Abstract
Purpose
To evaluate the incremental value of amide proton transfer (APT) imaging to diffusion tensor imaging (DTI), dynamic susceptibility contrast (DSC) imaging, and dynamic contrast-enhanced (DCE) imaging in differentiating recurrent diffuse gliomas (World Health Organization grade II-IV) from treatment-induced change after concurrent chemoradiotherapy or radiotherapy.
Methods
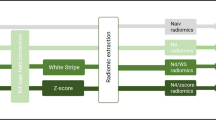
This study included 36 patients (25 patients with recurrent gliomas and 11 with treatment-induced changes) with post-treatment gliomas. The mean values of apparent diffusion coefficient (ADC), fractional anisotropy (FA), normalized cerebral blood volume (nCBV), normalized cerebral blood flow, volume transfer constant, rate transfer coefficient, extravascular extracellular volume fraction, plasma volume fraction, and APT asymmetry index were assessed. Independent quantitative parameters were investigated to predict recurrent glioma using multivariable logistic regression. The incremental value of APT signal to other parameters was assessed by the increase of the area under the curve, net reclassification index, and integrated discrimination improvement.
Results
Univariable analysis showed that lower ADC (p = 0.018), higher FA (p = 0.031), higher nCBV (p = 0.021), and higher APT signal (p = 0.009) were associated with recurrent gliomas. In multivariable logistic regression, the diagnostic performance of the model with ADC, FA, and nCBV significantly increased when APT signal was added, with areas under the curve of 0.87 and 0.92, respectively (net reclassification index of 0.77 and integrated discrimination improvement of 0.13).
Conclusion
APT imaging may be a useful imaging biomarker that adds value to DTI, DCE, and DSC parameters for distinguishing between recurrent gliomas and treatment-induced changes.




Similar content being viewed by others
Data availability
Our anonymized data can be obtained by any qualified investigator for the purposes of replicating procedures and results after ethics clearance and approval by all authors.
References
Burger PC, Mahaley MS Jr, Dudka L, Vogel FS (1979) The morphologic effects of radiation administered therapeutically for intracranial gliomas. A postmortem study of 25 cases. Cancer 44(4):1256–1272
Haider AS, van den Bent M, Wen PY, Vogelbaum MA, Chang S, Canoll PD, Horbinski CM, Huse JT (2020) Toward a standard pathological and molecular characterization of recurrent glioma in adults: a response assessment in neuro-oncology effort. Neuro-Oncology 22(4):450–456. https://doi.org/10.1093/neuonc/noz233
Xu J-L, Li Y-L, Lian J-M, S-w D, Yan F-S, Wu H, D-p S (2010) Distinction between postoperative recurrent glioma and radiation injury using MR diffusion tensor imaging. Neuroradiology 52(12):1193–1199
Wang S, Martinez-Lage M, Sakai Y, Chawla S, Kim SG, Alonso-Basanta M, Lustig RA, Brem S, Mohan S, Wolf RL, Desai A, Poptani H (2016) Differentiating tumor progression from pseudoprogression in patients with glioblastomas using diffusion tensor imaging and dynamic susceptibility contrast MRI. AJNR Am J Neuroradiol 37(1):28–36. https://doi.org/10.3174/ajnr.A4474
Wang S, Chen Y, Lal B, Ford E, Tryggestad E, Armour M, Yan K, Laterra J, Zhou J (2012) Evaluation of radiation necrosis and malignant glioma in rat models using diffusion tensor MR imaging. J Neuro-Oncol 107(1):51–60. https://doi.org/10.1007/s11060-011-0719-x
Gahramanov S, Muldoon LL, Varallyay CG, Li X, Kraemer DF, Fu R, Hamilton BE, Rooney WD, Neuwelt EA (2013) Pseudoprogression of glioblastoma after chemo- and radiation therapy: diagnosis by using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging with ferumoxytol versus gadoteridol and correlation with survival. Radiology 266(3):842–852. https://doi.org/10.1148/radiol.12111472
Chung WJ, Kim HS, Kim N, Choi CG, Kim SJ (2013) Recurrent glioblastoma: optimum area under the curve method derived from dynamic contrast-enhanced T1-weighted perfusion MR imaging. Radiology 269(2):561–568. https://doi.org/10.1148/radiol.13130016
Larsen VA, Simonsen HJ, Law I, Larsson HB, Hansen AE (2013) Evaluation of dynamic contrast-enhanced T1-weighted perfusion MRI in the differentiation of tumor recurrence from radiation necrosis. Neuroradiology 55(3):361–369. https://doi.org/10.1007/s00234-012-1127-4
Knutsson L, Xu J, Ahlgren A, van Zijl PCM (2018) CEST, ASL, and magnetization transfer contrast: How similar pulse sequences detect different phenomena. Magn Reson Med 80(4):1320–1340. https://doi.org/10.1002/mrm.27341
