Abstract
Purpose
Ligamentum flavum is one of the structures that could compress the spinal canal. Few studies have reported atrophy of ligamentum flavum after spinal fusion. The purpose of this study was to demonstrate the reduction of ligamentum flavum size after oblique lumbar interbody fusion (OLIF) using magnetic resonance imaging (MRI).
Method
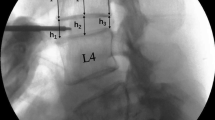
Seventeen patients who underwent OLIF without direct decompression were included. The MRI was obtained at the preoperative period, immediate postoperative period, and the follow-up period. Disc height (DH) was measured in plain radiograph. MRI measurements were spinal canal cross-sectional area (SCSA), ligamentum flavum thickness (LFT), ligamentum flavum area (LFA), and foraminal area (FA).
Results
Mean age of the patients was 68.5 ± 10.8. Mean times between postoperative MRI and follow-up MRI were 20.2 ± 11.9 months. Mean disc height increased from 7.6 ± 1.6 to 11.6 ± 1.7 mm at an immediate postoperative period but decreased to 10.1 ± 1.6 mm during follow-up (p < 0.001). SCSA increased from 96.9 ± 54.9 to 136.0 ± 72.7 mm2 and 171.4 ± 76.10 mm2 during follow-up (p < 0.001). LFT decreased from 3.9 ± 1.2 to 3.2 ± 0.8 mm (17.9%) and further decreased to 2.9 ± 0.7 mm during follow-up (9.4%) (p < 0.001). LFA decreased from 97.4 ± 36.9 to 86.1 ± 36.9 mm2 (11.6%) and further decreased to 77.2 ± 32.5 mm2 during follow-up (10.3%) (p = 0.001). FA increased from 69.2 ± 26.6 to 96.1 ± 23.0 mm2 and increased to 112.9 ± 23.0 mm2 during follow-up (p < 0.001).
Conclusion
OLIF could decompress the spinal canal and foraminal canal indirectly. Despite the diminishing disc height during the follow-up period, the spinal canal was further increased in size from the remodeling of the ligamentum flavum.







Similar content being viewed by others
Change history
07 July 2020
In the article "Decreasing Thickness and Remodeling of Ligamentum Flavum After Oblique Lumbar Interbody Fusion���, Figure 2 captions contained mistakes as descriptions for the Figure sections were not assigned correctly.
References
Kobayashi K, Ando K, Nishida Y, Ishiguro N, Imagama S (2018) Epidemiological trends in spine surgery over 10 years in a multicenter database. Eur Spine J 27(8):1698–1703. https://doi.org/10.1007/s00586-018-5513-4
Yoshiiwa T, Miyazaki M, Notani N, Ishihara T, Kawano M, Tsumura H (2016) Analysis of the relationship between ligamentum flavum thickening and lumbar segmental instability, disc degeneration, and facet joint osteoarthritis in lumbar spinal stenosis. Asian Spine J 10(6):1132–1140. https://doi.org/10.4184/asj.2016.10.6.1132
Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Fujimoto K, Shiga Y, Abe K, Kanamoto H, Inoue G, Takahashi K (2017) Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J 26(3):671–678. https://doi.org/10.1007/s00586-015-4170-0
Webb M, Eby M, Murray M (2018) Indirect decompression progresses substantially after immediate postoperative period following lateral lumbar interbody fusion. Univ Pennsylvania Orthopaedic J 28(1)
Ohtori S, Orita S, Yamauchi K, Eguchi Y, Aoki Y, Nakamura J, Miyagi M, Suzuki M, Kubota G, Inage K, Sainoh T, Sato J, Fujimoto K, Shiga Y, Abe K, Kanamoto H, Inoue G, Takahashi K, Furuya T, Koda M (2017) Change of lumbar ligamentum flavum after indirect decompression using anterior lumbar interbody fusion. Asian Spine J 11(1):105–112. https://doi.org/10.4184/asj.2017.11.1.105
Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L (2013) Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion clinical article. J Neurosurg-Spine 19(1):110–118. https://doi.org/10.3171/2013.4.Spine12319
Oliveira L, Marchi L, Coutinho E, Pimenta L (2010) A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976) 35(26 Suppl):S331–S337. https://doi.org/10.1097/BRS.0b013e3182022db0
Lang G, Perrech M, Navarro-Ramirez R, Hussain I, Pennicooke B, Maryam F, Avila MJ, Härtl R (2017) Potential and limitations of neural decompression in extreme lateral interbody fusion—a systematic review. World Neurosurg 101:99–113. https://doi.org/10.1016/j.wneu.2017.01.080
Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S (2015) Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 40 (3):E175–E182. doi:https://doi.org/10.1097/BRS.0000000000000703
Sairyo K, Biyani A, Goel V, Leaman D, Booth R, Thomas J, Gehling D, Vishnubhotla L, Long R, Ebraheim N (2005) Pathomechanism of ligamentum flavum hypertrophy: a multidisciplinary investigation based on clinical, biomechanical, histologic, and biologic assessments. Spine 30(23):2649–2656. https://doi.org/10.1097/01.brs.0000188117.77657.ee
