Abstract
Purpose
We sought to assess the impact of coronary revascularization on myocardial perfusion and fractional flow reserve (FFR) in patients without a cardiac history, with prior myocardial infarction (MI) or non-MI percutaneous coronary intervention (PCI). Furthermore, we studied the impact of scar tissue.
Methods
Symptomatic patients underwent [15O]H2O positron emission tomography (PET) and FFR before and after revascularization. Patients with prior CAD, defined as prior MI or PCI, underwent scar quantification by magnetic resonance imaging late gadolinium enhancement.
Results
Among 137 patients (87% male, age 62.2 ± 9.5 years) 84 (61%) had a prior MI or PCI. The increase in FFR and hyperemic myocardial blood flow (hMBF) was less in patients with prior MI or non-MI PCI compared to those without a cardiac history (FFR: 0.23 ± 0.14 vs. 0.20 ± 0.12 vs. 0.31 ± 0.18, p = 0.02; hMBF: 0.54 ± 0.75 vs. 0.62 ± 0.97 vs. 0.91 ± 0.96 ml/min/g, p = 0.04). Post-revascularization FFR and hMBF were similar across patients without a cardiac history or with prior MI or non-MI PCI. An increase in FFR was strongly associated to hMBF increase in patients without a cardiac history or with prior MI/non-MI PCI (r = 0.60 and r = 0.60, p < 0.01 for both). Similar results were found for coronary flow reserve. In patients with prior MI scar was negatively correlated to hMBF increase and independently predictive of an attenuated CFR increase.
Conclusions
Post revascularization FFR and perfusion were similar among patients without a cardiac history, with prior MI or non-MI PCI. In patients with prior MI scar burden was associated to an attenuated perfusion increase.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current revascularization strategies for patients with chronic coronary syndrome are aimed at detecting ischemia-causing coronary stenoses, restoration of myocardial perfusion by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) and, subsequently, relief of symptoms [1]. To maximize the effect of revascularization therapy, guidelines recommend to assess the presence of inducible ischemia beforehand [1]. Fractional flow reserve (FFR) is an important vessel-specific tool to assess myocardial ischaemia and since post-procedural FFR and myocardial blood flow (MBF) have been linked to superior outcomes, the use of FFR and MBF has been extended to a post-revascularization tool [2, 3]. A previous study by Driessen et al. included patients without prior myocardial infarction (MI) or PCI and showed that an increase in FFR was paralleled by improvement of hyperemic MBF with a strong correlation between these two indices (r = 0.74) [4]. However, the relationship between FFR and absolute myocardial perfusion is not only determined by epicardial coronary stenoses, but also by microvascular resistance and the subtended myocardial mass. As such, a supposedly increase in FFR is not necessarily commensurate with an equivalent increase in hyperemic blood flow (hMBF). Microvascular disease is encountered in up to 50% of patients with prior infarction and the revascularization benefit in terms of perfusion increase and as such symptom reduction has been questioned in this group of patients [5]. Remarkably, data on the restoration of myocardial blood flow after revascularization therapy in patients with prior MI or PCI is lacking. As such, we investigated the influence of revascularization on FFR and absolute myocardial perfusion in patients without a cardiac history, with prior MI or non-MI PCI using serial FFR and positron emission tomography (PET) MBF measurements. Furthermore, we investigated whether the restoration of myocardial perfusion is attenuated by scar tissue burden or conventional risk factors.
Methods
Patient selection
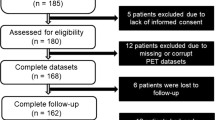
This is a sub study of the Comparison of Coronary CT Angiography, SPECT, PET, and Hybrid Imaging for Diagnosis of Ischemic Heart Disease Determined by Fractional Flow Reserve (PACIFIC 1) and Functional stress imaging to predict abnormal coronary fractional flow reserve: the PACIFIC 2 study (PACIFIC 2), which were prospective clinical single-centre, head-to-head comparative studies conducted from 2012 to 2020, at the Amsterdam UMC, VU University Medical Centers, Amsterdam, the Netherlands [6, 7]. All patients were suspected of having stable obstructive coronary artery disease (CAD), were referred for a clinically indicated diagnostic ICA, and underwent a 2-week protocol in which patients underwent [15O]H2O PET prior to invasive coronary angiography (ICA) with routine 3 vessel invasive FFR interrogation. Patients suspected for acute coronary syndrome were not included. Additionally, patients with a cardiac history, defined as prior MI or PCI, underwent cardiac magnetic resonance (CMR) imaging with late gadolinium enhancement (LGE) prior to invasive coronary angiography (ICA). This PACIFIC post-hoc analysis included patients in whom FFR interrogation or [15O]H2O PET perfusion imaging was repeated after coronary revascularization (PCI or CABG). Patients with events between revascularization and follow-up PET (n = 1) were excluded. The study complied with the Declaration of Helsinki. The study protocol was approved by the VUmc Medical Ethics Review Committee and all patients provided written informed consent.
