Abstract
Objective
Use subchondral bone length (SBL), a new MRI-derived measure that reflects the extent of cartilage loss and bone flattening, to predict the risk of progression to total knee replacement (TKR).
Methods
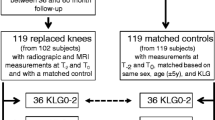
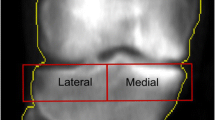
We employed baseline MRI data from the Osteoarthritis Initiative (OAI), focusing on 760 men and 1214 women with bone marrow lesions (BMLs) and joint space narrowing (JSN) scores, to predict the progression to TKR. To minimize bias from analyzing both knees of a participant, only the knee with a higher Kellgren-Lawrence (KL) grade was considered, given its greater potential need for TKR. We utilized the Kaplan–Meier survival curves and Cox proportional hazards models, incorporating raw and normalized values of SBL, JSN, and BML as predictors. The study included subgroup analyses for different demographics and clinical characteristics, using models for raw and normalized SBL (merged, femoral, tibial), BML (merged, femoral, tibial), and JSN (medial and lateral compartments). Model performance was evaluated using the time-dependent area under the curve (AUC), Brier score, and Concordance index to gauge accuracy, calibration, and discriminatory power. Knee joint and region-level analyses were conducted to determine the effectiveness of SBL, JSN, and BML in predicting TKR risk.
Results
The SBL model, incorporating data from both the femur and tibia, demonstrated a predictive capacity for TKR that closely matched the performance of the BML score and the JSN grade. The Concordance index of the SBL model was 0.764, closely mirroring the BML’s 0.759 and slightly below JSN’s 0.788. The Brier score for the SBL model stood at 0.069, showing comparability with BML’s 0.073 and a minor difference from JSN’s 0.067. Regarding the AUC, the SBL model achieved 0.803, nearly identical to BML’s 0.802 and slightly lower than JSN’s 0.827.
Conclusion
SBL’s capacity to predict the risk of progression to TKR highlights its potential as an effective imaging biomarker for knee osteoarthritis.



Similar content being viewed by others
Data availability
This study used data available in the public domain (https://nda.nih.gov/oai/).
References
Cui A, Li H, Wang D, et al. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587. https://doi.org/10.1016/j.eclinm.2020.100587. ([published Online First: 20201126]).
Cooper C, Cushnaghan J, Kirwan JR, et al. Radiographic assessment of the knee joint in osteoarthritis. Ann Rheum Dis. 1992;51(1):80–2. https://doi.org/10.1136/ard.51.1.80.
Gunther KP, Sun Y. Reliability of radiographic assessment in hip and knee osteoarthritis. Osteoarthr Cartil. 1999;7(2):239–46. https://doi.org/10.1053/joca.1998.0152.
Klara K, Collins JE, Gurary E, et al. Reliability and accuracy of cross-sectional radiographic assessment of severe knee osteoarthritis: role of training and experience. J Rheumatol. 2016;43(7):1421–6. https://doi.org/10.3899/jrheum.151300. ([published Online First: 20160415]).
Lanyon P, O’Reilly S, Jones A, et al. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis. 1998;57(10):595–601. https://doi.org/10.1136/ard.57.10.595.
Newman S, Ahmed H, Rehmatullah N. Radiographic vs. MRI vs. arthroscopic assessment and grading of knee osteoarthritis–- are we using appropriate imaging? J Exp Orthop. 2022;9(1):2. https://doi.org/10.1186/s40634-021-00442-y. ([published Online First: 20220103]).
Ravaud P, Giraudeau B, Auleley GR, et al. Radiographic assessment of knee osteoarthritis: reproducibility and sensitivity to change. J Rheumatol. 1996;23(10):1756–64.
Summers MN, Haley WE, Reveille JD, et al. Radiographic assessment and psychologic variables as predictors of pain and functional impairment in osteoarthritis of the knee or hip. Arthritis Rheum. 1988;31(2):204–9. https://doi.org/10.1002/art.1780310208.
Vignon E, Conrozier T, Piperno M, et al. Radiographic assessment of hip and knee osteoarthritis. Recommendations: recommended guidelines. Osteoarthr Cartil. 1999;7(4):434–6. https://doi.org/10.1053/joca.1999.0235.
Warashina H, Hasegawa Y, Tsuchiya H, et al. Clinical, radiographic, and thermographic assessment of osteoarthritis in the knee joints. Ann Rheum Dis. 2002;61(9):852–4. https://doi.org/10.1136/ard.61.9.852.
Roemer FW, Guermazi A, Hannon MJ, et al. Presence of magnetic resonance imaging-defined inflammation particularly in overweight and obese women increases risk of radiographic knee osteoarthritis: the POMA study. Arthritis Care Res (Hoboken). 2022;74(8):1391–8. https://doi.org/10.1002/acr.24568.
