Abstract
High-flow nasal cannula (HFNC) therapy has been applied in the perioperative respiratory care for children with congenital heart disease and respiratory problems. However, the information about the feasibility of home HFNC therapy remains lacking among them. We retrospectively reviewed 5 children with congenital heart disease and respiratory problems who underwent home HFNC therapy, and evaluated their feasibility and safety. Age and weight at the introduction of home HFNC therapy were 19 (2–119) months and 5.3 (3.1–11.4) kg, respectively. All subjects had chromosomal anomaly including trisomy 18 in 3 and trisomy 21 in 2 subjects. Cardiac diagnoses included ventricular septal defect in 3, tetralogy of Fallot with complete atrioventricular septal defect in one, and pulmonary atresia with ventricular septal defect in another subject. Other comorbidities involved pulmonary hypertension in 4, micrognathia in 4, West syndrome in one, and bronchial asthma in one subject. Respiratory manifestations involved cyanosis due to upper airway obstruction in 2 and central hypopnea in 2, and recurrent pneumonia in one subject. After home HFNC therapy, systemic oxygen saturation significantly increased from 60 (40–78)% to 83 (83–96)% (P = 0.04), while heart rate and blood partial pressure of carbon dioxide were significantly decreased. There was no adverse event relevant to home HFNC during the follow-up period of 12 (5–49) months. Among them, one patient subsequently underwent tracheotomy at 11 years of age, and two patients weaned to conventional home oxygen therapy at 7 and 23 months of age. Home HFNC is safe and feasible in children with congenital heart disease and respiratory problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with congenital heart disease (CHD) occasionally present with other comorbidities including respiratory problems or chromosomal anomaly. Recent advances in medical and surgical managements have improved the survival among such patients [1,2,3]. However, patients with airway obstruction, lung disease or central hypopnea may require continuous respiratory supports despite appropriate surgical interventions for CHD. Although nasal continuous positive airway pressure (CPAP) therapy has been widely performed among them for decades, high-flow nasal cannula (HFNC) recently has become an alternative to nasal CPAP [4]. HFNC can deliver heated and humidified air with appropriate fractional oxygen via a nasal prong, provide mild continuous positive airway pressure, reduce nasopharyngeal dead space, and promote a recruitment of the peripheral airway, thereby resulting in a reduction of breathwork [5, 6]. HFNC therapy has been mainly used in the clinical setting of neonatal respiratory distress, acute respiratory failure due to respiratory infection, and perioperative respiratory care among children with CHD [4, 5, 7]. In this study, we reviewed a case series of 5 children who underwent home HFNC for respiratory support, and evaluated their feasibility and safety.
Methods
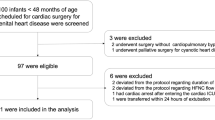
This study was approved by the Institutional Review Board in Kyushu Hospital, Japan Community Healthcare Organization. Informed consent was obtained from all patients’ guardians. We retrospectively reviewed clinical records and identified 5 subjects with CHD who underwent home HFNC therapy between 2017 and 2019. We obtained clinical data before and after home HFNC therapy, including systemic oxygen saturation, respiratory rate, heart rate, respiratory distress assessment instrument (RDSI) score and arterial or venous partial pressure of carbon dioxide (PCO2). RDSI score was calculated according to the previous study [8]. In the practice of home HFNC, a nasal prong adjusted to appropriate body size is connected to a home mechanical ventilator. Mechanical ventilators used are: MediOx 60® (PACIFIC MEDICO CO.,LTD. Tokyo, Japan) that offers both high-flow and positive pressure modes, and is equipped with a compressor, oxygen blender, humidifier heater base and pulse oximeter, providing total breathing care for patients with different interfaces available to match a range of environments, from medical institutions to the home; and Trilogy 100 plus® (Koninklijke Philips N.V., Eindhoven, Netherlands) and BiPAP A40® (Koninklijke Philips N.V., Eindhoven, Netherlands) that are equipment with a compressor, oxygen blender, and humidifier heater base to provide pressure-dependent ventilation. Home HFNC therapy is introduced after the admission for several days to ensure it is tolerable. Home healthcare providers maintained nasal prongs and mechanical ventilators to work appropriately every week.
Values are expressed as the median following the minimum and the maximum. Statistical analysis was performed using the Analysis TollPak In the Microsoft Office Excel™ add-in software. We compared clinical data before and a month after home HFNC therapy using the Wilcox-ranked analysis, and P value less than 0.05 was considered statistically significant.
