Abstract
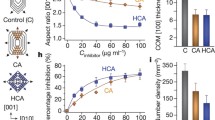
The formation of crystal aggregates, one of the critical processes in kidney stone pathogenesis, involves interactions between crystals (predominantly calcium oxalate monohydrate, COM) and urinary constituents (e.g., proteins), which serve as an adhesive “glue” between crystals in stones. To develop a better understanding of the protein–crystal interactions that lead to crystal aggregation, we have measured the effect of model proteins on bulk COM crystal properties as well as their adsorption on crystal surfaces using three synthetic polyanions: poly(aspartic acid) (polyD), poly(glutamic acid) (polyE), and poly(acrylic acid) (polyAA). These anionic macromolecules reduced the amount of COM crystal aggregation in bulk solution to an extent similar to that observed for mixture of proteins from normal urine, with little difference between the polymers. In contrast, the polymers exhibited differences in measures of COM crystal growth. Polycations such as poly(arginine) (polyR) and poly(lysine) (polyK) reduced aggregation weakly and exerted negligible effects on crystal growth. All polyions were found to associate with COM crystal surfaces, as evidenced by changes in the zeta potential of COM crystals in electrophoretic mobility measurements. On the other hand, COM aggregation and possibly growth can be promoted by many binary mixtures of polycations and polyanions, which appeared to be mediated by polymer aggregate formation rather than loss of crystal charge stabilization. Similarly, crystal aggregation promotion behavior can be driven by forming aggregates of weakly charged polyanions, like Tamm–Horsfall protein, suggesting that polymer (protein) aggregation may play a critical role in stone formation. Sensitivity of polyanion–COM crystal surface interactions to the chemical composition of polymer side groups were demonstrated by large differences in crystal aggregation behavior between polyD and polyE, which correlated with atomic force microscopy (AFM) measurements of growth inhibition on various COM surfaces and chemical force microscopy (CFM) measurements of unbinding forces between COM crystal surfaces and AFM tips decorated with either carboxylate or amidinium moieties (mimicking polyanion and polyR side chains, respectively). The lack of strong interaction for polyE at the COM (100) surface compared to polyD appeared to be the critical difference. Finally, the simultaneous presence of polyanions and polycations appeared to alter the ability of polycations to mediate unbinding forces in CFM and promote crystal growth. In summary, polyanions strongly associated with COM surfaces and influenced crystallization, while polycations did not, though important differences were observed based on the physicochemical properties of polyanions. Observations suggest that COM aggregation with both polyanion–polycation mixtures and weakly charged polyanions is promoted by polymer aggregate formation, which plays a critical role in bridging crystal surfaces.













Similar content being viewed by others
References
Aggarwal KP et al (2013) Nephrolithiasis: molecular mechanism of renal stone formation and the critical role played by modulators. Biomed Res Int. doi:10.1155/2013/292953
Kaiser ET, Bock SC (1989) Protein inhibitors of crystal-growth. J Urol 141(3):750–752
Kumar V, Lieske JC (2006) Protein regulation of intrarenal crystallization. Curr Opin Nephrol Hydrol 15(4):374–380
Ryall RL (1996) Glycosaminoglycans, proteins, and stone formation: adult themes and child’s play. Pediatr Nephrol 10(5):656–666
Boyce WH, Garvey FK (1956) The amount and nature of the organic matrix in urinary calculi: a review. J Urol 76(3):213–227
Gohel MDI, Shum DKY, Tam PC (2007) Electrophoretic separation and characterization of urinary glycosaminoglycans and their roles in urolithiasis. Carbohydr Res 342(1):79–86