PET
The PET scans were performed on a hybrid PET/CT device (Philips Gemini TF 64 or Ingenuity TF 128, Philips Healthcare, Best, The Netherlands). A 6-min dynamic scan protocol commencing simultaneously with an injection of 370 MBq [15O]H2O during resting and adenosine (140 µg/kg/min) induced hyperemic conditions. The dynamic scan sequence was followed by a low-dose CT-scan for attenuation correction. Parametric images of quantitative hyperemic MBF in ml/min/g were generated by in-house developed software (CardiacVUer, Amsterdam UMC, Vrije Universiteit Amsterdam, The Netherlands) [8] for each of the 17 left ventricle segments according to the standard American Heart Association model with standardized allocation of segments to the three vascular territories [9]. Patients were instructed to refrain from the intake of xanthine or caffeine 24 h prior to the PET. Parametric MBF images were analyzed. Regional hMBF was defined as mean hMBF of the entire vascular territory in the absence of a perfusion defect or as the mean hMBF of the perfusion defect (≥ 2 adjacent segments with a hMBF ≤ 2.3 ml/min/g) when present [10]. In the presence of an inferior perfusion defect the invasive angiography was used to determine coronary dominance and the perfusion defect was allocated accordingly. Regional hMBF of the predefined vascular territories was used for analysis.
CMR
Images were acquired on a 1.5-T whole body MR scanner (Magnetom Avanto, Siemens Healthineers). Left ventricular (LV) cardiac function was assessed in between stress and rest perfusion with steady-state free-precession cine imaging in the 2-, 3-, 4-chamber long-axis views and multiple short-axis views covering the LV from base to apex. Late gadolinium enhancement (LGE) was performed using a 2-dimensional segmented inversion-recovery gradient-echo pulse sequence. If LGE was considered visually present, total and segmental infarct size (in grams) was calculated from the LGE images using the full width at half maximum method [11]. Infarct mass was also expressed as a percentage of myocardial mass per segment according to the AHA 17-segment model excluding the apex [9]. Additionally, in accordance with the AHA model, infarct size and percentage for each vascular territory was calculated. The segments used for PET were also used for scar analysis. LGE analysis was performed using Circle CVI42 (version 5.13, Circle Cardiovascular Imaging, Inc, Calgary, Canada) by a researcher blinded to clinical characteristics.
ICA and FFR
ICA was performed according to standard clinical protocols [6]. Patients were instructed to refrain from the intake of xanthine or caffeine 24 h prior to the ICA. All major coronary arteries were routinely interrogated by FFR irrespective of stenosis severity and imaging results, except for occluded vessels or subtotal lesions with a diameter stenosis (DS) ≥ 90%. To induce maximal coronary hyperemia, adenosine was administered intracoronary as a 150 μg bolus. FFR was calculated as the ratio of mean distal intracoronary to aortic guiding pressure during hyperemia. The type of treatment (PCI, CABG or conservative) was left to the discretion of the operator and the heart team after consideration of symptoms, FFR and angiographic results. In case of PCI, post-procedural FFR was measured at the same location as the pre-PCI FFR. To evaluate the extent and diffuseness of atherosclerotic disease segment involvement scores were calculated according to Min et al., which is the sum of the number of segments with plaque irrespective of the degree of luminal stenosis [12].
Statistical analysis
Continuous variables are expressed as mean ± SD or median (interquartile range) where appropriate. Categorical variables are presented as frequencies with percentages. Baseline characteristics between two groups were compared by the independent sample's T-test for continuous variables and the chi-square test for categorical variables. The correlation between two variables (FFR, hMBF, CFR or scar) was analyzed using Pearson’s correlation analysis. Paired FFR and regional perfusion measurements (before and after revascularization) were compared by the paired samples T-test. Regional perfusion and FFR analyses were stratified for patients without prior CAD, with prior MI or with a non-MI PCI. Patients with both a prior MI and with a non-MI PCI were grouped as prior MI. The change in FFR and perfusion was compared between these groups using an one way analysis of variance (ANOVA). In case the overall F-test for the ANOVA was significant, posthoc pairwise comparisons between patient categories were performed with Bonferroni correction for multiple comparisons. To analyze the importance of baseline FFR a sensitivity analysis stratified for vessels with FFR greater or less than 0.75 was performed. To identify predictors of regional perfusion improvement an analyses with regionally matched scar was performed using a mixed models with a random effect for subjects. Significant (p < 0.15) variables in the univariable analysis were included in the multivariable model. A two-sided P value < 0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS software package version 26 (IBM SPSS Statistics, IBM Corporation, Armonk, NY).