Results
A summary of our series is shown in Table 1. Age and weight at the introduction of home HFNC were 19 (2–119) months and 5.3 (3.1–11.4) kg, respectively. There were 4 males. All subjects had chromosomal anomalies including trisomy 18 in 3, and trisomy 21 in 2 subjects. Primary CHD diagnoses included ventricular septal defect in 3, tetralogy of Fallot with complete atrioventricular septal defect in one, and pulmonary atresia wit ventricular septal defect in another subject. Other comorbidities included pulmonary hypertension in 4, micrognathia in 4, West syndrome in one, and bronchial asthma in another subject. Respiratory manifestations involved cyanosis due to upper airway obstruction in 2, and central hypopnea in 2, and recurrent pneumonia in one subject.
At a month after home HFNC therapy, systemic oxygen saturation significantly increased from 60 (40–78) to 83 (83–96)% (P = 0.04). Heart rate and PCO2 significantly decreased from 130 (108–145) bpm to 112 (90–134) bpm (P = 0.04) and from 94 (67–100) mmHg to 52 (42–66) mmHg (P = 0.04), respectively. Respiratory rate (from 40 [30–60] per min to 26 [20–40] per min, P = 0.06) and RDAI score (form 10 [3–16] to 3 [0–9], P = 0.06) tended to be decreased, but the differences did not reach statistical significance. There was no significant adverse event relevant to home HFNC during the follow-up period of 12 (5–49) months. Among them, one patient subsequently underwent tracheotomy at the age of 14 years, and two patients weaned to conventional home oxygen therapy at the age of 7 and 23 months. Herein, we describe 5 cases in detail as follows:
Case 1 A 2-month-old boy was admitted to our hospital because of cyanosis and feeding difficulty due to upper airway obstruction. He was born at the gestational age of 35 weeks and weighed 2768 g. He was diagnosed with tetralogy of Fallot and complete atrioventricular septal defect associated with trisomy 21. After birth, systemic oxygen saturation was 98% as there was adequate antegrade pulmonary blood flow. On admission, he developed tachypnea and respiratory distress with systemic oxygen saturation of 65%, due to the obstructive nasopharyngeal space. Blood gas analysis showed respiratory acidemia with pH level of 7.22 and pCO2 of 98 mmHg. We considered that the upper airway obstruction caused a decrease in pulmonary blood flow. He underwent home HFNC with a flow rate of 8 L/min and an oxygen fraction of 0.3 using MediOx 60®. Thereafter, his symptoms dramatically improved as he kept adequate alveolar oxygen tension and pulmonary blood flow. At the age of 6 months, his systemic oxygen saturation and body weight were 83% and 7.0 kg, respectively. At present, he is waiting for corrective surgery.
Case 2 A newborn male was admitted to the neonatal intensive care unit because of developing respiratory distress. He was born at the gestational age of 41 weeks and weighed 2068 g. Chromosomal test showed trisomy 18, and echocardiography showed ventricular septal defect and pulmonary hypertension. After respiratory support with HFNC for several days, his respiratory manifestations subsided, and HFNC was discontinued. However, his systemic oxygen saturation decreased to 50% during sleep, probably due to central hypopnea. As a result, HFNC was restarted. At the age of 5 months, he was discharged with home HFNC at a flow rate of 7 L/min and an oxygen fraction of 0.21 using MediOx 60®. His systemic oxygen saturation and respiratory rate after home HFNC were 82% and 40 /min, respectively. Home HFNC was changed to oxygen supplement therapy via nasal cannula at the age of 7 months. His condition is stable in the outpatient clinic.
Case 3 A 12-month-old boy was admitted to our hospital because of cyanosis due to upper airway obstruction and wheezy bronchitis. He was born at the gestational age of 39 weeks and weighed 2040 g. He was diagnosed with pulmonary atresia with ventricular septal defect associated with trisomy 21. Despite an appropriate placement of a right modified Blalock-Taussig shunt at the age of 4 months, his systemic oxygen saturation fluctuated between 70 and 90%. He was discharged with home oxygen therapy at the age of 7 months. However, he was repeatedly hospitalized for epileptic seizure due to West syndrome and cyanosis (systemic oxygen saturation below 60%) due to wheezy respiratory infection. Initially, HFNC was introduced at a flow rate of 14 L/min and an oxygen fraction of 1.0, and his symptoms improved. We, therefore, performed home HFNC using a conventional mechanical ventilator (Trilogy 100 plus®) on CPAP mode with a pressure of 6 cmH2O and an oxygen flow of 3 L/min. His systemic oxygen saturation was stable at approximately 85% even by this system. He underwent the Rastelli operation at the age of 22 months and weaned from home HFNC to nasal oxygen supplementation. At the age of 27 months, his systemic oxygen saturation at room air was 100% without respiratory distress.