Khan SR, Kok DJ (2004) Modulators of urinary stone formation. Front Biosci 9:1450–1482
Sallis JD (1987) Glycosaminoglycans as inhibitor of stone formation. Miner Electrolyte Metab 13(4):273–277
Verkoelen CF (2006) Crystal retention in renal stone disease: a crucial role for the glycosaminoglycan hyaluronan? J Am Soc Nephrol 17(6):1673–1687
Jariwalla RJ (2001) Rice-bran products: phytonutrients with potential applications in preventive and clinical medicine. Drug Exp Clin Res 27(1):17–26
Miyaoka R, Monga M (2009) Use of traditional Chinese medicine in the management of urinary stone disease. Int Br J Urol 35(4):396–405
Nasim MJ et al (2014) Gist of medicinal plants of Pakistan having ethnobotanical evidences to crush renal calculi (kidney stones). Acta Pol Pharm 71(1):3–10
Khan SR, Hackett RL (1987) Crystal-matrix relationships in experimentally induced urinary calcium-oxalate monohydrate crystals, an ultrastructural-study. Calssified Tissue Int 41(3):157–163
Boyce WH (1968) Organic matrix of human urinary concretions. Am J Med 45(5):673–683
Boyce WH, King JS (1963) 1. Some special aspects of metabolic dysfunction: present concepts concerning origin of matrix and stones. Ann N Y Acad Sci 104(2):563–578
Robertson WG, Peacock M, Nordin BEC (1968) Activity products in stone-forming and non-stone-forming urine. Clin Sci 34(3):579–594
Aggarwal KP et al (2013) Peeping into human renal calcium oxalate stone matrix: characterization of novel proteins involved in the intricate mechanism of urolithiasis. PLoS One 8(7):e69916. doi:10.1371/journal.pone.0069916
Aggarwal KP et al (2013) 2D map of proteins from human renal stone matrix and evaluation of their effect on oxalate induced renal tubular epithelial cell injury. Int Br J Urol 39(1):128–136
Boonla C et al (2014) Inflammatory and fibrotic proteins proteomically identified as key protein constituents in urine and stone matrix of patients with kidney calculi. Clin Chim Acta 429:81–89
Canales BK et al (2010) Proteome of human calcium kidney stones. Urology 76(4):1017.e13-20
Jou YC et al (2012) Proteomic study of renal uric acid stone. Urology 80(2):260–266
Kaneko K et al (2012) Comparison of matrix proteins in different types of urinary stone by proteomic analysis using liquid chromatography-tandem mass spectrometry. Int J Urol 19(8):765–772
Wu JQ, Gao YH (2015) Physiological conditions can be reflected in human urine proteome and metabolome. Exp Rev Proteomic 12(6):623–636
Okumura N et al (2013) Diversity in protein profiles of individual calcium oxalate kidney stones. PLoS One 8(7):e68624. doi:10.1371/journal.pone.0068624
Solis FJ (2002) Phase diagram of dilute polyelectrolytes: collapse and redissolution by association of counterions and co-ions. J Chem Phys 117(19):9009–9015
Manning GS (1978) Molecular theory of polyelectrolyte solutions with applications to electrostatic properties of polynucleotides. Q Rev Biophys 11(2):179–246
McKee MD, Nanci A (1996) Osteopontin at mineralized tissue interfaces in bone, teeth, and osseointegrated implants: ultrastructural distribution and implications for mineralized tissue formation, turnover, and repair. Microsc Res Tech 33(2):141–164
Paloian NJ, Giachelli CM (2014) A current understanding of vascular calcification in CKD. Am J Physiol Renal 307(8):F891–F900
Weiner S, Addadi L (1991) Acidic macromolecules of mineralized tissues—the controllers of crystal-formation. Trends Biochem Sci 16(7):252–256
Wesson JA, Ward MD (2007) Pathological biomineralization of kidney stones. Elements 3:415–421
Grover PK, Ryall RL (1999) Inhibition of calcium oxalate crystal growth and aggregation by prothrombin and its fragments in vitro—relationship between protein structure and inhibitory activity. Eur J Biochem 263(1):50–56
Hess B, Nakagawa Y, Coe FL (1989) Inhibition of calcium-oxalate monohydrate crystal aggregation by urine proteins. Am J Physiol 257(1):F99–F106
