Abstract
The management of image quality and radiation dose during pediatric CT scanning is dependent on how well one manages the radiographic techniques as a function of the type of exam, type of CT scanner, and patient size. The CT scanner’s display of expected CT dose index volume (CTDIvol) after the projection scan provides the operator with a powerful tool prior to the patient scan to identify and manage appropriate CT techniques, provided the department has established appropriate diagnostic reference levels (DRLs). This paper provides a step-by-step process that allows the development of DRLs as a function of type of exam, of actual patient size and of the individual radiation output of each CT scanner in a department. Abdomen, pelvis, thorax and head scans are addressed. Patient sizes from newborns to large adults are discussed. The method addresses every CT scanner regardless of vendor, model or vintage. We cover adjustments to techniques to manage the impact of iterative reconstruction and provide a method to handle all available voltages other than 120 kV. This level of management of CT techniques is necessary to properly monitor radiation dose and image quality during pediatric CT scans.
Similar content being viewed by others
Introduction: a solution for an important challenge
Authors within the radiology scientific community have argued for the last decade or so that there is potential for the development of radiation-induced cancer from radiation doses similar to those found during diagnostic CT studies of pediatric patients [1–3]. Although these authors have established the need for scan parameters to be tailored to each patient, steady evolution in scanner technology among CT vendors and among models within the same vendor has outpaced the development of appropriate pediatric CT protocols [4]. Careful management of pediatric CT image quality and radiation dose in an environment with rapidly changing technology is a big challenge.
Creating CT protocols is a daunting task for many a radiologist. The purpose of this paper is to provide the radiologist, radiologic technologist and medical physicist with a stepwise approach to this task. This approach requires the site’s doses of adult-size patients to fall within guidelines set by the American College of Radiology (ACR). This beginning requirement ensures that the site’s doses are reasonable with respect to doses at similar institutions. The noise levels in images of adult-size patients should also be acceptable to a site’s radiologists. Starting from there, we present a straightforward method that allows the radiologist, radiologic technologist and medical physicist to alter the tube current, rotation time of the gantry, the tube voltage, reformatted slice thickness, and the pitch to develop appropriate pediatric protocols from the site’s adult-size protocols. Although the scope of recommended changes may appear overwhelming, small steps can be initially taken. As staff members within the department become accustomed to higher noise/lower dose images associated with initial changes, e.g., tube current reduction only, more advanced changes, e.g., tube voltage change or iterative reconstruction, can be introduced.
Some tools that have only recently become available are needed to allow more effective management of pediatric radiation dose and image quality. First, no simple method to estimate the CT radiation dose to an individual pediatric patient existed until 2011 [5]. Second, the American College of Radiology’s Dose Index Registry has only recently begun to store patient CT dose indices from facilities across the nation [6, 7]. These data from the dose index registry allow the development of national diagnostic reference levels (DRLs), which have been very limited and not well understood in the United States [8].
The solution to this management challenge is the availability of unique scan parameters for each child that address the patient’s size, type of CT examination and the individual radiation output of the scanner. There are two approaches to this challenge. The first approach, which is beyond the scope of this paper, involves developing a detailed technique chart specific to each scanner within the department that lists scan parameters for each type of examination as a function of patient size [9, 10]. This is a robust, sound approach but takes a significant commitment and substantial staff time to establish and maintain. This type of staffing may only be available at large academic centers, so scanner-specific protocol sets for both adult-size patients and children may not be available in adult-focused facilities. Yet the vast majority of pediatric patients are not scanned in dedicated pediatric centers; up to 90% of pediatric CT scans performed in emergency rooms are performed in adult-focused hospitals [11].
A second approach, the focus of this paper, involves developing patient-specific scan parameters based on patient size and type of exam, to be determined by the CT operator at the time of the exam [12]. This approach verifies the appropriate pediatric scan parameters just prior to the patient scan once the size (attenuation characteristics) of the patient, type of examination, and actual CT scanner are known. Essentially, the voltage and mAs used for the scan are adjusted to provide the patient dose that matches previously adopted department DRLs. The method addresses manual vs. modulated tube current, changed voltage/tube current techniques, and iterative reconstruction dose reductions for examinations of the head, thorax and abdomen/pelvis.
