Abstract
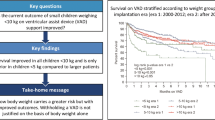
Pediatric ventricular assist device (VAD) implantation outcomes are increasingly promising for children with dilated cardiomyopathy and advanced decompensated heart failure (ADHF). VAD placement in patients with clinical features such as complex congenital cardiac anatomy, small body size, or major comorbidities remains problematic. These comorbidities have been traditionally prohibitive for VAD consideration leaving these children as a treatment-orphaned population. Here we describe the quality bundle surrounding these patients with ADHF considered high risk for VAD implantation at our institution. Over a 7-year period, a quality bundle aimed at the peri-operative care for children with high-risk features undergoing VAD implantation was incrementally implemented at a tertiary children’s hospital. Patients were considered high risk if they were neonates (< 30 days), had single-ventricle physiology, non-dilated cardiomyopathy, biventricular dysfunction, or significant comorbidities. The quality improvement bundle evolved to include (1) structured team-based peri-operative evaluation, (2) weekly VAD rounds addressing post-operative device performance, (3) standardized anticoagulation strategies, and (4) a multidisciplinary system for management challenges. These measures aimed to improve communication, standardize management, allow for ongoing process improvement, and incorporate principles of a high-reliability organization. Between January 2010 and December 2017, 98 patients underwent VAD implantation, 48 (49%) of which had high-risk comorbidities and a resultant cohort survival-to-transplant rate of 65%. We report on the evolution of a quality improvement program to expand the scope of VAD implantation to patients with high-risk clinical profiles. This quality bundle can serve as a template for future large-scale collaborations to improve outcomes in these treatment-orphaned subgroups.

Similar content being viewed by others

References
Fraser CD Jr, Jaquiss RD (2013) The Berlin heart EXCOR pediatric ventricular assist device: history, North American experience, and future directions. Ann N Y Acad Sci 1291:96–105
Blume ED, VanderPluym C, Lorts A et al (2018) Second annual pediatric interagency registry for mechanical circulatory support (Pedimacs) report: pre-implant characteristics and outcomes. J Heart Lung Transplant 37(1):38–45
Dipchand AI, Kirk R, Naftel DC et al (2018) Ventricular assist device support as a bridge to transplantation in pediatric patients. J Am Coll Cardiol 72(4):402–415
Burki S, Adachi I (2017) Pediatric ventricular assist devices: current challenges and future prospects. Vasc Health Risk Manag 13:177–185
Zafar F, Castleberry C, Khan MS et al (2015) Pediatric heart transplant waiting list mortality in the era of ventricular assist devices. J Heart Lung Transplant 34(1):82–88
Almond CS, Morales DL, Blackstone EH et al (2013) Berlin heart EXCOR pediatric ventricular assist device for bridge to heart transplantation in US children. Circulation 127(16):1702–1711
Maeda K, Rosenthal DN, Reinhartz O (2018) Ventricular assist devices for neonates and infants. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 21:9–14
Weinstein S, Bello R, Pizarro C, et al (2014) The use of the Berlin heart EXCOR in patients with functional single ventricle. J Thorac Cardiovasc Surg 147(2):697–704 (discussion 704–695).
Fraser CD Jr, Jaquiss RD, Rosenthal DN et al (2012) Prospective trial of a pediatric ventricular assist device. N Engl J Med 367(6):532–541
Magnetta DA, Kang J, Wearden PD, Smith KJ, Feingold B (2018) Cost-effectiveness of ventricular assist device destination therapy for advanced heart failure in duchenne muscular dystrophy. Pediatr Cardiol 39:1242–1248
Seguchi O, Kuroda K, Fujita T, Fukushima N, Nakatani T (2016) Advanced heart failure secondary to muscular dystrophy: clinical outcomes after left ventricular assist device implantation. J Heart Lung Transplant 35(6):831–834
Nunes AJ, Buchholz H, Sinnadurai S, MacArthur RG (2012) Long-term mechanical circulatory support of an adult patient with down syndrome. Ann Thorac Surg 93(4):1305–1307
Jeewa A, Manlhiot C, McCrindle BW, Van Arsdell G, Humpl T, Dipchand AI (2010) Outcomes with ventricular assist device versus extracorporeal membrane oxygenation as a bridge to pediatric heart transplantation. Artif Organs 34(12):1087–1091
Ford MA, Gauvreau K, McMullan DM et al (2016) Factors associated with mortality in neonates requiring extracorporeal membrane oxygenation for cardiac indications: analysis of the extracorporeal life support organization registry data. Pediatr Crit Care Med 17(9):860–870
Misfeldt AM, Kirsch RE, Goldberg DJ et al (2016) Outcomes of single-ventricle patients supported with extracorporeal membrane oxygenation. Pediatr Crit Care Med 17(3):194–202
Dipchand AI, Mahle WT, Tresler M et al (2015) Extracorporeal membrane oxygenation as a bridge to pediatric heart transplantation: effect on post-listing and post-transplantation outcomes. Circ Heart Fail 8(5):960–969
Alert SE (2017) Inadequate hand-off communication. Sentinel Event Alert 58:1–6.
Alvarez G, Coiera E (2006) Interdisciplinary communication: an uncharted source of medical error? J Crit Care 21(3):236–242 (discussion 242)
Ohno T (1988) Toyota production system: beyond large-scale production. Productivity Press, Portland
Hirano H, Furuya M (2006) JIT is flow: practice and principles of lean manufacturing. PCS Press, Inc, Portland
Wilson KA, Burke CS, Priest HA, Salas E (2005) Promoting health care safety through training high reliability teams. Qual Saf Health Care 14(4):303–309
Ke W, Km S (2007) Managing the unexpected: resilient performance in an age of uncertainty. Jossey-Bass, Portland
Massicotte MP, Bauman ME, Murray J, Almond CS (2015) Antithrombotic therapy for ventricular assist devices in children: do we really know what to do? J Thromb Haemost 13(Suppl 1):S343–350
Adachi I, Kostousov V, Hensch L, Chacon-Portillo MA, Teruya J (2018) Management of hemostasis for pediatric patients on ventricular-assist devices. Semin Thromb Hemost 44(1):30–37
Acknowledgements
The authors have no financial relationships relevant to this article to disclose.
Funding
No specific funding support was used for this quality report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Knoll, C., Chen, S., Murray, J.M. et al. A Quality Bundle to Support High-Risk Pediatric Ventricular Assist Device Implantation. Pediatr Cardiol 40, 1159–1164 (2019). https://doi.org/10.1007/s00246-019-02123-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02123-1