Jirathanathornnukul N, Limthongkul W, Yingsakmongkol W, Singhatanadgige W, Parkpian V, Honsawek S (2016) Increased expression of vascular endothelial growth factor is associated with hypertrophic ligamentum flavum in lumbar spinal canal stenosis. J Investig Med 64(4):882–887. https://doi.org/10.1136/jim-2015-000024
Honsawek S, Poonpukdee J, Chalermpanpipat C, Payungporn S, Limthongkul W, Yingsakmongkol W, Thanakit V, Parkpian V (2013) Hypertrophy of the ligamentum flavum in lumbar spinal canal stenosis is associated with increased bFGF expression. Int Orthop 37(7):1387–1392. https://doi.org/10.1007/s00264-013-1864-y
Yoshiiwa T, Miyazaki M, Notani N, Ishihara T, Kawano M, Tsumura H (2016) Analysis of the relationship between ligamentum flavum thickening and lumbar segmental instability, disc degeneration, and facet joint osteoarthritis in lumbar spinal stenosis. Asian Spine J 10(6):1132–1140. https://doi.org/10.4184/asj.2016.10.6.1132
Altinkaya N, Yildirim T, Demir S, Alkan O, Sarica FB (2011) Factors associated with the thickness of the ligamentum flavum: is ligamentum flavum thickening due to hypertrophy or buckling? Spine (Phila Pa 1976) 36 (16):E1093–E1097. doi:https://doi.org/10.1097/BRS.0b013e318203e2b5
Hur JW, Kim BJ, Park JH, Kim JH, Park YK, Kwon TH, Moon HJ (2015) The mechanism of ligamentum flavum hypertrophy: introducing angiogenesis as a critical link that couples mechanical stress and hypertrophy. Neurosurgery 77(2):274–281; discussion 281-272. https://doi.org/10.1227/NEU.0000000000000755
Moon HJ, Park YK, Ryu Y, Kim JH, Kwon TH, Chung HS, Kim JH (2012) The Angiogenic capacity from ligamentum flavum subsequent to inflammation a critical component of the pathomechanism of hypertrophy. Spine 37(3):E147–E155. https://doi.org/10.1097/BRS.0b013e3182269b19
Goel A, Nadkarni T, Shah A, Rai S, Rangarajan V, Kulkarni A (2015) Is only stabilization the ideal treatment for ossified posterior longitudinal ligament? Report of early results with a preliminary experience in 14 patients. World Neurosurg 84(3):813–819. https://doi.org/10.1016/j.wneu.2015.05.017
Koda M, Furuya T, Okawa A, Aramomi M, Inada T, Kamiya K, Ota M, Maki S, Ikeda O, Takahashi K, Mannoji C, Yamazaki M (2015) Bone union and remodelling of the non-ossified segment in thoracic ossification of the posterior longitudinal ligament after posterior decompression and fusion surgery. Eur Spine J 24(11):2555–2559. https://doi.org/10.1007/s00586-015-3888-z
Yan L, Gao R, Liu Y, He B, Lv S, Hao D (2017) The pathogenesis of ossification of the posterior longitudinal ligament. Aging Dis 8 (5):570-582. Doi:10.14336/AD.2017.0201
Nakashima H, Kanemura T, Satake K, Ishikawa Y, Ouchida J, Segi N, Yamaguchi H, Imagama S (2019) Indirect decompression on MRI chronologically progresses after immediate postlateral lumbar interbody fusion: the results from a minimum of 2 years follow-up. Spine (Phila Pa 1976) 44(24):E1411–e1418. https://doi.org/10.1097/brs.0000000000003180
Nemani VM, Aichmair A, Taher F, Lebl DR, Hughes AP, Sama AA, Cammisa FP, Girardi FP (2014) Rate of revision surgery after stand-alone lateral lumbar interbody fusion for lumbar spinal stenosis. Spine (Phila Pa 1976) 39(5):E326–E331. https://doi.org/10.1097/BRS.0000000000000141
Tempel ZJ, McDowell MM, Panczykowski DM, Gandhoke GS, Hamilton DK, Okonkwo DO, Kanter AS (2018) Graft subsidence as a predictor of revision surgery following stand-alone lateral lumbar interbody fusion. J Neurosurg Spine 28(1):50–56. https://doi.org/10.3171/2017.5.SPINE16427
Woods KRM, Billys JB, Hynes RA (2017) Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 17(4):545–553. https://doi.org/10.1016/j.spinee.2016.10.026
Jin CZ, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS (2018) Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res 13:1–10. https://doi.org/10.1186/s13018-018-0740-2
Quillo-Olvera J, Lin GX, Jo HJ, Kim JS (2018) Complications on minimally invasive oblique lumbar interbody fusion at L2-L5 levels: a review of the literature and surgical strategies. Ann Transl Med 6 (6):101. Doi:10.21037/atm.2018.01.22
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J-SK is a consultant for RIWOspine, GmbH, and Elliquence, LLC.
Other authors declare that they have no potential conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This is a retrospective study. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahatthanatrakul, A., Kim, H.S., Lin, GX. et al. Decreasing thickness and remodeling of ligamentum flavum after oblique lumbar interbody fusion. Neuroradiology 62, 971–978 (2020). https://doi.org/10.1007/s00234-020-02414-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02414-y