Which of the two approaches is the better choice? When the American Association of Physicists in Medicine (AAPM) begins publishing scanner-specific pediatric CT protocols on their Web site for specific CT scanners, this will be an excellent source of information that a department should be able to adapt into their practice with a reasonable effort. Until then, the scanner-specific method is probably the best choice for a department that has the resources to develop detailed scanner-specific protocols. For departments that do not have the resources to develop detailed protocols for each scanner for each possible size of pediatric patient, the second approach, patient-specific protocols based on patient size, should be pursued. The second approach requires more time and effort of staff when the pediatric patient arrives in the department. While the second approach occasionally results in a less-than-optimal pediatric scan technique, this approach should provide better patient care than the use of adult-size techniques or adoption of detailed pediatric techniques not developed for the scanner model and manufacturer of the scanner available in the department.
Establishing scan parameters, CTDIvol and Size Specific Dose Estimates (SSDE) for adult-size patients on a primary CT scanner
All the measured dose data and scan parameters necessary to establish a target dose for adult-size abdomen and head exams on the department’s primary scanner should be available within the department. The department’s qualified medical physicist must perform CTDI radiation dose measurements annually to maintain ACR accreditation and typically to comply with state regulations [13]. The qualified medical physicist’s records should provide both the measured CTDIvol and the scan parameters used to complete the measurement.
First, the department should establish that the primary scanner’s measured CTDIvol values agree with published DRLs. The CTDIvol measured with scan parameters used for standard scanning (iterative reconstruction turned off) should not exceed the diagnostic reference level values published by the ACR for adult-size patients:
If the measured CTDIvol values are close to these recommended limits, with the help of a qualified medical physicist, the department might elect to reduce scan parameters to reduce adult-size patient doses. For example, assume the department elects to reduce abdominal doses by 20%. This can be achieved by reducing the average mAs value during the scan by 20%. If the department is using iterative reconstruction, measured CTDIvol should be less than the ACR’s published diagnostic reference levels. For example, if the recommendation for the level of iterative reconstruction is a reduced patient dose of 30%, the measured CTDIvol should be less than 70% of the ACR’s published diagnostic reference levels.
This analysis establishes for the primary CT scanner a standard set of scan parameters (voltage, tube current, rotation time, slice width, and pitch) that deliver the desired radiation dose to the correct CTDI phantom, 16-cm and 32-cm diameter, respectively, for the adult-size head and body. Because CTDIvol is not a patient dose, one should estimate the SSDE, the weighted average patient dose to soft tissues within the scan volume, using equation 1 for the average adult-size abdominal scan [15]:
The dimensions of an adult-size abdomen of 28 × 38 cm [15] result in similar attenuation to the 32-cm diameter CTDI phantom on which the displayed CTDIvol is based.
Because SSDE has not been defined for head scans, the SSDE for head scans cannot be estimated. This first step ensures that the selected baseline scan parameters are appropriate for the particular design of the site’s primary CT scanner and for the site’s radiologists’ tolerance of quantum mottle in the CT images for adult-size head and abdomen exams.
Matching image quality for adult-size patients on all CT scanners
If a department uses more than one CT scanner, the image quality for a given size patient for a given type of exam should be similar regardless of which CT scanner is used. Image quality for a given exam and patient size is affected by the scanner’s hardware, by its image reconstruction algorithms, and by the radiation dose delivered to the patient. Although matching the radiation dose delivered to the patient for all scanners in the department does not guarantee similar image quality among all possible scanners, matching radiation dose to the patient should be a good first step to achieving similar image quality in many departments with a limited number of scanners, especially if the design of the department’s scanners is not significantly different. However radiologists, radiologic technologists and qualified medical physicists at the site must work as a team after matching patient radiation doses on all scanners to validate that similar image quality was achieved. Methods on how to ensure similar image quality among a site’s scanners when similar patient doses fail to achieve this goal can be found elsewhere [16]. This paper is focused on achieving similar radiation doses for the same size patient for a given type of exam among all the scanners in a given department.
Matching radiation dose for a given size patient does not mean that the scan parameters used on each CT scanner will be similar. This occurs because of the differing design characteristics of CT scanners from different vendors and of different models of CT scanners from the same vendor.
