Abstract
Purpose
Clinical PET imaging of human epidermal growth factor receptor 2 (HER2) can noninvasively detect HER2 overexpression in lesions. A novel 68Ga-NOTA-MAL-MZHER2 (68Ga-HER2) affibody was developed for clinical PET/CT, and its safety, tissue dosimetry, ability to detect HER2-positive lesions, and utility for HER2-targeted therapy in patients with advanced gastric cancer (AGC) were evaluated.
Methods
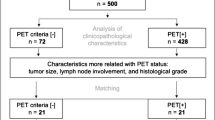
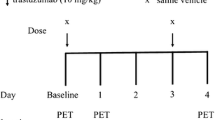
Thirty-four patients with AGC (23 with HER2-positive and 11 with HER2-negative primary lesions) were included and underwent PET/CT after an injection of approximately 3.7 MBq/kg body weight 68Ga-HER2 affibody. Thirteen patients (8 HER2-positive and 5 HER2-negative patients) were scanned at 1, 2, and 3 h post-injection to determine the best imaging timepoint, and the remaining patients were scanned at the optimized timepoint. All patients underwent standard 18F-FDG PET/CT within 7 d to identify viable lesions. The SUVmax of lesions larger than 1.0 cm were analyzed. Five lesion maxima were analyzed for each organ.
Results
(1) The 68Ga-HER2 affibody was safe and effective, and optimal image contrast was observed 2 h post-injection; the average effective absorbed dose was 0.0215 mSv/MBq. (2) The HER2-positive group had significantly higher 68Ga-HER2 affibody uptake than the HER2-negative group (SUVmax 10.7 ± 12.5 vs 3.8 ± 1.7, p = 0.005). The specificity and sensitivity were 100 and 55.4%, respectively, with a SUVmax cutoff value of 6.6. The SUVmax of the lesions ranged from 1.6 to 73.0, suggesting heterogeneity in HER2 expression. (3) 68Ga-HER2 affibody uptake showed an organ-dependent difference in patients with HER2-positive expression. Bone metastases had the highest uptake (SUVmax 40.5 ± 24.9), followed by liver metastases (SUVmax 11.9 ± 3.9) and lymph node metastases (SUVmax 5.6 ± 3.7), while the uptake in other lesions, including in the primary lesion, was relatively lower (SUVmax 7.3 ± 3.7). (4) Patients receiving therapy had a non-significantly lower lesion SUVmax than patients not receiving therapy (SUVmax 8.8 ± 4.9 vs 11.8 ± 15.2) (p = 0.253). Additionally, the 68Ga-HER2 affibody detected positive lesions in 1/11 patients with HER2-negative primary gastric cancer, which was confirmed by second generation gene sequencing. (5) Moreover, ten patients underwent baseline PET/CT followed by targeted anti-HER2 therapy. Patients with lesions showing high avidity to the 68Ga-HER2 affibody showed longer progression-free survival (PFS) than those with lesions showing low avidity (4–9 m vs 2–3 m).
Conclusion
68Ga-HER2 affibody PET/CT is a feasible method to noninvasively detect the HER2 status in AGC patients and enable early detection with a low dose. Ongoing anti-HER2 therapy did not influence 68Ga-HER2 affibody imaging, which allowed repeated evaluations to monitor the HER2 status after anti-HER2 therapy. This method provides an in vivo understanding of AGC biology that will ultimately help oncologists improve individualized therapy plans.










Similar content being viewed by others
Abbreviations
- HER2:
-
human epidermal receptor type 2
- 68Ga-HER2 affibody:
-
68Ga-NOTA-MAL-MZHER2
- MAL:
-
maleimide
- GC:
-
gastric cancer
- AGC:
-
advanced gastric cancer
- FPS:
-
progression-free survival
- IHC:
-
immunohistochemistry
- GEC:
-
gastroesophageal junction cancer
- i.v.:
-
intravenous injection
- h:
-
hour
- FISH:
-
fluorescent in situ hybridization
- DISH:
-
dual in situ hybridization
- PET:
-
positron emission tomography
- 68Ga:
-
Gallium-68
- AUCs:
-
areas under the curve
- HPLC:
-
high-performance liquid chromatography
- p.i.:
-
post-injection
- PPV:
-
positive predictive value
- NPV:
-
negative predictive value
- radio-TLC:
-
radioactive thin-layer chromatography scanner
- d:
-
day
- SUVmax :
-
the maximum single-voxel standardized uptake value
- ROIs:
-
regions of interest
- %ID/g:
-
percent injected dose per gram
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30.