Results
The study population consisted of 137 patients with 200 revascularized vessels. The mean age was 62.2 ± 9.5 years and 119 were male (86.9%). A total of 84 patients (61.3%) had a history of myocardial infarction or PCI. Patients were revascularized by PCI (n = 116, 84.7%) or CABG (n = 21, 15.3%). Further patient baseline characteristics are shown in Table 1. Vessel specific characteristics are shown in Table 2. In general, patients with prior MI or non-MI PCI had a more extensive cardiovascular risk profile. The median interval between revascularization and post revascularization PET was 34 days (interquartile range 21 to 58 days). Detailed flow charts describing PET and FFR availability are shown in supplemental Figs. 1, 2 and 3. Serial FFR measurements were available in 94 (47%) of the revascularized vessels, whereas paired hMBF and CFR measurements were available in 189 (95%) and 184 (92%) of the revascularized myocardial territories (supplemental Fig. 3). Baseline and post revascularization regional perfusion indices and FFR (including rest MBF) are depicted in Table 3 and supplemental Table 1.
Case examples showing the effect of revascularization on FFR and perfusion in patients with and without a prior cardiac history. Abbreviations: FFR, fractional flow reserve; LAD, left anterior descending artery; LGE, late gadolinium enhancement; PET, positron emission tomography; RCA, right coronary artery
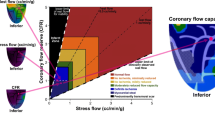
Change of regional perfusion and FFR after revascularization. Mean ± SD are displayed. Only revascularized vessels with measurements before and after revascularization were included for this sub analysis. Abbreviations: CAD, coronary artery disease; CFR, coronary flow reserve; FFR, fractional flower reserve; hMBF, hyperemic myocardial blood flow; MI, myocardial infarction; PCI, percutaneous coronary intervention
Change of perfusion and FFR after revascularization
Figure 1 exemplifies the study protocol by showing two case examples and their respective serial PET perfusion scans, ICA and CMR images. After revascularization mean FFR increased from 0.65 ± 0.15 to 0.90 ± 0.08 (p < 0.01, Fig. 2). An increase in FFR was observed for patients without a cardiac history, with prior MI or with non-MI PCI. However, it may be appreciated from Fig. 3 that FFR increased to a lesser degree in patients with a prior non-MI PCI compared to those without a prior history (∆ FFR 0.20 ± 0.12 vs. 0.31, p = 0.02). Regional hyperemic MBF and CFR improved after revascularization (hMBF: 1.73 ± 0.75 to 2.47 ± 0.88 ml/min/g; CFR: 2.08 ± 0.80 to 2.85 ± 0.96, p < 0.01 for both, Fig. 2). Similar to FFR, Fig. 3 shows a trend of an attenuated regional hMBF increase in patients with a prior MI or non-MI PCI (p = 0.04, p = ns for subgroup differences). CFR increase after revascularization did not significantly differ between patients with or without a prior cardiac history (p = 0.23). Baseline FFR and hMBF were significantly lower in patients without prior CAD (p < 0.01, Table 3). Post revascularization FFR, hMBF and CFR were similar across all subgroups (p = 0.39, p = 0.68 and p = 0.49). A perfusion decrease after revascularization was seen in 37 territories (ΔhMBF: 0.36 ± 0.39 ml/min/g). Those territories were predominantly characterised by a relatively preserved hMBF at baseline (2.27 ± 0.95 vs 1.60 ± 0.64, p < 0.01) and were more prevalent in patients with prior MI or non-MI PCI (27.3% vs 11.1% of revascularized territories, p < 0.01). In a sensitivity analysis the absolute improvement in FFR and perfusion indices stratified for baseline FFR (lower or greater than 0.75) are shown in in supplemental Table 1. Patients with a FFR below 0.75 at baseline had a numerically greater FFR and perfusion improvement across all subgroups.
