Abstract
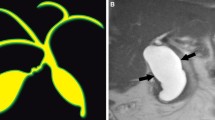
Pediatric gallbladder and bile duct disease encompasses a broad spectrum of processes, from congenital to developmental to neoplastic. We describe normal pediatric biliary anatomy and summarize the most common pathologic entities, with a focus on non-invasive imaging techniques and findings. Ultrasound is the first-line imaging modality in children with suspected biliary pathology based on its widespread availability, cost effectiveness, and lack of ionizing radiation. MRI and MRCP are often used for further evaluation in cases of diagnostic uncertainty and for surgical planning.













Similar content being viewed by others
References
Siegel MJ (2011) Pediatric Sonography, 4th edn. Philadelphia: Wolters Kluwer, Lippincott Williams & Wilkins
Yeh BM, et al. (2009) MR imaging and CT of the biliary tract. Radiographics 29(6):1669–1688
Seale MK, et al. (2009) Hepatobiliary-specific MR contrast agents: Role in imaging the liver and biliary tree. Radiographics 29(6):1725–1748
Griffin N, Charles-Edwards G, Grant LA (2012) Magnetic resonance cholangiopancreatography: The ABC of MRCP. Insights Imaging 3(1):11–21
McGahan JP, Phillips HE, Cox KL (1982) Sonography of the normal pediatric gallbladder and biliary tract. Radiology 144(4):873–875
Patriquin HB, DiPietro M, et al. (1983) Sonography of thickened gallbladder wall: Causes in children. Am J Roentgenol 141(1):57–60
Toppet V, et al. (1990) Lymph node enlargement as a sign of acute hepatitis A in children. Pediatr Radiol 20(4):249–252
Gwal K, et al. (2015) Reference values of MRI measurements of the common bile duct and pancreatic duct in children. Pediatr Radiol 45(8):1153–1159
Goh YM, et al. (2015) A case report of duplex gallbladder and review of the literature. Int J Surg Case Rep 14:179–181
Kinoshita LL, et al. (2002) Sonographic detection of gallbladder duplication: Two cases discovered in utero. J Ultrasound Med 21(12):1417–1421
Menon P, et al. (2013) Duplicated gall bladder with duodenal duplication cyst. J Pediatr Surg 48(4):e25–e28
Botsford A, et al. (2015) MRCP imaging of duplicate gallbladder: A case report and review of the literature. Surg Radiol Anat 37(5):425–429
Moyer V, Freese DK, et al. (2004) Guideline for the evaluation of cholestatic jaundice in infants: Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 39(2):115–128
Nicholas J (2015) Diseases of the Pediatric Gallbladder and Biliary Tract, in Textbook of Gastrointestinal Radiology. M.S.L. Richard M. Gore (ed.). Philadelphia: Elsevier, Saunders, pp 2180–2199
Balestreri W (1985) Neonatal cholestasis. J Pediatr Gastroenterol Nutr 106:171–184
Ikeda S, Sera Y, Oshiro H, et al. (1998) Gallbladder contraction in biliary atresia: A pitfall of ultrasound diagnosis. Pediatr Radiol 28:451–453
Kendrick APT, Phua KB, Ooi BC, et al. (2000) Making the diagnosis of biliary atresia using the triangular cord sign and gallbladder length. Pediatr Radiol 30:69–73
Kendrick APT, Phua KB, Ooi BC, Tan CE (2003) Biliary atresia: Making the diagnosis by the gallbladder ghost triad. Pediatr Radiol 33:311–315
McIlhenny J, Campbell S, Raible RJ, Antaki GM (1996) Pediatric case of the day. Biliary atresia and polysplenia syndrome. Am J Roentgenol 167: 269, 271–273.