Recall that CTDIvol measures the radiation dose delivered to standard CTDI phantoms [17]. Therefore the radiation dose to a patient from two different scanners will be similar if the displayed CTDIvol values are the same. Some scanners use short geometry while others use long geometry, as illustrated in Fig. 1. The scanner using long geometry must generate more X-rays per unit time because of the inverse square law to deliver the appropriate rate to the CT detector. If the bow-tie filter of a scanner attenuates more of the generated X-rays (dependent on composition and thickness of the filter), again, more X-rays must be generated. These two design differences are just two examples why the rate of radiation reaching the surface of the patient, which primarily determines the patient dose, can be significantly different on two different CT scanners using identical voltage, tube current, rotation time and pitch. End users cannot accurately estimate differences in patient dose between two CT scanners by simply comparing the product of tube current and rotation time (mAs).
Diagram shows focal spot relative to detector of CT scanner. a A greater distance between the focal spot and detector with long geometry requires more radiographic technique to deliver the same radiation dose to the patient. b Short geometry results in a significantly shorter distance from focal spot to detector
As a specific example, assume the qualified medical physicist measured 25 mGy for CTDIvol with a 32-cm CTDI phantom for an abdomen exam on the department’s primary scanner using 120 kV, 250 mAs and a pitch of 1. Because 25 mGy equals the ACR’s published DRL for routine abdomen exams, a site might elect to reduce the CTDIvol by 20% to 20 mGy. This can be achieved by either reducing the mAs scan parameter by 20% to 200 mAs, or by increasing the pitch 20% to 1.2. The DRL for the primary CT scanner for average adult-size abdomens corresponding to the 32-cm CTDI phantom (28x38 cm, see previous section) with scan parameters is:
Because the above DRL is specified for an average adult-size abdomen that corresponds to the CTDIvol of the standard 32-cm CTDI phantom [15], the SSDE is calculated from the displayed CTDIvol using equation 1.
Assume the qualified medical physicist used the same scan parameters and measured a CTDIvol of 13 mGy on scanner #2. The scan parameters must be increased by the ratio of the two measured CTDIvol values (20/13) = 1.54 to obtain the desired CTDIvol value of 20 mGy on the second scanner. Therefore,
result in a CTDIvol of 20 mGy and patient dose of 23 mGy (SSDE) on both scanners for the abdomen. Data for these two scanners might look like the following for routine average adult-size head exams:
resulting in a CTDIvol of ~74 mGy on both scanners for routine adult-size head examinations.
This analysis should be performed for all scanners in the department to ensure similar patient doses for both adult-size abdomens and heads regardless of which scanner is used. As discussed previously, staff within the department must then verify that similar patient doses result in similar image quality for the same size patient on all the department’s scanners.
Establishing pediatric patient DRLs for all CT scanners
After the designated radiologists, radiologic technologists and qualified medical physicists have verified that the baseline radiographic techniques for adult-size abdomens and heads result in similar image quality on all the site’s CT scanners, staff at the site can proceed to establish reasonable scan parameters for children. Acceptable levels of quantum mottle vary from one department to another based on the requirements of the radiologists within each department. Their tolerance of quantum mottle during high-contrast examinations of the chest, musculoskeletal system and select abdominal protocols such as the evaluation for renal stones should be greater. The recommendations provided here are for general soft-tissue studies.
In 2008 simple dose reduction tables for abdomens and chest were posted on the Image Gently Web site (www.imagegently.org) to assist in the development of pediatric techniques (Fig. 2). Eight patient ages and posteroanterior thicknesses were provided with a reduction factor that could be multiplied by the department’s adult-size mAs scan parameter to estimate a reasonable pediatric mAs as a function of patient size. Because these recommendations are based on the site’s adult-size CT dose, the relative level of quantum mottle acceptable to the site’s radiologists for adult imaging is maintained. These reduction factors were designed to deliver radiation doses to pediatric patients that were equal or slightly less than the site’s medium-size adult doses for the same CT examination.