Lieske JC, Huang E, Toback FG (2000) Regulation of renal epithelial cell affinity for calcium oxalate monohydrate crystals. Am J Physiol-Renal 278(1):F130–F137
Springmann KE et al (1986) Effects of human-urine on aggregation of calcium-oxalate crystals. J Urol 135(1):69–71
Christmas KG et al (2002) Aggregation and dispersion characteristics of calcium oxalate monohydrate: effect of urinary species. J Colloid Interface Sci 256(1):168–174
Govindaraj A, Selvam R (2001) Increased calcium oxalate crystal nucleation and aggregation by peroxidized protein of human kidney stone matrix and renal cells. Urol Res 29(3):194–198
Grases F, Gil JJ, Conte A (1989) Glycosaminoglycans—inhibition of calcium-oxalate crystalline growth and promotion of crystal aggregation. Colloid Surface 36(1):29–38
Bigelow MW et al (1997) Surface exposure of phosphatidylserine increases calcium oxalate crystal attachment to IMCD cells. Am J Physiol Renal 41(1):F55–F62
Worcester EM (1996) Inhibitors of stone formation. Semin Nephrol 16(5):474–486
Shiraga H et al (1992) Inhibition of calcium-oxalate crystal-growth invitro by uropontin—another member of the aspartic acid-rich protein superfamily. Proc Natl Acad Sci USA 89(1):426–430
Ito H, Coe FL (1977) Acidic peptide and polyribonucleotide crystal-growth inhibitors in human urine. Am J Physiol 233(5):F455–F463
Worcester EM et al (1992) The calcium-oxalate crystal growth inhibitor protein produced by mouse kidney cortical-cells in culture is osteopontin. J Bone Miner Res 7(9):1029–1036
Wesson JA, Worcester E (1996) Formation of hydrated calcium oxalates in the presence of poly-l-aspartic acid. Scanning Microsc 10(2):415–423
Prien EL (1963) Crystallographic analysis of urinary calculi—a 23 year survey study. J Urol 89(6):917–924
Kohri K et al (2012) Biomolecular mechanism of urinary stone formation involving osteopontin. Urol Res 40(6):623–637
Kumar V et al (2003) Annexin II is present on renal epithelial cells and binds calcium oxalate monohydrate crystals. J Am Soc Nephrol 14(2):289–297
Sorokina EA, Wesson JA, Kleinman JG (2004) An acidic peptide sequence of nucleolin-related protein can mediate the attachment of calcium oxalate to renal tubule cells. J Am Soc Nephrol 15(8):2057–2065
Pragasam V et al (2011) Calcium oxalate monohydrate aggregation is induced by desialylated Tamm–Horsfall protein. Urol Res 39:269–282
Wesson JA et al (2005) Regulation by macromolecules of calcium oxalate crystal aggregation in stone formers. Urol Res 33(3):206–212
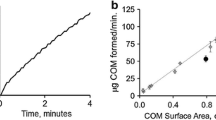
Jung T et al (2004) Probing crystallization of calcium oxalate monohydrate and the role of macromolecule additives with in situ atomic force microscopy. Langmuir 20(20):8587–8596
Farmanesh S et al (2014) Natural promoters of calcium oxalate monohydrate crystallization. J Am Chem Soc 136(36):12648–12657
Sheng XX et al (2005) Adhesion at calcium oxalate crystal surfaces and the effect of urinary constituents. Proc Natl Acad Sci USA 102(2):267–272
Hutter JL, Bechhoefer J (1993) Calibration of atomic-force microscope tips. Rev Sci Instrum 64(7):1868–1873
Priftis D, Tirrell M (2012) Phase behaviour and complex coacervation of aqueous polypeptide solutions. Soft Matter 8(36):9396–9405
Johnston APR et al (2006) Layer-by-layer engineered capsules and their applications. Curr Opin Colloid Interface 11(4):203–209
Decher G (1997) Fuzzy nanoassemblies: toward layered polymeric multicomposites. Science 277(5330):1232–1237
Tang ZY et al (2006) Biomedical applications of layer-by-layer assembly: from biomimetics to tissue engineering. Adv Mater 18(24):3203–3224
Lowack K, Helm CA (1998) Molecular mechanisms controlling the self-assembly process of polyelectrolyte multilayers. Macromolecules 31(3):823–833
Decher G, Hong JD, Schmitt J (1992) Buildup of ultrathin multilayer films by a self-assembly process. 3. Consecutively alternating adsorption of anionic and cationic polyelectrolytes on charged surfaces. Thin Solid Films 210(1–2):831–835