Baumann U, Ure B (2012) Biliary atresia. Clin Res Hepatol Gastroenterol 36:257–259
Ohi RK, Kasai M, Takahashi T (1969) Intrahepatic biliary obstruction in congenital bile duct atresia. Tohoku J Exp Med 99:129–149
Superina R, et al. (2011) The anatomic pattern of biliary atresia identified at time of Kasai hepatoportoenterostomy and early postoperative clearance of jaundice are significant predictors of transplant-free survival. Ann Surg 254(4):577
Park WH, et al. (1997) A new diagnostic approach to biliary atresia with emphasis on the ultrasonographic triangular cord sign: Comparison of ultrasonography, hepatobiliary scintigraphy, and liver needle biopsy in the evaluation of infantile cholestasis. J Pediatr Surg 32(11):1555–1559
Haber BA, Russo P (2003) Biliary atresia. Gastroenterol Clin North Am 32(3):891–911
Schwarz KB, et al. (2013) Extrahepatic anomalies in infants with biliary atresia: Results of a large prospective North American multicenter study. Hepatology 58(5):1724–1731
Shneider BL, et al. (2006) A multicenter study of the outcome of biliary atresia in the United States, 1997 to 2000. J Pediatr 148(4):467–474
Davenport M, et al. (1993) Biliary atresia splenic malformation syndrome: An etiologic and prognostic subgroup. Surgery 113(6):662–668
Mirza B, Iqbal S, Sheikh A (2012) Biliary atresia associated with polysplenia syndrome, situs inversus abdominus, and reverse rotation of intestine. APSP J Case Rep 3(2):14
Bennion RS, Thompson JE, Tompkins RK (1988) Agenesis of the gallbladder without extrahepatic biliary atresia. Arch Surg 123(10):1257–1260
De Matos V, et al. (2005) Does” Cystic” Biliary Atresia Represent a Distinct Clinical and Etiological Subgroup? A Series of Three Cases. Pediatr Dev Pathol 8(6):725–731
Muise AM, et al. (2006) Biliary atresia with choledochal cyst: Implications for classification. Clin Gastroenterol Hepatol 4(11):1411–1414
Moreira RK, et al. (2012) Biliary atresia: A multidisciplinary approach to diagnosis and management. Arch Pathol Lab Med 136(7):746–760
Dolgin SE (2004) Answered and unanswered controversies in the surgical management of extra hepatic biliary atresia. Pediatr Transplant 8(6):628–631
Davenport M, et al. (2003) The spectrum of surgical jaundice in infancy. J Pediatr Surg 38(10):1471–1479
Kasai M, Ohi R (1983) Long-term follow-up results of patients with biliary atresia. Ind J Pediatr 50(2):209–217
Ibrahim M, et al. (1997) Japanese Biliary Atresia Registry, 1989 to 1994. Tohoku J Exp Med 181(1):85–95
Davenport M, et al. (2004) Seamless management of biliary atresia in England and Wales (1999–2002). Lancet 363(9418):1354–1357
Wu ET, et al. (2001) Bacterial cholangitis in patients with biliary atresia: Impact on short-term outcome. Pediatr Surg Int 17(5–6):390–395
Kendrick APT, et al. (2000) Making the diagnosis of biliary atresia using the triangular cord sign and gallbladder length. Pediatr Radiol 30(2):69–73
Kendrick APAT, et al. (2003) Biliary atresia: Making the diagnosis by the gallbladder ghost triad. Pediatr Radiol 33(5):311–315
Kim MJ, et al. (2000) Biliary Atresia in Neonates and Infants: Triangular Area of High Signal Intensity in the Porta Hepatis at T2-weighted MR Cholangiography with US and Histopathologic Correlation 1. Radiology 215(2):395–401
Lee HJ, et al. (2003) Objective criteria of triangular cord sign in biliary atresia on US scans. Radiology 229(2):395–400
Kim WS, et al. (2007) Hepatic arterial diameter measured with US: Adjunct for US diagnosis of biliary atresia. Radiology 245(2):549–555
Treves ST (2007) Pediatric nuclear medicine/PET, 3rd edn. New York: Springer
Tulchinsky M (2010) The SNM practice guideline on hepatobiliary scintigraphy. J Nucl Med 51(12):1825
Jaw TS, et al. (1999) MR cholangiography in the evaluation of neonatal cholestasis. Radiology 212(1):249–256
Han SJ, et al. (2002) Magnetic resonance cholangiography for the diagnosis of biliary atresia. J Pediatr Surg 37(4):599–604
Guibaud L, et al. (1998) MR cholangiography in neonates and infants: Feasibility and preliminary applications. AJR Am J Roentgenol 170(1):27–31
