Abstract
Purpose
To systematically compare the efficacy and safety of sufentanil versus fentanyl for pain relief in labor involving combined spinal-epidural analgesia (CSEA), a systematic review and meta-analysis of randomized controlled trials targeting parturients requesting labor analgesia was conducted.
Methods
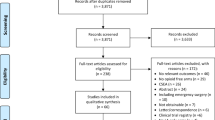
The primary outcome measure was visual analog scale scores assessed at 10, 15, 30, and 60 min after intrathecal injection. Secondary outcomes included duration of spinal analgesia, incidence of side effects in parturients, and neonatal Apgar scores.
Results
Twelve randomized controlled trials, including data from 881 patients fulfilled the inclusion criteria. No clinically meaningful differences in pain reduction after intrathecal injection were found between the two analgesics. Sufentanil extended the duration of spinal analgesia by 25.40 min (95% CI 21.82 to 28.98 min; p < 0.00001) compared with fentanyl. The risk for pruritus, nausea, and vomiting among parturients was 82% for those using sufentanil (relative risk 0.82 [95% CI 0.67–0.99]; p = 0.04) and 48% for those using fentanyl (relative risk 0.48 [95% CI 0.29–0.80]; p = 0.005). Both the synthesis results and sensitivity analysis demonstrated no differences in the risk for respiratory depression between parturients using sufentanil versus fentanyl. The neonates in sufentanil group exhibited higher Apgar scores than the fentanyl group 5 min after delivery (weighted mean difference 0.10 [95% CI 0.05–0.16]; p = 0.0002).
Conclusion
Existing evidence suggests that compared with fentanyl, sufentanil used for analgesia in combined spinal-epidural during labor is more effective in extending the duration of spinal analgesia, and may be safer for the infant. There was overall low clinical and statistical heterogeneity among the included studies. For all outcomes, variations caused by heterogeneity across trials were acceptable. Thus the findings of this meta-analysis may provide additional evidence for future clinical practices of pain relief in labor involving CSEA. Stronger evidence supporting this conclusion will require data from more high-quality and multicenter randomized controlled trials.
Similar content being viewed by others
References
Heesen M, Velde MVD, Klöhr S, Lehberger J, Rossaint R, Straube S (2014) Meta-analysis of the success of block following combined spinal-epidural vs epidural analgesia during labor. Anesthesia 69(1):64–71. https://doi.org/10.1111/anae.12456
Zheng L, Wu LJ (2016) Comparison of adding sufentanil or fentanyl to ropivacaine for combined spinal-epidural analgesia during labor. Anhui Med Pharm J 20(3):576–578. https://doi.org/10.3969/j.issn.1009-6469.2016.03.052
Shafer SL, Varvel JR (1991) Pharmacokinetics, pharmacodynamics, and rational opioid selection. Anesthesiology 74:53–63. https://doi.org/10.1097/00000542-199101000-00010
National Center for Biotechnology Information (2019) PubChem Database. Sufentanil, CID=41693. https://pubchem.ncbi.nlm.nih.gov/compound/41693. Accessed 29 July 2019
Chen P, Chen FC, Guo XX, Zhou BH (2017) Meta analysis of efficacy and safety of Dexmedetomidine combined with Sufentanil for postoperative patient-controlled intravenous analgesia. Chin J Pharmacovigilance 10:626–631. https://doi.org/10.3969/j.issn.1672-8629.2017.10.012
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group (2015) Preferred reporting items for systematic review and Meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1. https://doi.org/10.1186/2046-4053-4-1
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group PRISMA-P Group (2015) Preferred reporting items for systematic review and Meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647. https://doi.org/10.1136/bmj.g7647
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and Meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Nelson KE, Rauch T, Terebuh V, D’Angelo R (2002) A comparison of intrathecal fentanyl and sufentanil for labor analgesia. Anesthesiology 96(5):1070–1073. https://doi.org/10.1097/00000542-200205000-00007
Sheng XF, Yao SL (2016) Consensus of experts on labor analgesia (2016 edition). J Clin Anesth 32:816–818 ISSN: 1004-5805
Qu Y, Liu Z, Liu Y, et al. Consensus of Chinese obstetric anesthesia experts (2017 Edition). Chinese Society of Obstetric Anesthesiology. Chinese Medical Association. http://guide.medlive.cn/guideline/15952