Original downloadable worksheet on Image Gently Web site (www.imagegently.org) assists the user in the development of pediatric CT techniques that manage radiation dose as a function of patient size for the abdomen and thorax. Reduced mAs values in the table were designed to deliver a radiation dose to pediatric patients that is similar to the site’s standard adult-size radiation dose at 120 kV. BL baseline, PA posteroanterior, RF reduction factor
Today we have more robust data that allow significant improvement to the recommendations of 2008. Figure 3 is an updated, downloadable table, published on the Image Gently Web site. The fifth column lists the same ages of patients. Data published in 2010 [18] provided the anteroposterior and lateral thicknesses of the patient’s abdomen in columns 1 and 2. More important, these data illustrated that age is a poor indication of patient size; the largest 3-year-old abdomens were equal in size to the smallest 18-year-old abdomens. For this reason, the operator is encouraged to specify the size of the pediatric patient as opposed to the age. The effective diameters were calculated from the posteroanterior and lateral dimensions [15]. The mass for each patient size in column 4 comes from average weight and age data [19].
Downloadable worksheet on the Image Gently Web site is designed to assist the user in the development of pediatric CT techniques for the abdomen. The first four columns provide size and mass of eight different-size patients. Columns 6–8 provide options for limited, moderate or aggressive reduction of patient dose as a function of patient size. Columns 9–11 indicate the expected patient dose, or SSDE, expressed in units of mGy. Columns 12–14 indicate the reduced mAs value to be used for each of the three reduction models as a function of patient size. The assumed voltage is 120 kV. The data are for scanner #1. AP anteroposterior, LAT lateral, NB newborn, SSDE size-specific dose estimate
The sixth through eighth columns are the core of this table (Fig. 3). Column 6 uses the same dose-reduction criteria of the original table in Fig. 2. The differing reductions of mAs assigned to each patient size are designed to deliver the same radiation dose to the patient regardless of size. The reduction factors in column 6 differ by a few percentage points from the original reduction factors because of improved available data [15]. The one-quarter mAs for the newborn in column 8 reduces the patient dose for a newborn to half the dose of the department’s adult-size abdomen. The reduction factor varies linearly from the quarter mAs for the newborn to full mAs for the standard adult-size patient. This reduction factor was found to be acceptable to pediatric radiologists at six pediatric hospitals in the United States [20]. Column 7 lists reduction factors that are halfway in between the reduction factors listed in columns 6 and 8.
Columns 6 through 8 of Fig. 3 are labeled “limited,” “moderate,” and “aggressive” to indicate the degree of dose reduction as a function of the patient’s size. Columns 9 through 11 list the patient dose (SSDE) for the three levels of reduction. These columns are populated when the user fills in the voltage, tube current, rotation time, pitch used by qualified medical physicist when making axial CTDI dose measurements (should always be 1), pitch to be used during the clinical exam, and the size-specific patient dose estimate (SSDE) for the standard-size adult that corresponds to the 32-cm CTDI phantom (thickness dimensions of the abdomen of 28 × 38 cm [15]). Columns 12–14 list the estimated mAs that should be used for each patient size, depending on which of the three levels of reduction one selects.
Figure 4 is the same table as Fig. 3, but now for scanner #2. By comparing the data in Figs. 3 and 4, the recommended mAs values are different between the scanners that deliver the same radiation dose, SSDE, to the patient. A table for each scanner in the department needs to be created using the scan parameters for the adult-size abdomen.
Image from the Image Gently Web site shows the same downloadable example worksheet as in Fig. 3 except the circled tube current for an adult abdomen for scanner #2 is inserted. A comparison of the results of Figs. 3 and 4 illustrates that the estimated patient doses are similar for each of the three reduction models (columns 9–11), while the actual reduced techniques (mAs) in columns 12–14 are substantially different for scanners #1 and #2
Establishing pediatric chest DRLs for all CT scanners
Methods have been described to establish adult-size abdomen techniques that deliver similar patient doses regardless of the scanner used in a department. Because the thorax contains significantly more air in the lung fields than is found in the abdomen or pelvis, X-ray attenuation is not as pronounced in the thorax. Using an abdominal technique for the thorax delivers more X-rays to the detector, which reduces quantum mottle in the image but also increases the patient’s radiation dose. Therefore the technique factors for the thorax should be reduced to avoid an increase in patient dose relative to the abdomen. Let us assume the required reduction is 20%, which can be achieved by reducing the previously calculated technique factors by 20%. For scanner #1 the original technique of
while for scanner #2 the original technique of
The method used in the previous section can now be applied to the adult-size thorax technique factors in the previous paragraph to establish thorax DRLs based on patient size. Therefore 160 mAs for scanner #1 should be inserted in the table of Fig. 3 at the oval; the spreadsheet is designed to calculate the correct mAs for scanner #1 in columns 12–14. This step would be repeated for each scanner at the site; 245 mAs would be inserted at the oval for scanner #2. Reduction factors in column 8 (aggressive) of the table in Fig. 3 are based on an evaluation of image quality of abdominal images at six pediatric hospitals. Although these hospitals are analyzing similar data for the thorax, the results are not yet published. When the data become available, an additional technique reduction table for the thorax will be added to the Image Gently Web site. In the meantime, it might be prudent for one to start with reductions based on the moderate (column 7) model for the thorax until published results verify whether more significant reductions are reasonable.