Norton KI, et al. (2002) MR Cholangiography in the Evaluation of Neonatal Cholestasis: Initial Results 1. Radiology 222(3):687–691
Courtier JL, et al. (2012) Targeted MRI contrast agents for pediatric hepatobiliary disease. J Pediatr Gastroenterol Nutr 54(4):454–462
Alagille D, et al. (1987) Syndromic paucity of interlobular bile ducts (Alagille syndrome or arteriohepatic dysplasia): Review of 80 cases. J Pediatr 110(2):195–200
Alagille D, et al. (1975) Hepatic ductular hypoplasia associated with characteristic facies, vertebral malformations, retarded physical, mental, and sexual development, and cardiac murmur. J Pediatr 86(1):63–71
Lykavieris P (2001) Outcome of liver disease in children with Alagille syndrome: A study of 163 patients. Gut 49(3):431–435
Kamath BM, et al. (2004) Vascular anomalies in Alagille syndrome a significant cause of morbidity and mortality. Circulation 109(11):1354–1358
Perrault J (1981) Paucity of interlobular bile ducts: Getting to know it better. Dig Dis Sci 26(6):481–484
Tajima T, et al. (2001) Hepatic nodular hyperplasia in a boy with Alagille syndrome: CT and MR appearances. Pediatr Radiol 31(8):584–588
Santiago I, et al. (2012) Congenital cystic lesions of the biliary tree. AJR Am J Roentgenol 198(4):825–835
Soares KC, et al. (2014) Choledochal cysts: Presentation, clinical differentiation, and management. J Am Coll Surg 219(6):1167–1180
Huang CS, Huang CC, Chen DF (2010) Choledochal cysts: Differences between pediatric and adult patients. J Gastrointest Surg 14(7):1105–1110
Sato M, et al. (2001) Choledochal cyst due to anomalous pancreatobiliary junction in the adult: Sonographic findings. Abdom Imaging 26(4):395–400
Lee HK, et al. (2009) Imaging features of adult choledochal cysts: A pictorial review. Korean J Radiol 10(1):71–80
Wiseman K, et al. (2005) Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg 189(5):527–531 (discussion 531)
Lewis VA, et al. (2015) Imaging of choledochal cysts. Abdom Imaging 40(6):1567–1580
Shi LB, et al. (2001) Diagnosis and treatment of congenital choledochal cyst: 20 years’ experience in China. World J Gastroenterol 7(5):732–734
Komi N, et al. (1977) Congenital dilatation of the biliary tract; new classification and study with particular reference to anomalous arrangement of the pancreaticobiliary ducts. Gastroenterol Jpn 12(4):293–304
Nagi B, et al. (2003) Endoscopic retrograde cholangiopancreatography in the evaluation of anomalous junction of the pancreaticobiliary duct and related disorders. Abdom Imaging 28(6):847–852
Iwai N, et al. (1992) Congenital choledochal dilatation with emphasis on pathophysiology of the biliary tract. Ann Surg 215(1):27–30
Miyano T, Yamataka A (1997) Choledochal cysts. Curr Opin Pediatr 9(3):283–288
Edil BH, Olino K, Cameron JL (2009) The current management of choledochal cysts. Adv Surg 43:221–232
Todani T, et al. (2003) Classification of congenital biliary cystic disease: Special reference to type Ic and IVA cysts with primary ductal stricture. J Hepatobiliary Pancreat Surg 10(5):340–344
Alonso-Lej F, Rever WB Jr, Pessagno DJ (1959) Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg 108(1):1–30
Todani T, et al. (1977) Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 134(2):263–269
Michaelides M, et al. (2011) A new variant of Todani type I choledochal cyst. Imaging evaluation. Hippokratia 15(2):174–177
Ziegler KM, et al. (2010) Choledochoceles: Are they choledochal cysts? Ann Surg 252(4):683–690
Lipsett PA, et al. (1994) Choledochal cyst disease. A changing pattern of presentation. Ann Surg 220(5):644–652
Nicholl M, et al. (2004) Choledochal cysts in western adults: Complexities compared to children. J Gastrointest Surg 8(3):245–252
Shah OJ, et al. (2009) Choledochal cysts in children and adults with contrasting profiles: 11-year experience at a tertiary care center in Kashmir. World J Surg 33(11):2403–2411
Egbert ND, Bloom DA, Dillman JR (2013) Magnetic resonance imaging of the pediatric pancreaticobiliary system. Magn Reson Imaging Clin N Am 21(4):681–696