Plante L, Gaiser R (2017) Practice bulletin no.177: obstetric analgesia and anesthesia. Obstet Gynecol 129:e73–e89. https://doi.org/10.1097/AOG.0000000000002018
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions. Version 5.1.0. [updated march 2011]. https://handbook-5-1.cochrane.org/. Accessed 23 July 2019
Zheng JQ, Feng JF, Peng W, Zhao B, Chi T (2009) Clinical observation of sufentanil and fentanyl for combined spinal-epidural labor analgesia. Guangxi Med 31(9):1267–1269. https://doi.org/10.3969/j.issn.0253-4304.2009.09.018
Lu YM, Lin GY, Zhang Y (2009) Effects of sufentanil and ropivacaine on labor analgesia combined with spinal-epidural analgesia. Chin Med 4(9):703–705. https://doi.org/10.3760/cma.j.issn.1673-4777.2009.09.029
Yan XB, Li SQ (2011) Effects of sufentanil to ropivacaine for combined spinal-epidural analgesia during labor. Matern Child Healthc Chin 26(28):4466–4468 ISSN: 1001-4411 (2011)28-4466-03
Li RX, Ke SG, Xu XJ, Zhu TH (2013) Clinical analysis of effect of combined spinal-epidural in labor analgesia. Anhui Med 2(7):949–951. https://doi.org/10.3969/j.issn.1000-0399.2011.07.029
Li CF, Deng JL, Shen LY (2013) Application of adding sufentanil to low concentration ropivacaine for combined spinal-epidural analgesia during labor. Youjiang Med 41(4):599–551. https://doi.org/10.3969/j.issn.1003-1383.2013.04.030
Chen YL, Zeng LR, Guo R (2015) Comparison of the effects of sufentanil and fentanyl on parturients for combined spinal-epidural analgesia during labor. Heilongjiang Med Sci 38(1):32–34. https://doi.org/10.3969/j.issn.1008-0104.2015.01.014
Tang ZJ, Huang N, Shu JJ. (2017) Comparison of the effects of ropivacaine combined with sufentanil or fentanyl under CSEA combined with PCEA for labor analgesia. China practical medicine 12(19):124-6. https://doi.org/10.14163/j.cnki.11-5547/r.2017.19.066
Gaiser RR, Cheek TG, Gutsche BB (1998) Comparison of three different doses of intrathecal fentanyl and sufentanil for labor analgesia. J Clin Anesth 10(6):488–493. https://doi.org/10.1016/S0952-8180(98)00076-2
Cheng CJ, Sia AT, Lim EH, Loke GP, Tan HM (2001) Either sufentanil or fentanyl, in addition to intrathecal bupivacaine, provide satisfactory early labor analgesia. Can J Anesth 48(6):570–574. https://doi.org/10.1007/BF03016834
Farrar JT, Berlin JA, Strom BL (2003) Clinically important changes in acute pain outcome measures: a validation study. J Pain Symptom Manag 25:406–411. https://doi.org/10.1016/S0885-3924(03)00162-3
Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL (2000) Defining the clinically important difference in pain outcome measures. Pain 88:287–294. https://doi.org/10.1016/S0304-3959(00)00339-0
Scholz J, Steinfath M, Schulz M (1996) Clinical pharmacokinetics of Alfentanil, fentanyl and Sufentanil. Clin Pharmacokinet 31(4):275–292. https://doi.org/10.2165/00003088-199631040-00004
Acknowledgements
The authors appreciate the advice provided by Professor Yuguang Huang and his team at Peking Union Medical College Hospital, and funding provided by the Peking Union Medical College Education Fund 2017-2019.
Funding
This study was supported by the Peking Union Medical College Education Fund 2017–2019.
Author information
Authors and Affiliations
Contributions
The study was designed by the team led by SJ and LY. Authors worked in pairs for all reviews and analysis. LS and GS, and HZ and SX independently screened all retrieved trials by reviewing their titles and abstracts. ZM and DY, LS and GS, and HZ and SX independently evaluated the full-text literature for eligibility using the standardized criteria, and extracted relevant data from the full texts using a standardized data collection form, including key information regarding the trials, results of primary and secondary outcome measures, anesthetic dosage and usage, and parturient obstetric characteristics and their baseline comparability. Any disagreement between authors was resolved jointly by SJ, SL and LY. All authors agree with the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 368 kb)
Rights and permissions
About this article
Cite this article
Zhi, M., Diao, Y., Liu, S. et al. Sufentanil versus fentanyl for pain relief in labor involving combined spinal-epidural analgesia: a systematic review and meta-analysis of randomized controlled trials. Eur J Clin Pharmacol 76, 501–506 (2020). https://doi.org/10.1007/s00228-019-02806-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02806-x