Case 4 A 4-year-old boy was admitted to our hospital because of recurrent respiratory infection. He was born at the gestational age of 39 weeks and weighed 1686 g. He was diagnosed with ventricular septal defect and pulmonary stenosis associated with trisomy 18. Although the symptoms related to his heart failure was limited, he presented respiratory distress due to micrognathia and central hypopnea. His systemic oxygen saturation and respiratory rate were 76% and 30/min, respectively. He was intubated and supported by mechanical ventilation for a week. Although his clinical manifestations related to respiratory infection were improved, hypercapnia (PCO2 of 94 mmHg) persisted due to micrognathia and central hypopnea. Moreover, home HFNC therapy was performed using BiPAP A40 ® at a pressure of 4 cmH2O and an oxygen flow rate of 0.25 L/min; however, as he developed nausea and vomiting, BiPAP A40® that was a pressure-dependent device was changed to MediOx 60® that was a flow-dependent device. MediOx 60® was set at a flow rate of 8L/min and an oxygen fraction of 0.21–0.25. Subsequently, his symptoms improved, and his systemic oxygen saturation and respiratory rate were 86% and 26/min, respectively. At the age of 5 years, his condition is stable in the outpatient clinic.
Case 5 A 9-year-old girl was suffering from cyanosis during sleep due to central hypopnea. She was born at the gestational age of 38 weeks and weighed 1786 g. She was diagnosed with ventricular septal defect, atrial septal defect and patent ductus arteriosus associated with trisomy 18. Further, she had micrognathia. She was conservatively treated according to her family’s decision, and she developed Eisenmenger syndrome with a systemic oxygen saturation of 80% until the age of 4 years. When she developed respiratory failure and hypercapnia due to respiratory infection, blood gas analysis showed PCO2 of 100 mmHg. She was then intubated and supported by mechanical ventilation for several days. After extubation, she presented remarkable cyanosis during sleep with systemic oxygen saturation below 50%. Therefore, we performed home HFNC with a flow rate of 13 L/min and an oxygen fraction of 0.4 using MediOx 60®. After the introduction of home HFNC, her cyanosis during sleep transiently subsided and blood gas showed PCO2 of 66 mmHg. Nonetheless, she required tracheostomy and home ventilation therapy due to persistence of central hypopnea at 10 years of age. She is stable with a systemic oxygen saturation of 84% in the outpatient clinic.
Discussion
We present a series of 5 cases with congenital heart disease who effectively and safely underwent home HFNC therapy due to respiratory problems. HFNC has been applied in a variety of disease conditions and age, and is characterized by less use of sedation and fewer complications [5, 6]. In this study, home HFNC was applied in 2 subjects with upper airway obstruction, 2 subjects with central hypopnea, and one subject with chronic respiratory failure due to respiratory infection. However, home HFNC was effective in all subjects, whatever the objectives of home HFNC were.
There are two methods of home HFNC therapy: a nasal prong is connected to a flow-dependent mechanical ventilator designed for home HFNC, such as MediOx 60®, and a flow is set at 1–3 L/kg/min. MediOx 60® offers both high-flow and positive pressure modes, and provides total breathing care for patients with different interfaces available to match a range of environments. However, because of limited battery, it cannot be used during patient’s transfer. Thus, a conventional home mechanical ventilator with CPAP mode, such as Trilogy 100 plus® or BiPAP A40®, can be alternatively used. CPAP mode is set at a pressure of 4–6 cnH2O with or without oxygen supplementation. However, there are several concerns: that an abnormal elevation of the set pressure may occur due to an obstruction of the cannula, and that a decrease in the intracircuit pressure according to the types of nasal prongs may enable to maintain a sufficient airway pressure in the patient. In our case series, as one subjects (Case 4) presented vomiting, probably due to aerophagia, a pressure-dependent ventilator was changed to a flow-dependent ventilator. As previous reports have shown that the frequency of nasal CPAP failure is higher in nasal prong than in nasal mask [5, 6, 9], which suggests an importance that care providers at home properly make sure the tolerability and certainty of home HFNC.