Zhao Y, Xia Y, Kuang G, et al. Cross-tissue analysis using machine learning to identify novel biomarkers for knee osteoarthritis. Comput Math Methods Med. 2022;2022:9043300. https://doi.org/10.1155/2022/9043300. ([published Online First: 20220623]).
Teoh YX, Lai KW, Usman J, et al. Discovering knee osteoarthritis imaging features for diagnosis and prognosis: review of manual imaging grading and machine learning approaches. J Healthc Eng. 2022;2022:4138666. https://doi.org/10.1155/2022/4138666. ([published Online First: 20220218]).
Tan JS, Tippaya S, Binnie T, et al. Predicting knee joint kinematics from wearable sensor data in people with knee osteoarthritis and clinical considerations for future machine learning models. Sensors (Basel). 2022;22(2). https://doi.org/10.3390/s22020446. [published Online First: 20220107].
Nowinka Z, Alagha MA, Mahmoud K, et al. Predicting depression in patients with knee osteoarthritis using machine learning: model development and validation study. JMIR Form Res. 2022;6(9):e36130. https://doi.org/10.2196/36130. ([published Online First: 20220913]).
Kokkotis C, Ntakolia C, Moustakidis S, et al. Explainable machine learning for knee osteoarthritis diagnosis based on a novel fuzzy feature selection methodology. Phys Eng Sci Med. 2022;45(1):219–29. https://doi.org/10.1007/s13246-022-01106-6. ([published Online First: 20220131]).
Joseph GB, McCulloch CE, Nevitt MC, et al. Machine learning to predict incident radiographic knee osteoarthritis over 8 years using combined MR imaging features, demographics, and clinical factors: data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2022;30(2):270–9. https://doi.org/10.1016/j.joca.2021.11.007. ([published Online First: 20211118]).
Bonakdari H, Pelletier JP, Blanco FJ, et al. Single nucleotide polymorphism genes and mitochondrial DNA haplogroups as biomarkers for early prediction of knee osteoarthritis structural progressors: use of supervised machine learning classifiers. BMC Med. 2022;20(1):316. https://doi.org/10.1186/s12916-022-02491-1. ([published Online First: 20220912]).
Bonakdari H, Pelletier JP, Abram F, et al. A machine learning model to predict knee osteoarthritis cartilage volume changes over time using baseline bone curvature. Biomedicines. 2022;10(6). https://doi.org/10.3390/biomedicines10061247. [published Online First: 20220526].
Zeng K, Hua Y, Xu J, et al. Multicentre study using machine learning methods in clinical diagnosis of knee osteoarthritis. J Healthc Eng. 2021;2021:1765404. https://doi.org/10.1155/2021/1765404. ([published Online First: 20211203]).
Peuna A, Thevenot J, Saarakkala S, et al. Machine learning classification on texture analyzed T2 maps of osteoarthritic cartilage: oulu knee osteoarthritis study. Osteoarthr Cartil. 2021;29(6):859–69. https://doi.org/10.1016/j.joca.2021.02.561. ([published Online First: 20210223]).
Leporace G, Gonzalez F, Metsavaht L, et al. Are there different gait profiles in patients with advanced knee osteoarthritis? A machine learning approach. Clin Biomech (Bristol, Avon). 2021;88:105447. https://doi.org/10.1016/j.clinbiomech.2021.105447. ([published Online First: 20210814]).
Kokkotis C, Moustakidis S, Baltzopoulos V, et al. Identifying robust risk factors for knee osteoarthritis progression: an evolutionary machine learning approach. Healthcare (Basel). 2021;9(3). https://doi.org/10.3390/healthcare9030260. [published Online First: 20210301].
Jamshidi A, Pelletier JP, Labbe A, et al. Machine learning-based individualized survival prediction model for total knee replacement in osteoarthritis: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken). 2021;73(10):1518–27. https://doi.org/10.1002/acr.24601. ([published Online First: 20210826]).
Cheung JC, Tam AY, Chan LC, et al. Superiority of multiple-joint space width over minimum-joint space width approach in the machine learning for radiographic severity and knee osteoarthritis progression. Biology (Basel). 2021;10(11). https://doi.org/10.3390/biology10111107. [published Online First: 20211027].
Brisson NM, Gatti AA, Damm P, et al. Association of machine learning-based predictions of medial knee contact force with cartilage loss over 2.5 years in knee osteoarthritis. Arthritis Rheumatol. 2021;73(9):1638–45. https://doi.org/10.1002/art.41735. ([published Online First: 20210806]).