Establishing pediatric head DRLs for all CT scanners
Because adult-size head techniques and associated CTDIvol have been established for all scanners in the department in previous sections, one needs to apply reduction factors as a function of patient size to establish appropriate pediatric head DRLs for all CT scanners in the department. Figure 5 provides the necessary data, which are similar to Fig. 3 with a couple exceptions. First, only five patient sizes are provided. The head of a 1-year-old is approximately 80% of an adult-size head, and that of a 5-year-old is 90% of an adult-size head [18], which reduces the patient sizes needed to model the growth of the head. Second, no aggressive model for dose reduction is provided because a study of image quality and dose for pediatric heads is not available like it is for pediatric abdomens [20].
This downloadable worksheet from Image Gently serves the same purpose as the worksheet of Fig. 3, except this one is for the head as opposed to the abdomen. Only two reduction models are provided, in columns 6 and 7, as opposed to the previous three models. Because size-specific dose estimate (SSDE) is not defined for the head, there is no indication of patient dose represented by SSDE. Columns 8 and 9 indicate the reduced mAs value as a function of patient head size. The data are for scanner #1 using 120 kV
Image of the same downloadable worksheet as from Image Gently as in Fig. 5, except the circled tube current for an adult head for scanner #2 is inserted. Again, the estimated patient doses in Figs. 4 and 6 are the same for each of the two reduction models (columns 6 and 7) while the actual reduced techniques (mAs) in columns 8 and 9 are substantially different for scanners #1 and #2
The rationale for the data in column 6 of Fig. 5 is similar to that for the data in column 6 of Fig. 3: the recommended reductions in mAs should result in similar dose to the patient regardless of pediatric patient size. These recommendations were originally based on unpublished dose measurements within anthropomorphic phantoms designed to model a newborn, a 2-year-old, a 6-year-old and an adult-size head.
Column 7 of Fig. 5, moderate mAs reduction factor, results in a radiation dose to the 16-cm CTDI phantom for a 1-year-old technique that is 47% of the CTDI dose of the adult-size technique to the same 16-cm CTDI phantom on the same scanner. Is column 7 in Fig. 5 a reasonable model? Yes, for two reasons. First, the mAs in column 9 of Fig. 5 for a 1-year-old’s head is 47% of the adult-size mAs. This matches the ACR’s recommended reference CTDIvol doses of 35 mGy and 75 mGy for a 1-year-old and adult-size head CT exam [13]. The ACR-recommended values are based on measured CTDIvol clinical head doses submitted with accreditation applications by thousands of sites for their CT scanners. Second, the reduction of mAs listed in column 9 changes exponentially with changes in thickness of the patient’s head. This means that as smaller heads are imaged, the technique (mAs) is reduced so the number of X-rays exiting the patient remains essentially constant at the detector. This results in dose reduction to the patient as head size decreases, but not at the expense of image quality because the number of X-rays reaching the detector determines quantum mottle in the image. The data in Fig. 6 is similar to the data in Fig. 5 with the exception of columns 8 and 9, because Fig. 6 is for scanner #2 as opposed to scanner #1.
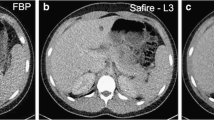
Establishing iterative reconstruction DRLs for all CT scanners
Several authors have described dose reductions achieved with iterative reconstruction techniques offered by CT manufacturers [21–24]. These studies demonstrate that iterative reconstruction can maintain diagnostic image quality for certain clinical applications at reduced dose levels to the patient.