All subjects in our case series consisted of children with uncorrected CHD. Although limited information regarding hemodynamic effects on HFNC is available, HFNC supports respiration through direct delivery of gas at high-flow rates into the nasopharynx to create a reservoir of fresh gas and to reduce dead space, rather than through an increase in the end-expiratory pressure to increase lung volume, and thus its effect on pulmonary arterial pressure and central venous pressure are limited [6]. Recent reports have encouraged preferable effects on not only breathwork but also hemodynamics in children with CHD [6, 10, 11]. Kuwata et al. described a detailed hemodynamic change before and after HFNC in a child after a Fontan operation, which demonstrated a decrease in heart rate and pulmonary vascular resistance, and an increase in cardiac output without any change in central venous pressure [10]. Our present study suggested that HFNC seemed to improve vital signs and respiratory efforts with little effects on pulmonary hemodynamics even in children with cyanotic congenital heart disease or Eisenmenger syndrome.
This study has a considerable limitation. The number of subjects is too small to conclude the absolute feasibility and safety. Therefore, further studies are warranted to collect the definitive information about home HFNC therapy in children with CHD.
Conclusions
Home HFNC therapy is feasible and safe in children with CHD and respiratory problems, even when they have cyanotic or unrepaired CHD. Home HFNC should be further studied to achieve appropriate homecare among them.
Data Availability
All data will be offered if applicable.
Code Availability
Not applicable.
References
Iida C, Muneuchi J, Yamamoto J, Yokota C, Ohmura J, Kamimura T et al (2019) Impacts of surgical interventions on the long-term outcomes in individuals with trisomy. J Pediatr Surg 18:S0022-3468
Domingo L, Carey JC, Eckhauser A, Wilkes J, Menon SC (2019) Mortality and resource use following cardiac interventions in children with trisomy 13 and trisomy 18 and congenital heart disease. Pediatr Cardiol 40(2):349–356
Evans JM, Dharmar M, Meierhenry E, Marcin JP, Raff GW (2014) Association between Down syndrome and in-hospital death among children undergoing surgery for congenital heart disease: a US population-based study. Circ Cardiovasc Qual Outcomes 7:445–452
Franklin D, Babl FE, Schlapbach LJ, Oakley E, Craig S, Neutze J et al (2018) A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 378:1121–1131
Shioji N, Iwasaki T, Kanazawa T, Shimizu K, Suemori T, Sugimoto K et al (2017) Physiological impact of high-flow nasal cannula therapy on postextubation acute respiratory failure after pediatric cardiac surgery: a prospective observational study. J Intensive Care 5:35
Dysart K, Miller TL, Wolfson MR, Shaffer TH (2009) Research in high flow therapy: mechanisms of action. Respir Med 103:1400–1405
Hoffman SB, Terrell N, Driscoll CH, Davis NL (2016) Impact of high-flow nasal cannula use on neonatal respiratory support patterns and length of stay. Respir Care 61:1299–1304
Angoulvant F, Bellêttre X, Milcent K, Teglas JP, Claudet I, Le Guen CG et al (2017) Effect of nebulized hypertonic saline treatment in emergency departments on the hospitalization rate for acute bronchiolitis: a randomized clinical trial. JAMA Pediatr 171:e171333
Say B, Kanmaz Kutman HG, Oguz SS, Oncel MY, Arayici S, Canpolat FE et al (2016) Binasal prong versus nasal mask for applying cpap to preterm infants: a randomized controlled trial. Neonatology 109:258–264
Kuwata S, Kurishima C, Kim J, Iwamoto Y, Saiki H, Ishido H et al (2015) Clinical evaluation of the hemodynamic effects of the high-flow nasal cannula therapy on the fontan circulation. Clin Med Insights Cardiol 9:109–111
Inata Y, Takeuchi M (2017) Complex effects of high-flow nasal cannula therapy on hemodynamics in the pediatric patient after cardiac surgery. J Intensive Care 5:30
Funding
This research received no grant from any funding agency in the public, commercial of not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical Approval
This study is approval by the Institutional Review Board in Kyushu Hospital, Japan Community Healthcare Organization.
Consent to Participate
Consent to participate is waived because this study is retrospective study.
Consent for Publication
All authors approved this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hanaki, Y., Muneuchi, J., Yamamoto, J. et al. Home High-Flow Nasal Cannula Therapy in Children with Congenital Heart Disease. Pediatr Cardiol 43, 1131–1135 (2022). https://doi.org/10.1007/s00246-022-02834-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02834-y