Gower LB (2008) Biomimetic model systems for investigating the amorphous precursor pathway and its role in biomineralization. Chem Rev 108(11):4551–4627
Kolbach-Mandel A, Kleinman J, Wesson J (2015) Exploring calcium oxalate crystallization: a constant composition approach. Urolithiasis 43(5):397–409
Benkovic J et al (1995) Effect of Tamm–Horsfall protein on calcium-oxalate precipitation. Eur J Clin Chem Clin 33(10):705–710
Hallson PC, Rose GA (1979) Uromucoids and urinary stone formation. Lancet 1(8124):1000–1002
Hess B et al (1991) Molecular abnormality of Tamm-Horsfall glycoprotein in calcium-oxalate nephrolithiasis. Am J Physiol 260(4):F569–F578
Mo L et al (2007) Renal calcinosis and stone formation in mice lacking osteopontin, Tamm–Horsfall protein, or both. Am J Physiol-Renal 293(6):F1935–F1943
Scurr DS, Robertson WG (1986) Modifiers of calcium-oxalate crystallization found in urine. 3. Studies on the role of Tamm–Horsfall mucoprotein and of ionic-strength. J Urol 136(2):505–507
Ronco P et al (1987) Physiopathologic aspects of Tamm-Horsfall protein: a phylogenetically conserved marker of the thick ascending limb of Henle’s loop. Adv Nephrol Necker Hosp 16:231–249
Wesson JA, Worcester EM, Kleinman JG (2000) Role of anionic proteins in kidney stone formation: interaction between model anionic polypeptides and calcium oxalate crystals. J Urol 163(4):1343–1348
Amjad Z, Koutsoukos PG (2014) Impact of surfactants on the performance of “Green Additives” as calcium carbonate inhibitors for aqueous systems. Tenside Surfact Det 51(1):40–45
Mandel NS, Mandel GS (1989) Urinary-tract stone disease in the United-States veteran population. 2. Geographical analysis of variations in composition. J Urol 142(6):1516–1521
Schubert G (2006) Stone analysis. Urol Res 34(2):146–150
Wesson JA, Ward MD (2006) Role of crystal surface adhesion in kidney stone disease. Curr Opin Nephrol Hydrol 15(4):386–393
Sheng X (2004) Face-specific molecular adhesion and binding to calcium oxalate monohydrate: implication for kidney stone disease. Dissertation, University of Minnesota-Minneapolis, MN p 127
Wesson JA et al (2003) Osteopontin is a critical inhibitor of calcium oxalate crystal formation and retention in renal tubules. J Am Soc Nephrol 14(1):139–147
Wesson JA et al (2002) Osteopontin in nephrolithiasis. J Am Soc Nephrol 13:574A–575A
Farmanesh S et al (2014) Specificity of growth inhibitors and their cooperative effects in calcium oxalate monohydrate crystallization. J Am Chem Soc 136:367–376
De Yoreo JJ, Qiu SR, Hoyer JR (2006) Molecular modulation of calcium oxalate crystallization. Am J Physiol-Renal 291(6):F1123–F1131
Wang LJ et al (2008) Phosphorylation of osteopontin is required for inhibition of calcium oxalate crystallization. J Phys Chem B 112(30):9151–9157
Grohe B et al (2007) Control of calcium oxalate crystal growth by face-specific adsorption of an osteopontin phosphopeptide. J Am Chem Soc 129(48):14946–14951
Hunter GK et al (2009) Role of phosphate groups in inhibition of calcium oxalate crystal growth by osteopontin. Cell Tissue Org 189(1–4):44–50
O’Young J et al (2009) Phosphorylation of osteopontin peptides mediates adsorption to and incorporation into calcium oxalate crystals. Cell Tissue Org 189(1–4):51–55
Farmanesh S et al (2013) High-throughput platform for design and screening of peptides as inhibitors of calcium oxalate monohydrate crystallization. J Cryst Growth 373:13–19
Wang LJ et al (2006) Modulation of calcium oxalate crystallization by linear aspartic acid-rich peptides. Langmuir 22(17):7279–7285
Chen CL et al (2014) Tuning calcite morphology and growth acceleration by a rational design of highly stable protein-mimetics. Sci Rep 4:6266. doi:10.1038/srep06266
Anderson NG, Anderson NL, Tollaksen SL (1979) Proteins of human-urine. 1. Concentration and analysis by 2-dimensional electrophoresis. Clin Chem 25(7):1199–1210