Pediatric techniques that provide reduced doses associated with iterative reconstruction are best determined using the technique reduction tables found in Figs. 3 and 5. For example, assume the recommended dose reduction via iterative reconstruction techniques is 30%. The site knows the basic technique and dose for adult-size heads or abdomens from the previously described methods for the CT scanners in question. If the standard adult-size technique for a given exam requires 300 mAs, dose from this technique will be reduced 30% using 300 × 0.7 = 210 mAs. So 210 mAs is plugged into the table in either Fig. 3 or 5 to obtain the appropriate additional reduction in mAs as a function of patient size. As with all other implemented dose reductions, the site should carefully evaluate image quality and validate any dose reduction recommendations provided by the CT vendor relative to achievable dose reduction with application of iterative reconstruction.
Establishing reduced voltage techniques for all examinations
The previous sections provide methods that can be used to develop a variety of CT techniques all at the same voltage, 120 kV. Decreasing the voltage decreases the energy carried by each photon, which leads to a less penetrating beam, increased quantum mottle in the image, and less dose to the patient if no other scan parameters are adjusted [25]. In most situations, a lower voltage increases contrast in soft-tissue organs and in CT angiography studies. The degree of change in radiation dose and quantum mottle caused by changes in voltage can be reduced by changing the mAs in the opposite direction of the change in tube voltage [26].
The choice of voltage should be made based on the need for subject contrast in the image [27–30]. About 120 kV is reasonable for the majority of soft-tissue imaging in children without intravenous or oral contrast agents. To improve contrast or to perform CT angiography, 100 kV is reasonable for medium-size pediatric patients. Neonates to small pediatric patients can be imaged at as low as 80 kV. The 80-kV images at the maximum tube current of the CT scanner will not produce an adequate number of X-rays to avoid artifacts and maintain reasonable quantum mottle in the image for larger pediatric patients [31].
How does one practically adjust patient dose for pediatric CT scanning with voltages other than 120 kV? First, the methods of the previous sections are used to identify the appropriate mAs at 120 kV for a given patient on a given scanner. After reducing the voltage for pediatric imaging, the mAs is either increased to maintain the original radiation dose with improved contrast in the image or increased to a lesser degree to maintain the original image quality (contrast-to-noise ratio) with some reduction in radiation dose.
The first case, reduced voltage at same dose, is the simplest. Use the methods of the previous sections to establish department DRLs for each scanner. When scanning each patient, complete the projection scan. Dial in the 120-kV pediatric protocol and the reduced mAs from the previous methods. The scanner should display a projected CTDIvol for the 120-kV technique. Note the CTDIvol. Dial in the reduced voltage, 70 kV, 80 kV, 90 kV or 100 kV (depending on patient size and scanner model), and increase the mAs until the displayed CTDIvol matches the CTDIvol of the 120-kV technique [31]. This should provide an increase in image quality at the same dose that would be used with a 120-kV technique.
In the second case, reduced voltage and reduced dose, a reduction of voltage increases contrast in the image with a concurrent increase in noise. If the increase in noise is greater than the increase in contrast, the contrast-to-noise ratio and image quality will decrease unless the mAs is increased. For example, consider 80 kV vs. 120 kV imaging:
One must increase the mAs and patient dose until the increase in quantum mottle in the image decreases to 30% with no reduction in contrast-to-noise ratio compared to the original image. The magnitude of the adjustment is dependent on the imaging task and the size of the patient. A greater degree of dose reduction can typically be achieved with smaller patients [31].
How does one determine the change in contrast with change in voltage? One simple method involves scanning the second section of the ACR CT accreditation phantom with every available voltage setting on the CT scanner in question. One must use a clinically appropriate scan or display field of view as well as clinically used image processing for the types of examinations in question. The selected scan or display field of view may change the bowtie filter used, depending on the design of the scanner. Both the bowtie filter and image processing affect contrast in the clinical images. The ACR CT accreditation phantom should be available at many sites that have obtained ACR CT accreditation unless the site depends on a consultant qualified medical physicist to provide the ACR phantom.
