Abstract
Objective
Prostate cancer frequently metastasizes to bone, inducing osteosclerotic lesions. The objective of this study was to clarify the three-dimensional (3D) trabecular bone microstructure in bone metastasis from prostate cancer by comparison with normal and degenerative sclerotic bone lesions, using microcomputed tomography (micro-CT).
Design and materials
A total of 32 cancellous bone samples were excised from the lumbar spine of six autopsy patients: 15 metastatic samples (one patient), eight degenerative sclerotic samples (four patients) and the rest from normal sites (three patients). The samples were serially scanned cross-sectionally by micro-CT with a pixel size of 23.20 µm, slice thickness of 18.56 µm, and image matrix of 512×512. Each image data set consisted of 250 consecutive slices. The volumes of interest (96×96×120 voxels) were defined in the original image sets and 3D indices of the trabecular microstructure were determined.
Results
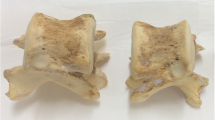
The trabecular thickness (Tb.Th) in degenerative sclerotic lesions was significantly higher than that in normal sites, whereas no significant difference was observed in trabecular number (Tb.N). By contrast, in metastatic lesions, the Tb.N was significantly higher with increased bone volume fraction (BV/TV) than in normal sites, and no significant difference was found in Tb.Th. The characteristics of the trabecular surface in the metastatic samples showed concave structural elements with an increase in BV/TV, indicating osteolysis of the trabecular bone. In 3D reconstructed images, increased trabecular bone with an irregular surface was observed in samples from metastatic sites, which were uniformly sclerotic on soft X-ray radiographs.
Conclusion
These results support, through 3D morphological features, the strong bone resorption effect in bone metastasis from prostate cancer.








Similar content being viewed by others
References
Koutsilieris M. Osteoblastic metastasis in advanced prostate cancer. Anticancer Res 1993; 13:443–450.
Jacobs SC. Spread of prostatic cancer to bone. Urology 1983; 21:337–344.
Charhon SA, Chapuy MC, Delvin EE, Valentin-Opran A, Edouard CM, Meunier PJ. Histomorphometric analysis of sclerotic bone metastases from prostatic carcinoma with special reference to osteomalacia. Cancer 1983; 51:918–924.
Aoki J, Yamamoto I, Hino M, et al. Sclerotic bone metastasis: radiologic-pathologic correlation. Radiology 1986; 159:127–132.
Clarke NW, McClure J, George NJR. Morphometric evidence for bone resorption and replacement in prostate cancer. Br J Urol 1991; 68:74–80.
Odgaard A, Gundersen HJG. Quantification of connectivity in cancellous bone, with special emphasis on 3-D reconstructions. Bone 1993; 14:173–182.
Parfitt AM, Drezner MK, Glorieux FH, et al. Bone histomorphometry: standardization of nomenclature, symbols, and units. J Bone Miner Res 1987; 2:595–610.
Hildebrand T, Rüegsegger P. A new method for the model-independent assessment of thickness in three-dimensional images. J Microsc 1997; 185:67–75.
Hahn M, Vogel M, Pompesius-Kempa M, Delling G. Trabecular bone pattern factor: a new parameter for simple quantification of bone microarchitecture. Bone 1992; 13:327–330.
Whitehouse WJ. The quantitative morphology of anisotropic trabecular bone. J Microsc 1974; 101:153–168.
Müller R, Hahn M, Vogel M, Delling G, Rüegsegger P. Morphometric analysis of noninvasively assessed bone biopsies: comparison of high-resolution computed tomography and histologic sections. Bone 1996; 18:215–220.
Jorgensen SM, Demirkaya O, Ritman EL. Three-dimensional imaging of vasculature and parenchyma in intact rodent organs with X-ray micro-CT. Am J Physiol 1998; 275:H1103―H1114.
Hildebrand T, Laib A, Müller R, Dequeker J, Rüegsegger P. Direct Three-dimensional morphometric analysis of human cancellous bone: microstructural data from spine, femur, iliac crest, and calcaneus. J Bone Miner Res 1999; 14:1167–1174.