Relation between FFR and perfusion
At baseline, a moderate correlation was observed in patients without a cardiac history between perfusion indices (hMBF and CFR) and FFR (r = 0.59 and r = 0.56, p < 0.01 for both). A weak baseline correlation was observed between baseline FFR and perfusion in patients with prior MI or non-MI PCI (hMBF: r = 0.31; CFR r = 0.35 for patients with prior MI and hMBF: r = 0.30; CFR r = 0.22 for patients with prior non-MI PCI, p < 0.01 for all, supplemental Fig. 4). Hyperemic MBF and FFR were at baseline concordant in 72% of patients without cardiac history, whereas 58% and 57% of the measurements were concordant in patients with prior MI or non-MI PCI. Figure 4 shows the relation between % perfusion change and FFR following revascularization. The relationship between FFR and hMBF increase was strong in both patients with and without cardiac history (r = 0.60 and r = 0.60, p < 0.01 for both). The relationship between FFR and CFR was strong in patients without a cardiac history (r = 0.70, p < 0.01) and moderate (r = 0.57, p < 0.01) for patients with a cardiac history. A substantial overlap was observed between the segment involvement scores among patients without prior CAD, with prior MI or with prior non-MI PCI with more segments affected by atherosclerotic disease in patients without prior CAD than in patients with prior MI or non-MI PCI (supplemental Table 2).
Relationship between changes in FFR and perfusion. Only revascularized vessels with measurements before and after revascularization were included for this sub analysis. A cardiac history was defined as a history of PCI and/or MI. Analyses for patients with a cardiac history could not be split for prior MI/PCI since a limited amount of combined measurements was available. Abbreviations: CFR, coronary flow reserve; FFR, fractional flow reserve; hMBF, hyperemic myocardial blood flow
The influence of scar on change of FFR and perfusion
Table 2 depicts the amount of LGE per revascularized territory. Figure 5 shows the impact of regional scar tissue on restoration of regional myocardial perfusion. Increased scar was negatively associated to hMBF and CFR increase (r = -0.34, p = 0.02 and r = -0.53, p = 0.02) in patients with prior MI. In patients with non-MI PCI scar and perfusion were not related.
Relationship between scar and change in FFR and perfusion. The relation between scar and delta FFR (n = 57), delta hMBF (n = 94) and CFR (n = 92) split for patients with prior MI and prior non-MI PCI. Scar is depicted as a percentage of the revascularized segments. Abbreviations: CFR, coronary flow reserve; FFR, fractional flow reserve; hMBF, hyperemic myocardial blood flow; MI, myocardial infarction; PCI, percutaneous coronary intervention
Predictors of perfusion improvement
In a univariable analysis (supplemental Table 3) including baseline characteristics, cardiovascular risk factors, prior PCI for stable CAD in the revascularized territory, left ventricle ejection fraction and scar (as % of revascularized territory) only prior PCI for stable CAD in the revascularized territory and scar had a p < 0.15 for hMBF increase. Scar and a history of smoking were negative predictors of CFR increase. In the multivariable analysis assessing hMBF increase, none of the predictors with a univariable p-value < 0.15 were significantly associated with hMBF increase. Scar and a history of smoking were independent negative predictors of CFR increase.
Discussion
This sub study of the PACIFIC 1 and 2 assessed the potential of coronary revascularization to restore myocardial perfusion as assessed by quantitative [15O]H2O PET and is, to the best of our knowledge, the first to evaluate the effect of prior coronary revascularizations and myocardial infarctions on the improvement of absolute myocardial perfusion after revascularization. Moreover, this study provides insight into the relationship between FFR and absolute myocardial perfusion before and after revascularization. The main findings can be summarized as follows: 1) Successful coronary revascularization improved FFR and perfusion in patients without a cardiac history, with prior MI or with prior non-MI PCI 2) Post revascularization FFR and perfusion were similar in patients without a cardiac history, with prior MI or non-MI PCI 3) Changes in FFR and absolute perfusion were strongly associated 4) Regional scar and a history of smoking were independently negatively associated with CFR increase. Other cardiovascular risk factors were not independently predictive of an attenuated recovery of myocardial perfusion.