Bonakdari H, Jamshidi A, Pelletier JP, et al. A warning machine learning algorithm for early knee osteoarthritis structural progressor patient screening. Ther Adv Musculoskelet Dis. 2021;13:1759720X21993254. https://doi.org/10.1177/1759720X21993254. ([published Online First: 20210223]).
Tiwari A, Poduval M, Bagaria V. Evaluation of artificial intelligence models for osteoarthritis of the knee using deep learning algorithms for orthopedic radiographs. World J Orthop. 2022;13(6):603–14. https://doi.org/10.5312/wjo.v13.i6.603. ([published Online First: 20220618]).
Tang X, Guo D, Liu A, et al. Fully automatic knee joint segmentation and quantitative analysis for osteoarthritis from magnetic resonance (MR) images using a deep learning model. Med Sci Monit. 2022;28:e936733. https://doi.org/10.12659/MSM.936733. ([published Online First: 20220614]).
Panfilov E, Tiulpin A, Nieminen MT, et al. Deep learning-based segmentation of knee MRI for fully automatic subregional morphological assessment of cartilage tissues: data from the Osteoarthritis Initiative. J Orthop Res. 2022;40(5):1113–24. https://doi.org/10.1002/jor.25150. ([published Online First: 20210806]).
Li D, Bharti B, Wei J, et al. Sex imbalance produces biased deep learning models for knee osteoarthritis detection. Can Assoc Radiol J. 2022;8465371221120539. https://doi.org/10.1177/08465371221120539. [published Online First: 20220830].
Kunze KN, Jang SJ, Li T, et al. Radiographic findings involved in knee osteoarthritis progression are associated with pain symptom frequency and baseline disease severity: a population-level analysis using deep learning. Knee Surg Sports Traumatol Arthrosc. 2022. https://doi.org/10.1007/s00167-022-07213-x. ([published Online First: 20221111]).
Jiang G, Ding J, Ge C. Deep learning-based CT imaging to evaluate the therapeutic effects of acupuncture and moxibustion therapy on knee osteoarthritis. Comput Math Methods Med. 2022;2022:1135196. https://doi.org/10.1155/2022/1135196. ([published Online First: 20220521]).
Hu Y, Tang J, Zhao S, et al. Deep learning-based multimodal 3 T MRI for the diagnosis of knee osteoarthritis. Comput Math Methods Med. 2022;2022:7643487. https://doi.org/10.1155/2022/7643487. ([published Online First: 20220429]).
Guan B, Liu F, Mizaian AH, et al. Deep learning approach to predict pain progression in knee osteoarthritis. Skeletal Radiol. 2022;51(2):363–73. https://doi.org/10.1007/s00256-021-03773-0. ([published Online First: 20210409]).
Ahmed SM, Mstafa RJ. A comprehensive survey on bone segmentation techniques in knee osteoarthritis research: from conventional methods to deep learning. Diagnostics (Basel). 2022;12(3). https://doi.org/10.3390/diagnostics12030611. [published Online First: 20220301].
Abdullah SS, Rajasekaran MP. Automatic detection and classification of knee osteoarthritis using deep learning approach. Radiol Med. 2022;127(4):398–406. https://doi.org/10.1007/s11547-022-01476-7. ([published Online First: 20220309]).
Neogi T, Bowes MA, Niu J, et al. Magnetic resonance imaging-based three-dimensional bone shape of the knee predicts onset of knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Rheum. 2013;65(8):2048–58. https://doi.org/10.1002/art.37987.
Chang GH, Park LK, Le NA, et al. Subchondral bone length in knee osteoarthritis: a deep learning-derived imaging measure and its association with radiographic and clinical outcomes. Arthritis Rheumatol. 2021;73(12):2240–8. https://doi.org/10.1002/art.41808. ([published Online First: 20211029]).
Harrell FE Jr, Califf RM, Pryor DB, et al. Evaluating the yield of medical tests. JAMA. 1982;247(18):2543–6.
U.S. Department of Health and Human Services. (n.d.). NIMH Data Archive–- OAI. National Institutes of Health. https://nda.nih.gov/oai/ [Dataset].
Acknowledgements
We thank Dr. Jonathan Scalera, Boston University Chobanian & Avedisian School of Medicine, for his assistance with MRI annotations.
Funding
This work was supported in part by a grant from the Karen Toffler Charitable trust, grants from the American Heart Association (17SDG33670323 and 20SFRN35460031), and grants from the National Institutes of Health (R01-AR070139, RF1-AG062109, R01-HL159620, R21-CA253498, R43-DK134273, U01-AG018820 and P30-AR072571).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study did not require ethical approval.
Competing interests
The authors declare no competing interests.
Patient and public involvement
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Surendran, T., Park, L.K., Lauber, M.V. et al. Survival analysis on subchondral bone length for total knee replacement. Skeletal Radiol (2024). https://doi.org/10.1007/s00256-024-04627-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00256-024-04627-1