Müller R, Campenhout HV, Damme BV, et al. Morphometric analysis of human bone biopsies: a quantitative structural comparison of histological sections and micro-computed tomography. Bone 1998; 23:59–66.
Adami S. Bisphosphonates in prostate carcinoma. Cancer. 1997; 80:1674–1679.
Galasko CS. Mechanisms of lytic and blastic metastatic disease of bone. Clin Orthop 1982; 169:20–27.
Tamada T, Sone T, Tomomitsu T, Jo Y, Tanaka H, Fukunaga M. Biochemical markers for the detection of bone metastasis in patients with prostate cancer: diagnostic efficacy and the effect of hormonal therapy. J Bone Miner Metab 2001; 19:45–51.
Koizumi M, Maeda H, Yoshimura K, Yamauchi T, Kawai T, Ogata E. Dissociation of bone formation markers in bone metastasis of prostate cancer. Br J Cancer 1997; 75:1601–1604.
Takeuchi S, Arai K, Saitoh H, Yoshida K, Miura M. Urinary pyridinoline and deoxypyridinoline as potential markers of bone metastasis in patients with prostate cancer. J Urol 1996; 156:1691–1695.
Koizumi M, Yamada Y, Takiguchi T, et al. Bone metabolic markers in bone metastases. J Cancer Res Clin Oncol 1995; 121:542–548.
Scher HI, Chung LWK. Bone metastases: improving the therapeutic index. Semin Oncol 1994; 21:630–656.
Percival RC, Urwin GH, Harris S, et al. Biochemical and histological evidence that carcinoma of the prostate is associated with increased bone resorption. Eur J Surg Oncol 1987; 13:41–49.
Urwin GH, Percival RC, Harris S, Beneton MNC, Williams JL, Kanis JA. Generalised increase in bone resorption in carcinoma of the prostate. Br J Urol 1985; 57:721–723.
Roudier MP, Vesselle H, True LD, Higano CS, Ott SM, King SH, Vessella RL. Bone histology at autopsy and matched bone scintigraphy findings in patients with hormone refractory prostate cancer: the effect of bisphosphonate therapy on bone scintigraphy results. Clin Exp Metastas 2003; 20:171–180.
Roland SI. Calcium studies in ten cases of osteoblastic prostatic metastasis. J Urol 1958; 79:339–342.
Heidenreich A, Hofmann R, Engelmann UH. The use of bisphosphonate for the palliative treatment of painful bone metastasis due to hormone refractory prostate cancer. J Urol 2001; 165:136―140.
Adami S. Salvagno G, Guarrera G, et al. Dichloromethylene-diphosphonate in patients with prostatic carcinoma metastatic to the skeleton. J Urol 1985; 134:1152–1154.
Percival RC, Watson ME, Williams JL, Kanis JA. Carcinoma of the prostate: remission of paraparesis with inhibitors of bone resorption. Postgrad Med J 1985; 61:551–553.
Kylmälä T, Tammela T, Risteli L, Risteli J, Taube T, Elomaa I. Evaluation of the effect of oral clodronate on skeletal metastases with type 1 collagen metabolites: a controlled trial of the Finnish prostate cancer group. Eur J Cancer 1993; 29:821–825.
Vinholes J, Guo C-Y, Purohit OP, Eastell R, Coleman RE. Metabolic effects of pamidronate in patients with metastatic bone disease. Br J Cancer 1996; 73;1089–1095.
Garnero P, Buchs N, Zekri J, Rizzoli R, Coleman RE, Delmas PD. Markers of bone turnover for the management of patients with bone metastases from prostate cancer. Br J Cancer 2000; 82:858–864.
Acknowledgements
This study was supported in part by a Research Project Grant (no. 12-504) from Kawasaki Medical School. The authors would like to thank Hitoshi Nagatsuka, DDS, PhD and Noriyuki Nagai, DDS, PhD for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamada, T., Sone, T., Jo, Y. et al. Three-dimensional trabecular bone architecture of the lumbar spine in bone metastasis from prostate cancer: comparison with degenerative sclerosis. Skeletal Radiol 34, 149–155 (2005). https://doi.org/10.1007/s00256-004-0855-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-004-0855-x