Hiemenz PC, Rajagopalan R (1997) Principles of colloid and surface chemistry, 3rd rev. and expanded/ed. Marcel Dekker, New York, p xix, 650
Bohmer MR, Evers OA, Scheutjens J (1990) Weak polyelectrolytes between 2 surfaces—adsorption and stabilization. Macromolecules 23(8):2288–2301
Cheng H et al (2006) Polynucleotide adsorption to negatively charged surfaces in divalent salt solutions. Biophys J 90(4):1164–1174
Hansma HG et al (1992) Reproducible imaging and dissection of plasmid DNA under liquid with the atomic force microscope. Science 256(5060):1180–1184
Pastre D et al (2003) Adsorption of DNA to mica mediated by divalent counterions: a theoretical and experimental study. Biophys J 85(4):2507–2518
Scheutjens J, Fleer GJ (1980) Statistical theory of the adsorption of interacting chain molecules. 2. Train, loop, and tail size distribution. J Phys Chem 84(2):178–190
Vanderschee HA, Lyklema J (1984) A lattice theory of polyelectrolyte adsorption. J Phys Chem 88(26):6661–6667
Hess B (1994) Tamm–Horsfall glycoprotein and calcium nephrolithiasis. Miner Electrol Metab 20(6):393–398
Kabanov AV, Kabanov VA (1998) Interpolyelectrolyte and block ionomer complexes for gene delivery: physicochemical aspects. Adv Drug Deliver Rev 30(1–3):49–60
Acknowledgements
We gratefully acknowledge the financial support provided by the Department of Veterans Affairs through their Research Career Development and Merit Review Programs (RCD and MR 9305 JAW) and in part with resources and the use of facilities at the Clement J. Zablocki Department of Veterans Affairs Medical Center, Milwaukee, WI. Funding was also obtained through parts of several grants from the National Institutes of Health/National Institute for Diabetes, Digestive, and Kidney Diseases (DK 68551, 74741, and 82550-JAW). Additional financial support was provided by the Medical College of Wisconsin Jacob Lemann Endowment Grant, the Materials Research Science and Engineering Center (MRSEC) program of the National Science Foundation under Award Number DMR-1420073 (MDW), the Welch Foundation under Award Number E-1794 (JDR), and the National Science Foundation under Award Number 1207441 (JDR). We also gratefully acknowledge the technical support from MIS.MAC (Mandel International Stone and Molecular Analysis Center), Milwaukee, WI, for crystal analysis through Dr. Neil Mandel, as well as particular contributions from Dr. William Zachowicz to ζ-potential measurements and Samuel Cohen to polyanion–polycation aggregation experiments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflicts of interest to report.
Funding
This study which spanned many years was funded with grants for the Department of Veterans Affairs Career Development and Merit Review programs (RCD and MR 9305 - JAW) and the use of facilities at the Clement J. Zablocki Department of Veterans Affairs Medical Center, Milwaukee, WI, and in part by grants from the National Institutes of Health (NIDDK, DK 68551, 74741, and 82550 - JAW). Additional financial support was provided by the Medical College of Wisconsin Jacob Lemann Endowment Grant and the Materials Research Science and Engineering Center (MRSEC) program of the National Science Foundation under Award Number DMR-1420073 (MDW).
Human studies
The participating patient in this study was recruited with informed consent to an established study under VA IRB approval (VA-IRB Protocol: 9305-01P). All procedures performed in these studies were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments.
Additional information
Submitted to Special Issue of Urolithiasis on the “Physico-chemical, Biochemical and Biological Mechanisms of Stone-Formation” November 24, 2016.
Rights and permissions
About this article
Cite this article
Rimer, J.D., Kolbach-Mandel, A.M., Ward, M.D. et al. The role of macromolecules in the formation of kidney stones. Urolithiasis 45, 57–74 (2017). https://doi.org/10.1007/s00240-016-0948-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-016-0948-8