Lam WW, et al. (1999) MR cholangiography and CT cholangiography of pediatric patients with choledochal cysts. AJR Am J Roentgenol 173(2):401–405
Nicholas J (2014) Textbook of gastrointestinal radiology: Diseases of the pediatric gallbladder and biliary tract. Amsterdam: Elsevier Health Sciences
Todani T, et al. (1995) Characteristics of choledochal cysts in neonates and early infants. Eur J Pediatr Surg 5(3):143–145
Johnson K, Alton HM, Chapman S (1998) Evaluation of mebrofenin hepatoscintigraphy in neonatal-onset jaundice. Pediatr Radiol 28(12):937–941
Park DH, et al. (2005) Can MRCP replace the diagnostic role of ERCP for patients with choledochal cysts? Gastrointest Endosc 62(3):360–366
Sacher VY, et al. (2013) Role of magnetic resonance cholangiopancreatography in diagnosing choledochal cysts: Case series and review. World J Radiol 5(8):304–312
Rozel C, et al. (2011) Imaging of biliary disorders in children. Pediatr Radiol 41(2):208–220
Watts DR, Lorenzo GA, Beal JM (1974) Proceedings: Congenital dilatation of the intrahepatic biliary ducts. Arch Surg 108(4):592–598
Cha SW, et al. (2008) Choledochal cyst and anomalous pancreaticobiliary ductal union in adults: Radiological spectrum and complications. J Comput Assist Tomogr 32(1):17–22
Torra R, et al. (1997) Autosomal dominant polycystic kidney disease with anticipation and Caroli’s disease associated with a PKD1 mutation. Rapid communication. Kidney Int 52(1):33–38
Parada LA, et al. (1999) Clonal chromosomal abnormalities in congenital bile duct dilatation (Caroli’s disease). Gut 45(5):780–782
Zhang DY, et al. (2012) Caroli’s disease: A report of 14 patients and review of the literature. J Dig Dis 13(9):491–495
Venkatanarasimha N, et al. (2011) Imaging features of ductal plate malformations in adults. Clin Radiol 66(11):1086–1093
Marchal GJ, et al. (1986) Caroli disease: High-frequency US and pathologic findings. Radiology 158(2):507–511
Miller WJ, et al. (1995) Imaging findings in Caroli’s disease. AJR Am J Roentgenol 165(2):333–337
Dayton MT, Longmire WP Jr, Tompkins RK (1983) Caroli’s Disease: A premalignant condition? Am J Surg 145(1):41–48
Stringer MD, Lim P, Cave M, Martinez D, Lilford RJ (1996) Fetal gallstones. J Pediatr Surg 31(11):1589–1591
Mehta S, et al. (2012) Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics 129(1):e82–e88
Coley BD (2016) Caffey’s pediatric diagnostic imaging, 12th edn. Philadelphia: Elsevier Saunders
Brill PW, Winchester P, Rosen MS (1982) Neonatal cholelithiasis. Pediatr Radiol 12(6):285–288
Matos C, Avni EF, et al. (1987) Total parenteral nutrition (TPN) and gallbladder diseases in neonates. Sonographic assessment. J Ultrasound Med 6(5):243–248
Svensson J, Makin E (2012) Gallstone disease in children. Semin Pediatr Surg 21(3):255–265
Vrochides DV (2005) Is there a role for routine preoperative endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in children? Arch Surg 140(4):359–361
Kim TK, et al. (2002) Diagnosis of intrahepatic stones: Superiority of MR cholangiopancreatography over endoscopic retrograde cholangiopancreatography. Am J Roentgenol 179(2):429–434
Gunnarsdottir A, et al. (2008) Laparoscopic aided cholecystostomy as a treatment of inspissated bile syndrome. J Pediatr Surg 43(4):e33–e35
Davenport M, et al. (2003) The spectrum of surgical jaundice in infancy. J Pediatr Surg 38(10):1471–1479
Berrani H, et al. (2015) Association of N-acetylcysteine and glucagon during percutaneous cholangiography in the treatment of inspissated bile syndrome. Arch Pediatr 22(3):300–302
Miloh T, et al. (2009) Inspissated bile syndrome in a neonate treated with cefotaxime: Sonographic aid to diagnosis, management, and follow-up. J Ultrasound Med 28(4):541–544
King LJ, et al. (2000) Hepatobiliary and pancreatic manifestations of cystic fibrosis: MR imaging appearances. Radiographics 20(3):767–777
Ruzal-Shapiro C (1998) Cystic fibrosis: An overview. Radiol Clin North Am 36(1):143–161
Akata D, Akhan O (2007) Liver manifestations of cystic fibrosis. Eur J Radiol 61(1):11–17