Figure 7 is a typical image of the second section of the ACR CT accreditation phantom. Placing a region of interest, similar to the circular one shown, over the 1-cm disc at the top of the image and over a background region to the left of the 1-cm disc allows the calculation of the mean signal strengths (CT number) in each of the two regions. The difference in the CT numbers between the regions of interest quantitates the contrast level in each image at a different voltage setting. The contrast at each voltage setting relative to (divided by) the contrast at 120 kV provides an estimate of the increase/decrease in contrast as a function of each voltage setting. In the example shown in Fig. 7, the contrast-to-noise ratio is:
Tube current modulation considerations
The majority of CT scans today involve tube current modulation, where the CT scanner varies the rate of radiation production as a function of path length of the X-rays passing through the patient. The CT scanner automatically controls the modulation of the tube current based on attenuation data acquired by the scanner during the projection scan of the patient’s body. However the operator must indicate the level of quantum mottle desired in the image. Because this affects the patient dose, it also determines the CTDIvol associated with the scan. Therefore, in the previous section, the operator sets the desired mAs in the case of a manual acquisition or the acceptable level of quantum mottle in the image when using the automated tube current modulation mode. More mAs or less quantum mottle in the image will increase the projected CTDIvol and vice versa. The operator must know in the case of modulated techniques how to indicate more or less quantum mottle to the automated tube current modulation system of the scanner. This operator control is different for each CT scanner manufacturer. Vendor dose education slide sets, which provide a starting point for operators who need more information, are available from GE Healthcare, Hitachi Medical Systems, NeuroLogica, Neusoft, Philips Healthcare, Siemens Healthcare and Toshiba [32]. The application specialist of your CT vendor should also be able to provide more information on this operator control.
Conclusion
The management of pediatric image quality and radiation dose is dependent on how well you develop and manage the radiographic techniques used for your pediatric CT scans. The recent development of size-specific dose estimate and the ACR’s national dose registry provides the data needed to develop more precise diagnostic reference levels within individual departments for their individual CT scanners. A department should establish some basic techniques as a function of patient size for different exams for each of its scanners up front. The CT scanner’s display of projected CTDIvol after the projection scan is complete, but before axial or helical scanning is initiated, provides the operator with a powerful tool that allows the correct scan parameters to be identified and selected immediately before the axial or helical scan for either manual or tube current modulated scans.
The ability to fine-tune techniques as a function of the patient size on a given scanner is required to properly manage pediatric image quality and radiation dose. This is especially true in adult-focused hospitals, which scan the vast majority of pediatric patients in the United States, despite the fact that pediatric CT imaging is typically the occasional scan in each individual adult hospital.
References
Brenner D, Elliston C, Hall E et al (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176:289–296
Paterson A, Frush DP, Donnelly LF (2001) Helical CT of the body: are settings adjusted for pediatric patients? AJR Am J Roentgenol 176:297–301
Donnelly LF, Emery KH, Brody AS et al (2001) Minimizing radiation dose for pediatric body applications of single-detector helical CT: strategies at a large children’s hospital. AJR Am J Roentgenol 176:303–306
Frush DP (2009) Radiation, CT, and children: the simple answer is … it’s complicated. Radiology 252:4–6
Strauss KJ, Goske MJ, Frush DP et al (2009) Image Gently vendor summit: working together for better estimates of pediatric radiation dose from CT. AJR Am J Roentgenol 192:1169–1175
Robinson TJ, Robinson JD, Kanal KM (2013) Implementation of the ACR dose index registry at a large academic institution: early experience. J Digit Imaging 26:309–315
Morin R (2011) TU‐B‐110‐02: ACR dose index registry for comparing CT dose indices. Med Phys 38:3749
Gray JE, Archer BR, Butler PF et al (2005) Reference values for diagnostic radiology: application and impact. Radiology 235:354–358