Functional treatment of CAD
Physiology-guided coronary interventions have been shown to confer prognostic benefit over a merely anatomical driven approach [13]. Germane to this, post-PCI FFR contains prognostic information and a suboptimal restoration of intracoronary pressures (i.e. FFR < 0.90) has been associated with an increased risk of adverse cardiovascular events and higher rates of target vessel revascularization [14, 15]. Therefore, FFR has been considered the reference standard for discerning the functional significance of epicardial lesions [1]. However, the question remains whether FFR and myocardial perfusion metrics are interchangeable and provide us with similar or complementary information on the CAD spectrum. Interestingly, FFR and [15O]H2O PET have a shared history. The second ever published paper on FFR was its first validation in humans in isolated LAD lesions using relative flow reserve by [15O]H2O PET as a reference standard [16]. Several studies confirmed that FFR provides an invasive measure of myocardial perfusion, although the relationship is governed by diffuse epicardial disease, and microvascular function. Contrary to the validation study of the de Bruyne et al. we included symptomatic patients and did not exclude diffusely diseased patients, which is exemplified by median segment involvement scores ≥ 4. In this regard, we found a moderate correlation between baseline FFR, hyperemic MBF and CFR in patients without a prior cardiac history, which is consistent with earlier results [17]. On the other hand, only a weak correlation was seen between baseline FFR and perfusion metrics in patients with prior MI or non-MI PCI. Patients with prior CAD had lower segment involvement scores suggesting more diffuse CAD in patients without prior CAD. The weaker baseline correlation between FFR and perfusion in patients with prior CAD may be ascribed to a higher occurrence of microvascular disease in this high-risk category. Also, the influence of plaque characteristics on FFR and perfusion cannot be neglected [18, 19]. Patients with prior CAD (I.e. prior MI or non-MI PCI) had a numerically lower FFR and perfusion increase. It should be noted that baseline perfusion and FFR of patients without prior CAD were lower but post revascularization FFR and perfusion were similar, suggesting a similar post revascularization potential. Therefore, non-invasive evaluation of myocardial perfusion by PET may play a role in identifying patients who might experience symptom reduction from revascularization therapy. Quantitative myocardial blood flow imaging is nowadays not only limited to PET MPI. There are promising results using CZT-SPECT devices. Although there are important differences in tracer kinetics, it is promising Acampa and colleagues have demonstrated the feasibility of quantifying myocardial perfusion using CZT-SPECT [20]. Furthermore, Mannarino et al. showed that vessels with > 50% diameter stenosis on invasive angiography with regional perfusions deficits showed a trend towards more vessel-specific adverse events, underlying the potential of functional imaging to guide coronary interventions and to predict revascularization related outcome [21]. Integrating anatomical and functional information offers several advantages, while independently used may lead to disregarding valuable information on important aspects of the complex interplay between anatomy and ischemia.
Notably, multiple perfusion metrics can be derived from PET. A study by Bom and colleagues demonstrated longitudinal perfusion gradients to reflect diffuse CAD, while Johnson and colleagues suggested the integration of hMBF and CFR into coronary flow capacity to more accurately identify ischemia [22]. A serial PET study by De Winter et al. revealed coronary flow at baseline to predict improvement of perfusion after revascularization therapy [23, 24]. Most probably the abovementioned perfusion metrics are complementary and should all be evaluated in symptomatic patients [25]. Further studies need to exploit these perfusion metrics to advance our understanding of the atherosclerotic spectrum and on the potential future applications of quantitative PET beyond its current role being merely a gatekeeper for the “cathlab”.
The influence of scar and risk factors on restoration of perfusion
Restoration of myocardial perfusion following revascularization is dependent on the alleviation of coronary diameter stenosis. However, myocardial blood flow is regulated by both epicardial coronary flow and microvascular resistance. Traditional risk factors have been shown to induce microvascular disease, a condition that is associated with abnormal myocardial perfusion requiring specific conservative (i.e. noninvasive) treatment [26,27,28]. Although microvascular disease represents a separate entity with unique therapeutic implications, there is a large overlap between epicardial atherosclerosis and microvascular dysfunction [29]. Residual ischemia after successful coronary revascularization could be caused by residual CAD or microvascular dysfunction. We assessed the diffuseness of atherosclerosis by calculating visual segment involvement scores. Prior studies suggested that diffuse, potentially flow-limiting, CAD could be missed by visual assessment [30]. These patients are at risk of being incorrectly classified as patients with microvascular disease, potentially attributing to a significant proportion of contemporary patients diagnosed with microvascular disease [29].
The amount of ischemia that is accounted for by diffuse CAD or microvascular disease is difficult to determine upfront and has been associated with persisting angina and even adverse outcomes. In other words, a successful stent placement is not necessarily commensurate with improved perfusion. Additionally, in a study from our institution, lower stress perfusion was seen in elderly and obese patients, despite focal obstructive CAD was excluded [31].