Roskoski R Jr. The ErbB/HER family of protein-tyrosine kinases and cancer. Pharmacol Res. 2014;79:34–74.
Gravalos C, Jimeno A. HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol. 2008;19:1523–9.
Hofmann M, Stoss O, Shi D, et al. Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology. 2008;52:797–805.
Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687–97.
Ajani JA, D'Amico TA, Almhanna K, et al. Gastric cancer, version 3.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2016;14:1286–312.
Grillo F, Fassan M, Sarocchi F, Fiocca R, Mastracci L. HER2 heterogeneity in gastric/gastroesophageal cancers: from benchside to practice. World J Gastroenterol. 2016;22:5879–87.
Kanayama K, Imai H, Yoneda M, Hirokawa YS, Shiraishi T. Significant intratumoral heterogeneity of human epidermal growth factor receptor 2 status in gastric cancer: a comparative study of immunohistochemistry, FISH, and dual-color in situ hybridization. Cancer Sci. 2016;107:536–42.
Nishida Y, Kuwata T, Nitta H, et al. A novel gene-protein assay for evaluating HER2 status in gastric cancer: simultaneous analyses of HER2 protein overexpression and gene amplification reveal intratumoral heterogeneity. Gastric Cancer. 2015;18:458–66.
Park SR, Park YS, Ryu MH, et al. Extra-gain of HER2-positive cases through HER2 reassessment in primary and metastatic sites in advanced gastric cancer with initially HER2-negative primary tumours: results of GASTric cancer HER2 reassessment study 1 (GASTHER1). Eur J Cancer. 2016;53:42–50.
Watson S, Validire P, Cervera P, et al. Combined HER2 analysis of biopsies and surgical specimens to optimize detection of trastuzumab-eligible patients in eso-gastric adenocarcinoma: a GERCOR study. Ann Oncol. 2013;24:3035–9.
Kim KM, Bilous M, Chu KM, et al. Human epidermal growth factor receptor 2 testing in gastric cancer: recommendations of an Asia-Pacific task force. Asia Pac J Clin Oncol. 2014;10:297–307.
Dijkers EC, Kosterink JG, Rademaker AP, et al. Development and characterization of clinical-grade 89Zr-trastuzumab for HER2/neu immunoPET imaging. J Nucl Med. 2009;50:974–81.
Dijkers EC, Oude Munnink TH, Kosterink JG, et al. Biodistribution of 89Zr-trastuzumab and PET imaging of HER2-positive lesions in patients with metastatic breast cancer. Clin Pharmacol Ther. 2010;87:586–92.
O'Donoghue JA, Lewis JS, Pandit-Taskar N, et al. Pharmacokinetics, biodistribution, and radiation dosimetry for (89)Zr-trastuzumab in patients with esophagogastric cancer. J Nucl Med. 2018;59:161–6.
Tamura K, Kurihara H, Yonemori K, et al. 64Cu-DOTA-trastuzumab PET imaging in patients with HER2-positive breast cancer. J Nucl Med. 2013;54:1869–75.
Ulaner GA, Hyman DM, Ross DS, et al. Detection of HER2-positive metastases in patients with HER2-negative primary breast cancer using 89Zr-trastuzumab PET/CT. J Nucl Med. 2016;57:1523–8.
Beylergil V, Morris PG, Smith-Jones PM, et al. Pilot study of 68Ga-DOTA-F(ab')2-trastuzumab in patients with breast cancer. Nucl Med Commun. 2013;34:1157–65.
Tolmachev V. Imaging of HER-2 overexpression in tumors for guiding therapy. Curr Pharm Des. 2008;14:2999–3019.
Orlova A, Wallberg H, Stone-Elander S, Tolmachev V. On the selection of a tracer for PET imaging of HER2-expressing tumors: direct comparison of a 124I-labeled affibody molecule and trastuzumab in a murine xenograft model. J Nucl Med. 2009;50:417–25.
Sorensen J, Velikyan I, Sandberg D, et al. Measuring HER2-receptor expression in metastatic breast cancer using [68Ga]ABY-025 affibody PET/CT. Theranostics. 2016;6:262–71.
Yanai A, Harada R, Iwata R, et al. Site-specific labeling of F-18 proteins using a supplemented cell-free protein synthesis system and O-2-[(18)F]fluoroethyl-L-tyrosine: [(18)F]FET-HER2 affibody molecule. Mol Imaging Biol. 2019;21:529–37.
Kramer-Marek G, Kiesewetter DO, Martiniova L, et al. [18F]FBEM-Z(HER2:342)-affibody molecule—a new molecular tracer for in vivo monitoring of HER2 expression by positron emission tomography. Eur J Nucl Med Mol Imaging. 2008;35:1008–18.