McCollough C (2011) Translating protocols across patient size: babies to bariatric. AAPM 2011 Summit. American Association of Physicists in Medicine, College Park, MD, p 45
Fletcher JG (2010) Adjusting kV to reduce dose or improve image quality — how to do it right. AAPM technology assessment institute: summit on CT dose. American Association of Physicists in Medicine, College Park, MD, p 62
Larson DB, Johnson LW, Schnell BM et al (2011) Rising use of CT in child visits to the emergency department in the United States, 1995–2008. Radiology 259:793–801
McCollough CH (2013) Standardization versus individualization: how each contributes to managing dose in computed tomography. Health Phys 105:445–453
American College of Radiology (2013) FAQ CT quality control manual. http://www.acr.org/~/media/ACR/Documents/Accreditation/CT/CT%20QC%20Manual%20FAQ%2081613%20Final.pdf. Accessed 12 June 2014
McCollough C, Branham T, Herlihy V et al (2006) Radiation doses from the ACR CT accreditation program: review of data since program inception and proposals for new reference values and pass/fail limits. RSNA 92nd Scientific Assembly, Chicago. http://doseoptimization.jacr.org/Content/PDF/McCollough-Diagnostic.pdf. Accessed 9 June 2014
Boone JM, Strauss KJ, Cody DD et al (2011) Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. American Association of Physicists in Medicine, College Park, MD, p 30. http://www.aapm.org/pubs/reports/rpt_204.pdf. Accessed 9 June 2014
Solomon JB, Christianson O, Samei E (2012) Quantitative comparison of noise texture across CT scanners from different manufacturers. Med Phys 39:6048–6055
Strauss KJ (2014) Dose indices: everybody wants a number. Pediatr Radiol. doi:10.1007/s00247-014-3104-z
Kleinman PL, Strauss KJ, Zurakowski D et al (2010) Patient size measured on CT images as a function of age at a tertiary care children’s hospital. AJR Am J Roentgenol 194:1611–1619
National Center for Health Statistics (2000) 2000 CDC growth charts for the United States: methods and development. Department of Health and Human Services, Hyattsville, MD, p 203
Goske MJ, Strauss KJ, Coombs LP et al (2013) Diagnostic reference ranges for pediatric abdominal CT. Radiology 268:208–218
Singh S, Kalra MK, Gilman MD et al (2011) Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology 259:565–573
Prakash P, Kalra MK, Ackman JB et al (2010) Diffuse lung disease: CT of the chest with adaptive statistical iterative reconstruction technique. Radiology 256:261–269
Singh S, Kalra MK, Hsieh J et al (2010) Abdominal CT: comparison of adaptive statistical iterative and filtered back projection reconstruction techniques. Radiology 257:373–383
Schindera ST, Diedrichsen L, Muller HC et al (2011) Iterative reconstruction algorithm for abdominal multidetector CT at different tube voltages: assessment of diagnostic accuracy, image quality and radiation dose in a phantom study. Radiology 260:454–462
Strauss KJ, Goske MJ, Kaste SC et al (2010) Image gently: ten steps you can take to optimize image quality and lower CT dose for pediatric patients. AJR Am J Roentgenol 194:868–873
Huda W, Ogden KM, Khorasani MR (2008) Effect of dose metrics and radiation risk models when optimizing CT x-ray tube voltage. Phys Med Biol 53:4719–4732
Huda W (2002) Dose and image quality in CT. Pediatr Radiol 32:751–754
Huda W, Scalzetti EM, Levin G (2000) Technique factors and image quality as functions of patient weight at abdominal CT. Radiology 217:430–435
Lucaya J, Piqueras J, Garcia-Pena P et al (2000) Low-dose high-resolution CT of the chest in children and young adults: dose, cooperation, artifact incidence, and image quality. AJR Am J Roentgenol 175:985–992
Crawley MT, Booth A, Wainwright A (2001) A practical approach to the first iteration in the optimization of radiation dose and image quality in CT: estimates of the collective dose savings achieved. Br J Radiol 74:607–614
Goske MJ, Callahan MJ, Frush DP et al (2012) The image gently campaign: championing radiation protection for children through awareness, educational resources and advocacy. In: Tack D, Kalra MK, Gevernois PA (eds) Radiation dose from multidetector CT, 2nd edn. Springer, New York, p 649
The American Association of Physicists in Medicine (2014) CT scan protocols. http://www.aapm.org/pubs/CTProtocols. Accessed 9 June 2014
Conflicts of interest
Keith J. Strauss provides paid consulting services to Philips Healthcare upon request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strauss, K.J. Developing patient-specific dose protocols for a CT scanner and exam using diagnostic reference levels. Pediatr Radiol 44 (Suppl 3), 479–488 (2014). https://doi.org/10.1007/s00247-014-3088-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-014-3088-8