Suh CH, Park JE, Jung SC, Choi CG, Kim SJ, Kim HS (2019) Amide proton transfer-weighted MRI in distinguishing high- and low-grade gliomas: a systematic review and meta-analysis. Neuroradiology 61(5):525–534. https://doi.org/10.1007/s00234-018-02152-2
Park JE, Kim HS, Park KJ, Kim SJ, Kim JH, Smith SA (2016) Pre- and posttreatment glioma: comparison of amide proton transfer imaging with MR spectroscopy for biomarkers of tumor proliferation. Radiology 278(2):514–523. https://doi.org/10.1148/radiol.2015142979
Park JE, Lee JY, Kim HS, Oh JY, Jung SC, Kim SJ, Keupp J, Oh M, Kim JS (2018) Amide proton transfer imaging seems to provide higher diagnostic performance in post-treatment high-grade gliomas than methionine positron emission tomography. Eur Radiol 28(8):3285–3295. https://doi.org/10.1007/s00330-018-5341-2
Park KJ, Kim HS, Park JE, Shim WH, Kim SJ, Smith SA (2016) Added value of amide proton transfer imaging to conventional and perfusion MR imaging for evaluating the treatment response of newly diagnosed glioblastoma. Eur Radiol 26(12):4390–4403. https://doi.org/10.1007/s00330-016-4261-2
Ellingson BM, Bendszus M, Boxerman J, Barboriak D, Erickson BJ, Smits M, Nelson SJ, Gerstner E, Alexander B, Goldmacher G, Wick W, Vogelbaum M, Weller M, Galanis E, Kalpathy-Cramer J, Shankar L, Jacobs P, Pope WB, Yang D, Chung C, Knopp MV, Cha S, van den Bent MJ, Chang S, Yung WK, Cloughesy TF, Wen PY, Gilbert MR (2015) Consensus recommendations for a standardized brain tumor imaging protocol in clinical trials. Neuro-Oncology 17(9):1188–1198. https://doi.org/10.1093/neuonc/nov095
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820
Takano S, Tian W, Matsuda M, Yamamoto T, Ishikawa E, Kaneko MK, Yamazaki K, Kato Y, Matsumura AJB (2011) Detection of IDH1 mutation in human gliomas: comparison of immunohistochemistry and sequencing. Brain Tumor Pathol 28(2):115–123
Brandes AA, Franceschi E, Tosoni A, Blatt V, Pession A, Tallini G, Bertorelle R, Bartolini S, Calbucci F, Andreoli AJJCO (2008) MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol 26(13):2192–2197
Tofts PS, Brix G, Buckley DL, Evelhoch JL, Henderson E, Knopp MV, Larsson HB, Lee TY, Mayr NA, Parker GJ, Port RE, Taylor J, Weisskoff RM (1999) Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging 10(3):223–232. https://doi.org/10.1002/(sici)1522-2586(199909)10:3<223::aid-jmri2>3.0.co;2-s
Weisskoff R, Boxerman J, Sorensen A, Kulke S, Campbell T, Rosen B (1994) Simultaneous blood volume and permeability mapping using a single Gd-based contrast injection. In: Proceedings of the Society of Magnetic Resonance. Second Annual Meeting, pp 6–12
Boxerman JL, Schmainda KM, Weisskoff RM (2006) Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 27(4):859–867
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Pencina MJ, D'Agostino RB Sr, Demler OV (2012) Novel metrics for evaluating improvement in discrimination: net reclassification and integrated discrimination improvement for normal variables and nested models. Stat Med 31(2):101–113. https://doi.org/10.1002/sim.4348
Zhou J, Tryggestad E, Wen Z, Lal B, Zhou T, Grossman R, Wang S, Yan K, Fu DX, Ford E, Tyler B, Blakeley J, Laterra J, van Zijl PC (2011) Differentiation between glioma and radiation necrosis using molecular magnetic resonance imaging of endogenous proteins and peptides. Nat Med 17(1):130–134. https://doi.org/10.1038/nm.2268
Shah R, Vattoth S, Jacob R, Manzil FFP, O’Malley JP, Borghei P, Patel BN, Curé JK (2012) Radiation necrosis in the brain: imaging features and differentiation from tumor recurrence. Radiographics 32(5):1343–1359
Al Sayyari A, Buckley R, McHenery C, Pannek K, Coulthard A, Rose S (2010) Distinguishing recurrent primary brain tumor from radiation injury: a preliminary study using a susceptibility-weighted MR imaging-guided apparent diffusion coefficient analysis strategy. AJNR Am J Neuroradiol 31(6):1049–1054. https://doi.org/10.3174/ajnr.A2011
Thomas AA, Arevalo-Perez J, Kaley T, Lyo J, Peck KK, Shi W, Zhang Z, Young RJ (2015) Dynamic contrast enhanced T1 MRI perfusion differentiates pseudoprogression from recurrent glioblastoma. J Neuro-Oncol 125(1):183–190. https://doi.org/10.1007/s11060-015-1893-z
Zakhari N, Taccone MS, Torres CH, Chakraborty S, Sinclair J, Woulfe J, Jansen GH, Cron GO, Thornhill RE, McInnes MDF, Nguyen TB (2019) Prospective comparative diagnostic accuracy evaluation of dynamic contrast-enhanced (DCE) vs. dynamic susceptibility contrast (DSC) MR perfusion in differentiating tumor recurrence from radiation necrosis in treated high-grade gliomas. J Magn Reson Imaging 50(2):573–582. https://doi.org/10.1002/jmri.26621
