18(9):1141–1150
Peters TM (2006) Image-guidance for surgical procedures. Phys Med Biol 51(14):R505
Yaniv Z, Cleary K (2006) Image-guided procedures: a review. Technical Report CAIMR TR-2006-3, Georgetown University, Washington, DC, USA
Banovac F, Tang J, Xu S, et al. (2005) Precision targeting of liver lesions using a novel electromagnetic navigation device in physiologic phantom and swine. Med Phys 32(8):2698–2705
Maier-Hein L, Tekbas A, Seitel A, et al. (2008) In vivo accuracy assessment of a needle-based navigation system for CT-guided radiofrequency ablation of the liver. Med Phys 35(12):5385–5396
Wood BJ, Zhang H, Durrani A, et al. (2005) Navigation with electromagnetic tracking for interventional radiology procedures: a feasibility study. J Vasc Interv Radiol 16(4):493–505
Banovac F, Wilson E, Zhang H, Cleary K (2006) Needle biopsy of anatomically unfavorable liver lesions with an electromagnetic navigation assist device in a computed tomography environment. J Vasc Interv Radiol 17(10):1671–1675
Yaniv Z, Cheng P, Wilson E, et al. (2010) Needle-based interventions with the image-guided surgery toolkit (IGSTK): from phantoms to clinical trials. IEEE Trans Biomed Eng 57(4):922–933
Krücker J, Xu S, Venkatesan A, et al. (2011) Clinical utility of real-time fusion guidance for biopsy and ablation. J Vasc Interv Radiol 22(4):515–524
Appelbaum L, Solbiati L, Sosna J, et al. (2013) Evaluation of an electromagnetic image-fusion navigation system for biopsy of small lesions: assessment of accuracy in an in vivo swine model. Acad Radiol 20(2):209–217
Wacker FK, Vogt S, Khamene A, et al. (2006) An augmented reality system for MR image–guided needle biopsy: initial results in a swine model. Radiology 238(2):497–504
Nicolau S, Pennec X, Soler L, et al. (2009) An augmented reality system for liver thermal ablation: design and evaluation on clinical cases. Med Image Anal 13(3):494–506
Oliveira-Santos T, Peterhans M, Hofmann S, Weber S (2011) Passive single marker tracking for organ motion and deformation detection in open liver surgery. In: Information processing in computer-assisted interventions. Springer, Berlin, pp 156–167
von Jako CR, Zuk Y, Zur O, Gilboa P (2013) A novel accurate minioptical tracking system for percutaneous needle placement. IEEE Trans Biomed Eng 60(8):2222–2225
Lin Q, Yang R, Cai K, et al. (2015) Strategy for accurate liver intervention by an optical tracking system. Biomed Opt Express 6(9):3287–3302
Bale R, Schullian P, Schmuth M, et al. (2016) Stereotactic radiofrequency ablation for metastatic melanoma to the liver. Cardiovasc Interv. Radiol 39(8):1128–1135
Mauri G, Cova L, De Beni S, et al. (2015) Real-time US-CT/MRI image fusion for guidance of thermal ablation of liver tumors undetectable with US: results in 295 cases. Cardiovasc Interv Radiol 38(1):143–151
Mauri G, De Beni S, Forzoni L, D’Onofrio S, Kolev V, Laganà M, Solbiati L (2014) Virtual navigator automatic registration technology in abdominal application. In: 2014 36th annual international conference of the IEEE engineering in medicine and biology society, 2014. IEEE, pp 5570–5574
Mauri G (2015) Expanding role of virtual navigation and fusion imaging in percutaneous biopsies and ablation. Abdom Imaging 40(8):3238–3239
Xiao D, Luo H, Jia F, et al. (2016) A Kinect camera based navigation system for percutaneous abdominal puncture. Phys Med Biol 61(15):5687–5705
Appelbaum L, Sosna J, Nissenbaum Y, Benshtein A, Goldberg SN (2011) Electromagnetic navigation system for CT-guided biopsy of small lesions. Am J Roentgenol 196(5):1194–1200
Birkfellner W, Watzinger F, Wanschitz F, Ewers R, Bergmann H (1998) Calibration of tracking systems in a surgical environment. IEEE Trans Med Imaging 17(5):737–742
Wallach D, Toporek G, Weber S, Bale R, Widmann G (2014) Comparison of freehand-navigated and aiming device-navigated targeting of liver lesions. Int J Med Robot 10(1):35–43
Hintze J (2011) PASS 11. NCSS, LLC. Kaysville. Utah, USA. www.ncss.com.
Seitel A, Bellemann N, Hafezi M, et al. (2016) Towards markerless navigation for percutaneous needle insertions. Int J Comput Assist Radiol Surg 11(1):107–117
Toporek G, Engstrand J, Nilsson H, et al. (2015) Intra-interventional image fusion and needle placement verification for percutaneous CT-guided interventions. Int J Comput Assist Radiol Surg 10(Suppl 1):S37–S38
Xia J, Siochi RA (2012) A real-time respiratory motion monitoring system using KINECT: proof of concept. Med Phys 39(5):2682–2685
Tahavori F, Alnowami M, Wells K Marker-less respiratory motion modeling using the Microsoft Kinect for Windows. In: SPIE Medical imaging, 2014. International Society for Optics and Photonics, pp 90360 K–90310 K
Yue J, Sun X, Cai J, et al. (2012) Lipiodol: a potential direct surrogate for cone-beam computed tomography image guidance in radiotherapy of liver tumor. Int J Radiat Oncol Biol Phys 82(2):834–841
Tsuchida M, Yamato Y, Aoki T, et al. (1999) CT-guided agar marking for localization of nonpalpable peripheral pulmonary lesions. Chest 116(1):139–143
Sainani NI, Arellano RS, Shyn PB, et al. (2013) The challenging image-guided abdominal mass biopsy: established and emerging techniques ‘if you can see it, you can biopsy it’. Abdom Imaging 38(4):672–696
Mauri G, Porazzi E, Cova L, et al. (2014) Intraprocedural contrast-enhanced ultrasound (CEUS) in liver percutaneous radiofrequency ablation: clinical impact and health technology assessment. Insights Imaging 5(2):209–216
Mauri G, Cova L, Ierace T, et al. (2016) Treatment of metastatic lymph nodes in the neck from papillary thyroid carcinoma with percutaneous laser ablation. Cardiovasc Interv Radiol 39(7):1023–1030
Shyn P, Tatli S, Sahni V, et al. (2014) PET/CT-guided percutaneous liver mass biopsies and ablations: targeting accuracy of a single 20 s breath-hold PET acquisition. Clin Radiol 69(4):410–415
Acknowledgements
We thank Dr. Gregory C Sharp for language improvement.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported by the following grants: National Key Research and Development Program (No. 2016YFC0106502), NSFC-GD Union Foundation (No. U1401254), NSFC-Shenzhen Union Foundation (No. U1613221), Guangdong Provincial Key Science and Technology Program (No. 2015B020214005), Guangdong Science and Technology Program (No. 2013B010404028), Shenzhen Key Science and Technology Development Program (No. JCYJ20140509174140681, JCCJY20140415162543027, JCYJ20150630114942306, and CXZZ20150430161339354).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable institutional and/or national guidelines for the care and use of animals were followed.
Informed consent
Statement of informed consent was not applicable since the manuscript does not contain any patient data.
Rights and permissions
About this article
Cite this article
Xiao, D., Li, Y., Luo, H. et al. In vivo comparison of two navigation systems for abdominal percutaneous needle intervention. Abdom Radiol 42, 1993–2000 (2017). https://doi.org/10.1007/s00261-017-1083-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1083-x