In the present study, of conventional risk factors only a history of smoking was predictive of perfusion increase. This may be attributed to a population with a relatively large atherosclerotic burden, an end-stage disease wherein the impact of traditional risk factors may be nullified. The vascular damage caused by traditional cardiovascular risk factors attenuates the relative contribution of these risk factors. Indeed, studies have shown that prediction models perform better in middle-aged populations than in elderly patients [32]. In addition, risk scores appear to have only a modest discriminatory power in high-risk patients with typical angina [33]. The presence and extent of regional scar in patients with a prior MI was associated to an attenuated perfusion increase and independently predictive of a attenuated CFR increase following revascularization. We found slightly stronger correlations between scar and CFR than between scar and hMBF. One explanation is that CFR incorporates rest perfusion. An increased rest perfusion is associated to MACE and related to microvascular dysfunction and epicardial coronary stenosis [34]. It bears mentioning that scar burden in our population was rather small and FFR measurements account for scarred myocardium. Territories with extensive scar will by definition have a higher FFR and will be less likely revascularized [35]. In addition, the use of a [15O]H2O perfusion tracer is less suitable for visualizing non-viable tissue since MBF is only measured in viable tissue and this may have affected the present findings. Nevertheless, scar tissue is often heterogeneous and contains islands of viable tissue, which is reflected by [15O]H2O PET as areas of abnormal perfusion. Interestingly, a recent animal study by Grönman and colleagues demonstrated resting MBF suitable for the assessment of viability with a similar diagnostic value as measures of perfusable tissue fractions and index [36]. All-in all, epicardial atherosclerosis and coronary microvascular dysfunction are two different entities of the atherosclerotic spectrum with large overlap. Non-invasive quantitative perfusion imaging combined with FFR measurements may provide a comprehensive understanding of the complex interplay between FFR, microvascular function and its impact on myocardial perfusion. We studied the influence of revascularization on perfusion and FFR restoration but had no information on the post revascularization symptomatic status. As such we could not correlate our findings with (post)revascularization symptoms. Also the numbers do not allow a prognostic analysis. However, since ischaemia testing and FFR are the backbone of the revascularization strategy we think these derivatives are of sufficient quality to provide useful information. Further studies are warranted to determine whether a combined approach of pressure and flow measures may further distinguish between patients who may benefit from revascularization and patients in whom pharmacotherapy targeting endothelial and microvascular atherosclerosis is required in terms of perfusion increase and symptom reduction.
Limitations
This is a post hoc sub analysis of two prospective studies including a modest number of patients, and some limitations should be addressed. First, although coronary dominance was checked regional perfusion as assessed by PET is matched with FFR measurements upon standardized coronary anatomy and does not account for individual variations. Second, [15O]H2O was used as tracer. The tracer has the unique ability to be linearly related to myocardial blood flow, primarily in viable myocardium [37]. Therefore the influence of nonviable tissue (i.e. scar) could be underestimated. Third, although patients with prior MI were included, regional extensive scar was scarce and results with regard to the influence of scar should be considered hypothesis-generating. This might be attributed to the excellent STEMI care in the densely populated Netherlands [38]. Fourth, segment involve scores were calculated to analyze diffuseness of atherosclerosis. Pressure pull back curves were not routinely performed during ICA. Finally, patients underwent follow-up PET after a median of 34 days. It has been reported that myocardial perfusion increases further after 1 month post revascularization. Therefore myocardial perfusion might have increased further in our patients [39, 40].
Conclusion
Successful coronary revascularization improved FFR and absolute myocardial perfusion in patients without a cardiac history, with prior MI or with prior non-MI PCI. Post revascularization FFR and perfusion were similar in patients without a cardiac history, with prior MI or non-MI PCI. An increase in FFR was paralleled by improvements in absolute perfusion. In patients with prior infarction scar burden was associated to an attenuated perfusion increase.
Data Availability
Data are available on request.
Abbreviations
- CABG:
-
Coronary artery bypass graft surgery
- CAD:
-
Coronary artery disease
- CFR:
-
Coronary flow reserve
- CMD:
-
Coronary microvascular dysfunction
- FFR:
-
Fractional flow reserve
- ICA:
-
Invasive coronary angiography
- LGE:
-
Late gadolinium enhancement
- hMBF:
-
Hyperemic myocardial blood flow
- MI:
-
Myocardial infarction
- CMR:
-
Cardiac magnetic resonance
- PCI:
-
Percutaneous coronary intervention
- PET:
-
Positron emission tomography
References
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407–77.
Pijls NH, Klauss V, Siebert U, Powers E, Takazawa K, Fearon WF, et al. Coronary pressure measurement after stenting predicts adverse events at follow-up: a multicenter registry. Circulation. 2002;105(25):2950–4.
Hori Y, Yoda S, Nakanishi K, Tano A, Suzuki Y, Matsumoto N, et al. Myocardial ischemic reduction evidenced by gated myocardial perfusion imaging after treatment results in good prognosis in patients with coronary artery disease. J Cardiol. 2015;65(4):278–84.
Driessen RS, Danad I, Stuijfzand WJ, Schumacher SP, Knuuti J, Mäki M, et al. Impact of Revascularization on Absolute Myocardial Blood Flow as Assessed by Serial [(15)O]H(2)O Positron Emission Tomography Imaging: A Comparison With Fractional Flow Reserve. Circ Cardiovasc Imaging. 2018;11(5): e007417.
van Kranenburg M, Magro M, Thiele H, de Waha S, Eitel I, Cochet A, et al. Prognostic value of microvascular obstruction and infarct size, as measured by CMR in STEMI patients. JACC Cardiovasc Imaging. 2014;7(9):930–9.