Kim HS, Goh MJ, Kim N, Choi CG, Kim SJ, Kim JH (2014) Which combination of MR imaging modalities is best for predicting recurrent glioblastoma? Study of diagnostic accuracy and reproducibility. Radiology 273(3):831–843. https://doi.org/10.1148/radiol.14132868
Yun TJ, Park CK, Kim TM, Lee SH, Kim JH, Sohn CH, Park SH, Kim IH, Choi SH (2015) Glioblastoma treated with concurrent radiation therapy and temozolomide chemotherapy: differentiation of true progression from pseudoprogression with quantitative dynamic contrast-enhanced MR imaging. Radiology 274(3):830–840. https://doi.org/10.1148/radiol.14132632
Seeger A, Braun C, Skardelly M, Paulsen F, Schittenhelm J, Ernemann U, Bisdas S (2013) Comparison of three different MR perfusion techniques and MR spectroscopy for multiparametric assessment in distinguishing recurrent high-grade gliomas from stable disease. Acad Radiol 20(12):1557–1565. https://doi.org/10.1016/j.acra.2013.09.003
Shin KE, Ahn KJ, Choi HS, Jung SL, Kim BS, Jeon SS, Hong YG (2014) DCE and DSC MR perfusion imaging in the differentiation of recurrent tumour from treatment-related changes in patients with glioma. Clin Radiol 69(6):e264–e272. https://doi.org/10.1016/j.crad.2014.01.016
Fatterpekar GM, Galheigo D, Narayana A, Johnson G, Knopp E (2012) Treatment-related change versus tumor recurrence in high-grade gliomas: a diagnostic conundrum--use of dynamic susceptibility contrast-enhanced (DSC) perfusion MRI. AJR Am J Roentgenol 198(1):19–26. https://doi.org/10.2214/ajr.11.7417
Cha J, Kim ST, Kim HJ, Kim BJ, Kim YK, Lee JY, Jeon P, Kim KH, Kong DS, Nam DH (2014) Differentiation of tumor progression from pseudoprogression in patients with posttreatment glioblastoma using multiparametric histogram analysis. AJNR Am J Neuroradiol 35(7):1309–1317. https://doi.org/10.3174/ajnr.A3876
Hu LS, Baxter LC, Smith KA, Feuerstein BG, Karis JP, Eschbacher JM, Coons SW, Nakaji P, Yeh RF, Debbins J, Heiserman JE (2009) Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements. AJNR Am J Neuroradiol 30(3):552–558. https://doi.org/10.3174/ajnr.A1377
Xu JL, Shi DP, Dou SW, Li YL, Yan FS (2011) Distinction between postoperative recurrent glioma and delayed radiation injury using MR perfusion weighted imaging. J Med Imaging Radiat Oncol 55(6):587–594. https://doi.org/10.1111/j.1754-9485.2011.02315.x
Zhou J, Tryggestad E, Wen Z, Lal B, Zhou T, Grossman R, Wang S, Yan K, Fu D-X, Ford E (2011) Differentiation between glioma and radiation necrosis using molecular magnetic resonance imaging of endogenous proteins and peptides. Nat Med 17(1):130–134
Heo HY, Lee DH, Zhang Y, Zhao X, Jiang S, Chen M, Zhou J (2017) Insight into the quantitative metrics of chemical exchange saturation transfer (CEST) imaging. Magn Reson Med 77(5):1853–1865. https://doi.org/10.1002/mrm.26264
Lee DH, Heo HY, Zhang K, Zhang Y, Jiang S, Zhao X, Zhou J (2017) Quantitative assessment of the effects of water proton concentration and water T(1) changes on amide proton transfer (APT) and nuclear overhauser enhancement (NOE) MRI: The origin of the APT imaging signal in brain tumor. Magn Reson Med 77(2):855–863. https://doi.org/10.1002/mrm.26131
Funding
This research received funding from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science, Information and Communication Technologies and Future Planning (2014R1A1A1002716, 2020R1A2C1003886). This research was also supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2020R1I1A1A01071648).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this retrospective study, formal consent was not required.
Consent to participate
As this is a retrospective study, the institutional review board waived the need for obtaining informed patient consent.
Consent for publication
All of the authors gave consent for publication of the article.
Code availability
The Matlab (MathWorks, Natick, MA) code for amide proton transfer image processing can be obtained by any qualified investigator for the purposes of replicating procedures and results after approval by all authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Park, Y.W., Ahn, S.S., Kim, E.H. et al. Differentiation of recurrent diffuse glioma from treatment-induced change using amide proton transfer imaging: incremental value to diffusion and perfusion parameters. Neuroradiology 63, 363–372 (2021). https://doi.org/10.1007/s00234-020-02542-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02542-5