Kramer-Marek G, Bernardo M, Kiesewetter DO, et al. PET of HER2-positive pulmonary metastases with 18F-ZHER2:342 affibody in a murine model of breast cancer: comparison with 18F-FDG. J Nucl Med. 2012;53:939–46.
Velikyan I. 68Ga-based radiopharmaceuticals: production and application relationship. Molecules. 2015;20:12913–43.
Baum RP, Prasad V, Muller D, et al. Molecular imaging of HER2-expressing malignant tumors in breast cancer patients using synthetic 111In- or 68Ga-labeled affibody molecules. J Nucl Med. 2010;51:892–7.
Xu Y, Bai Z, Huang Q, et al. PET of HER2 expression with a novel (18)FAl labeled affibody. J Cancer. 2017;8:1170–8.
Xu Y, Wang L, Pan D, et al. PET imaging of a (68)Ga labeled modified HER2 affibody in breast cancers: from xenografts to patients. Br J Radiol. 2019;92:20190425.
Sandstrom M, Lindskog K, Velikyan I, et al. Biodistribution and radiation dosimetry of the anti-HER2 affibody molecule 68Ga-ABY-025 in breast cancer patients. J Nucl Med. 2016;57:867–71.
Bates M, Sperinde J, Kostler WJ, et al. Identification of a subpopulation of metastatic breast cancer patients with very high HER2 expression levels and possible resistance to trastuzumab. Ann Oncol. 2011;22:2014–20.
Mortimer JE, Bading JR, Park JM, et al. Tumor uptake of (64)Cu-DOTA-trastuzumab in patients with metastatic breast cancer. J Nucl Med. 2018;59:38–43.
Boyer AP, Collier TS, Vidavsky I, Bose R. Quantitative proteomics with siRNA screening identifies novel mechanisms of trastuzumab resistance in HER2 amplified breast cancers. Mol Cell Proteomics. 2013;12:180–93.
Sandberg D, Tolmachev V, Velikyan I, et al. Intra-image referencing for simplified assessment of HER2-expression in breast cancer metastases using the affibody molecule ABY-025 with PET and SPECT. Eur J Nucl Med Mol Imaging. 2017;44:1337–46.
Gebhart G, Lamberts LE, Wimana Z, et al. Molecular imaging as a tool to investigate heterogeneity of advanced HER2-positive breast cancer and to predict patient outcome under trastuzumab emtansine (T-DM1): the ZEPHIR trial. Ann Oncol. 2016;27:619–24.
D'Huyvetter M, Vincke C, Xavier C, et al. Targeted radionuclide therapy with a 177Lu-labeled anti-HER2 nanobody. Theranostics. 2014;4:708–20.
Bhusari P, Vatsa R, Singh G, et al. Development of Lu-177-trastuzumab for radioimmunotherapy of HER2 expressing breast cancer and its feasibility assessment in breast cancer patients. Int J Cancer. 2017;140:938–47.
Acknowledgments
The current research was financially supported by the National Key Research and Development Program of China (No. 2017YFC1308900), National Major Scientific and Technological Special Project for “Significant New Drugs Development”(2017ZX09304021), National Natural Science Foundation (31671035, 81472749), Jiangsu Program for Innovation Research Team (CXTDA2017024), Jiangsu Provincial Natural Science Foundation (BK20170204), Jiangsu Health International Exchange Program (JSH-2018-015), Jiangsu talent projects (LGY2017088), Beijing Natural Science Foundation, Jing-Jin-Ji special projects for basic research cooperation (H2018206600), Beijing Excellent Talents Funding (2017000021223ZK33), Beijing Municipal Administration of Hospitals-Yangfan Project (ZYLX201816), Jiangsu Provincial Commission of Health and Family Planning Foundation (H2017031), and Wuxi Commission of Health and Family Planning Foundation (Q201729).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflict of interests.
Ethical approval
All procedures in this study were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later versions. Informed consent was, or its equivalent, was obtained from all patients included in the study. The clinical study was approved by the Ethics Committee of the Beijing Cancer Hospital (ethical approval no. 2018KT61).
Informed consent
Informed consent was obtained from the 34 individual participants included in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology—Digestive Tract
Electronic supplementary material
ESM 1
(DOC 46 kb)
Rights and permissions
About this article
Cite this article
Zhou, N., Liu, C., Guo, X. et al. Impact of 68Ga-NOTA-MAL-MZHER2 PET imaging in advanced gastric cancer patients and therapeutic response monitoring. Eur J Nucl Med Mol Imaging 48, 161–175 (2021). https://doi.org/10.1007/s00259-020-04898-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-020-04898-5