Danad I, Raijmakers PG, Driessen RS, Leipsic J, Raju R, Naoum C, et al. Comparison of Coronary CT Angiography, SPECT, PET, and Hybrid Imaging for Diagnosis of Ischemic Heart Disease Determined by Fractional Flow Reserve. JAMA Cardiol. 2017;2(10):1100–7.
Driessen RS, van Diemen PA, Raijmakers PG, Knuuti J, Maaniitty T, Underwood SR, Nagel E, Robbers LFHJ, Demirkiran A, von Bartheld MB, van de Ven PM, Hofstra L, Somsen GA, Tulevski II, Boellaard R, van Rossum AC, Danad I, Knaapen P. Functional stress imaging to predict abnormal coronary fractional flow reserve: the PACIFIC 2 study. Eur Heart J. 2022;43(33):3118–3128. https://doi.org/10.1093/eurheartj/ehac286
Harms HJ, Knaapen P, de Haan S, Halbmeijer R, Lammertsma AA, Lubberink M. Automatic generation of absolute myocardial blood flow images using [15O]H2O and a clinical PET/CT scanner. Eur J Nucl Med Mol Imaging. 2011;38(5):930–9.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart - A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105(4):539–42.
Danad I, Uusitalo V, Kero T, Saraste A, Raijmakers PG, Lammertsma AA, et al. Quantitative assessment of myocardial perfusion in the detection of significant coronary artery disease: cutoff values and diagnostic accuracy of quantitative [(15)O]H2O PET imaging. J Am Coll Cardiol. 2014;64(14):1464–75.
Amado LC, Gerber BL, Gupta SN, Rettmann DW, Szarf G, Schock R, et al. Accurate and objective infarct sizing by contrast-enhanced magnetic resonance imaging in a canine myocardial infarction model. J Am Coll Cardiol. 2004;44(12):2383–9.
Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50(12):1161–70.
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’t Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213–24.
Johnson NP, Tóth GG, Lai D, Zhu H, Açar G, Agostoni P, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol. 2014;64(16):1641–54.
Rimac G, Fearon WF, De Bruyne B, Ikeno F, Matsuo H, Piroth Z, et al. Clinical value of post-percutaneous coronary intervention fractional flow reserve value: A systematic review and meta-analysis. Am Heart J. 2017;183:1–9.
De Bruyne B, Baudhuin T, Melin JA, Pijls NH, Sys SU, Bol A, et al. Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation. 1994;89(3):1013–22.
Lee JM, Kim CH, Koo BK, Hwang D, Park J, Zhang J, Tong Y, Jeon KH, Bang JI, Suh M, Paeng JC, Cheon GJ, Na SH, Ahn JM, Park SJ, Kim HS. Integrated myocardial perfusion imaging diagnostics improve detection of functionally significant coronary artery stenosis by 13N-ammonia positron emission tomography. Circ Cardiovasc Imaging. 2016;9(9):e004768. https://doi.org/10.1161/CIRCIMAGING
Driessen RS, Stuijfzand WJ, Raijmakers PG, Danad I, Min JK, Leipsic JA, et al. Effect of Plaque Burden and Morphology on Myocardial Blood Flow and Fractional Flow Reserve. J Am Coll Cardiol. 2018;71(5):499–509.
Imai S, Kondo T, Stone GW, Kawase Y, Ahmadi AA, Narula J, et al. Abnormal Fractional Flow Reserve in Nonobstructive Coronary Artery Disease. Circ Cardiovasc Interv. 2019;12(2): e006961.
Acampa W, Zampella E, Assante R, Genova A, De Simini G, Mannarino T, et al. Quantification of myocardial perfusion reserve by CZT-SPECT: A head to head comparison with (82)Rubidium PET imaging. J Nuclear Cardiol. 2021;28(6):2827–39.
Mannarino T, D’Antonio A, Assante R, Zampella E, Gaudieri V, Buongiorno P, et al. Regional myocardial perfusion imaging in predicting vessel-related outcome: interplay between the perfusion results and angiographic findings. Eur J Nucl Med Mol Imaging. 2022;50(1):160–7.
Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging. 2012;5(4):430–40.
Bom MJ, Driessen RS, Raijmakers PG, Everaars H, Lammertsma AA, van Rossum AC, et al. Diagnostic value of longitudinal flow gradient for the presence of haemodynamically significant coronary artery disease. Eur Heart J Cardiovasc Imaging. 2019;20(1):21–30.
de Winter RW, Jukema RA, van Diemen PA, Schumacher SP, Driessen RS, Stuijfzand WJ, Everaars H, Bom MJ, van Rossum AC, van de Ven PM, Verouden NJ, Nap A, Raijmakers PG, Danad I, Knaapen P. The impact of coronary revascularization on vessel-specific coronary flow capacity and long-term outcomes: a serial [15O]H2O positron emission tomography perfusion imaging study. Eur Heart J Cardiovasc Imaging. 2022;23(6):743–752. https://doi.org/10.1093/ehjci/jeab263
Gould KL. Apples, oranges, or pears: unexpected insights in coronary pathophysiology. Eur Heart J Cardiovasc Imaging. 2019;20(1):14–7.