Mieli-Vergani G, Vergani D (2016) Sclerosing cholangitis in children and adolescents. Clin Liver Dis 20(1):99–111
Deneau M, et al. (2013) Primary sclerosing cholangitis, autoimmune hepatitis, and overlap in Utah children: Epidemiology and natural history. Hepatology 58(4):1392–1400
Gregorio GV, et al. (2001) Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: A 16-year prospective study. Hepatology 33(3):544–553
Debray D, et al. (1994) Sclerosing cholangitis in children. J Pediatr 124(1):49–56
Wilschanski M, et al. (1995) Primary sclerosing cholangitis in 32 children: Clinical, laboratory, and radiographic features, with survival analysis. Hepatology 22(5):1415–1422
Feldstein AE, et al. (2003) Primary sclerosing cholangitis in children: A long-term follow-up study. Hepatology 38(1):210–217
Miloh T, et al. (2009) A retrospective single-center review of primary sclerosing cholangitis in children. Clin Gastroenterol Hepatol 7(2):239–245
Chavhan GB, et al. (2008) Primary sclerosing cholangitis in children: Utility of magnetic resonance cholangiopancreatography. Pediatr Radiol 38(8):868–873
Rossi G, et al. (2013) Diagnosis of sclerosing cholangitis in children: Blinded, comparative study of magnetic resonance versus endoscopic cholangiography. Clin Res Hepatol Gastroenterol 37(6):596–601
Ibrahim SH, Lindor KD (2011) Current management of primary sclerosing cholangitis in pediatric patients. Paediatr Drugs 13(2):87–95
Mitchell SA, et al. (2001) A preliminary trial of high-dose ursodeoxycholic acid in primary sclerosing cholangitis. Gastroenterology 121(4):900–907
Ross AM, Anupindi SA, Balis UJ (2003) Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 11-2003. A 14-year-old boy with ulcerative colitis, primary sclerosing cholangitis, and partial duodenal obstruction. N Engl J Med 348(15):1464–1476
Pieringer H, et al. (2014) IgG4- related disease: An orphan disease with many faces. Orphanet J Rare Dis 9:110
Zen Y, et al. (2007) Pathological classification of hepatic inflammatory pseudotumor with respect to IgG4-related disease. Modern Pathol 20(8):884–894
Donnelly LF, et al. (1998) Diagnosis please. Case 2: Embryonal rhabdomyosarcoma of the biliary tree. Radiology 208(3):621–623
Caty MG, Oldham KT, Prochownik EV (1990) Embryonal rhabdomyosarcoma of the ampulla of Vater with long-term survival following pancreaticoduodenectomy. J Pediatr Surg 25(12):1256–1258
Raney RBJr, et al. (1985) Rhabdomyosarcoma of the biliary tree in childhood. A report from the Intergroup Rhabdomyosarcoma Study. Cancer 56(3):575–581
Brugières L, Branchereau S, Laithier V (2012) Paediatric malignant liver tumours. B Cancer 99(2):219–228
Pietsch JB, et al. (2001) Obstructive jaundice secondary to lymphoma in childhood. J Pediatr Surg 36(12):1792–1795
Arenas GB (2006) Primary pancreatic lymphoma in pediatric patients. Radiologia 49(2):125–127
Arellano CMR, Kritsaneepaiboon S, Lee EY (2011) CT Imaging findings of malignant neoplasms arising in the epigastric region in children. Clin Imaging 35(1):10–20
Acknowledgments
The authors would like to thank the following individuals for assisting in the collection of images for this article: Melissa Semp, APN – Division of Gastroenterology, Hepatology, & Nutrition; Ann & Robert H. Lurie Children’s Hospital of Chicago. Kelsey Stoller, PNP – Division of Gastroenterology, Hepatology, & Nutrition; Ann & Robert H. Lurie Children’s Hospital of Chicago. Joan Lokar, APN, NP – Transplant Surgery; Ann & Robert H. Lurie Children’s Hospital of Chicago. Susan Kelly, RN – Research Coordinator; Division of Gastroenterology, Hepatology, & Nutrition; Ann & Robert H. Lurie Children’s Hospital of Chicago.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
IRB approval
Not applicable.
Rights and permissions
About this article
Cite this article
Sharafinski, M.E., Meyers, A.B. & Vorona, G. Pediatric cholangiopathies: diseases of the gallbladder and biliary tract. Abdom Radiol 42, 69–85 (2017). https://doi.org/10.1007/s00261-016-0865-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0865-x