Wang L, Jerosch-Herold M, Jacobs DR Jr, Shahar E, Folsom AR. Coronary risk factors and myocardial perfusion in asymptomatic adults: the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Coll Cardiol. 2006;47(3):565–72.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356(8):830–40.
Ishihara M, Sato H, Tateishi H, Kawagoe T, Shimatani Y, Kurisu S, et al. Time course of impaired coronary flow reserve after reperfusion in patients with acute myocardial infarction. Am J Cardiol. 1996;78(10):1103–8.
Gould KL, Johnson NP. Coronary Physiology Beyond Coronary Flow Reserve in Microvascular Angina: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72(21):2642–62.
Collet C, Sonck J, Vandeloo B, Mizukami T, Roosens B, Lochy S, et al. Measurement of Hyperemic Pullback Pressure Gradients to Characterize Patterns of Coronary Atherosclerosis. J Am Coll Cardiol. 2019;74(14):1772–84.
Danad I, Raijmakers PG, Appelman YE, Harms HJ, de Haan S, van den Oever ML, et al. Coronary risk factors and myocardial blood flow in patients evaluated for coronary artery disease: a quantitative [15O]H2O PET/CT study. Eur J Nucl Med Mol Imaging. 2012;39(1):102–12.
van Bussel EF, Hoevenaar-Blom MP, Poortvliet RKE, Gussekloo J, van Dalen JW, van Gool WA, et al. Predictive value of traditional risk factors for cardiovascular disease in older people: A systematic review. Prev Med. 2020;132: 105986.
Baskaran L, Danad I, Gransar H, Ó Hartaigh B, Schulman-Marcus J, Lin FY, et al. A Comparison of the Updated Diamond-Forrester, CAD Consortium, and CONFIRM History-Based Risk Scores for Predicting Obstructive Coronary Artery Disease in Patients With Stable Chest Pain: The SCOT-HEART Coronary CTA Cohort. JACC Cardiovasc Imaging. 2019;12(7 Pt 2):1392–400.
Kato S, Saito N, Nakachi T, Fukui K, Iwasawa T, Taguri M, et al. Stress perfusion coronary flow reserve versus cardiac magnetic resonance for known or suspected CAD. J Am Coll Cardiol. 2017;70(7):869–79.
Pijls NH. Fractional flow reserve after previous myocardial infarction. Eur Heart J. 2007;28(19):2301–2.
Grönman M, Tarkia M, Stark C, Vähäsilta T, Kiviniemi T, Lubberink M, et al. Assessment of myocardial viability with [(15)O]water PET: A validation study in experimental myocardial infarction. J Nuclear Cardiol. 2021;28(4):1271–80.
Driessen RS, Raijmakers PG, Stuijfzand WJ, Knaapen P. Myocardial perfusion imaging with PET. Int J Cardiovasc Imaging. 2017;33(7):1021–31.
Vos NS, Amoroso G, Grundeken MJ, Ijsselmuiden AJ, van Geuns RJ, Spaargaren R, et al. Pre-hospital management, procedural performance and outcomes for primary percutaneous coronary intervention in ST-elevation myocardial infarction in the Netherlands: Insights from the Dutch cohort of the APPOSITION-III trial. Neth Heart J. 2016;24(12):730–9.
Uren NG, Crake T, Lefroy DC, de Silva R, Davies GJ, Maseri A. Delayed recovery of coronary resistive vessel function after coronary angioplasty. J Am Coll Cardiol. 1993;21(3):612–21.
Spyrou N, Khan MA, Rosen SD, Foale R, Davies DW, Sogliani F, et al. Persistent but reversible coronary microvascular dysfunction after bypass grafting. Am J Physiol Heart Circ Physiol. 2000;279(6):H2634–40.
Funding
Internal funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Prof. Knaapen received research grants from HeartFlow Inc. All other authors have no conflict of interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ruurt Jukema and Ruben de Winter shared first authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jukema, R., de Winter, R., Hopman, L. et al. Impact of cardiac history and myocardial scar on increase of myocardial perfusion after revascularization. Eur J Nucl Med Mol Imaging 50, 3897–3909 (2023). https://doi.org/10.1007/s00259-023-06356-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06356-4