Abstract
Objective
The substantial weight loss in Parkinson’s patients may be related to direct influences of levodopa treatment on fat mobilization/oxidation. We assessed systemic and local metabolic responses to levodopa/benserazide in patients with idiopathic Parkinson’s disease.
Methods
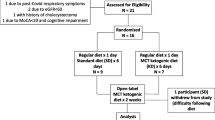
We studied 10 Parkinson’s disease patients and examined adipose tissue and skeletal muscle metabolism directly with microdialysis. We monitored dialysate concentrations of ethanol, glucose, lactate, pyruvate, and glycerol to assess tissue blood flow and metabolism before and after levodopa/benserazide intake. We also conducted in vitro studies on adipocytes from healthy women.
Results
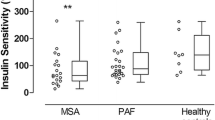
Levodopa/benserazide increased serum levodopa, 3,4-dihydroxyphenylacetic acid (DOPAC), and norepinephrine (P < 0.01). Serum adipose tissue and skeletal muscle glycerol did not change or decreased. Adipose tissue glycerol was inversely correlated with serum levodopa concentrations (P < 0.05). In isolated adipocytes, levodopa attenuated isoproterenol-induced glycerol release (P < 0.05).
Conclusion
Levodopa/benserazide elicits pronounced metabolic changes in both adipose tissue and skeletal muscle with a switch from lipid to carbohydrate metabolism. In adipose tissue, levodopa/benserazide failed to activate lipolysis. Therefore, we suggest that levodopa/benserazide does not induce fat wasting through direct and acute influences on adipose tissue metabolism.






Similar content being viewed by others
References
Markus HS, Tomkins AM, Stern GM (1993) Increased prevalence of undernutrition in Parkinson’s disease and its relationship to clinical disease parameters. J Neural Transm Parkinson’s Dis Dement Sect 5:117–125
Davies KN, King D, Davies H (1994) A study of the nutritional status of elderly patients with Parkinson’s disease. Age Ageing 23:142–145
Bachmann CG, Trenkwalder C (2006) Body weight in patients with Parkinson’s disease. Mov Disord 21:1824–1830
Palhagen S, Lorefalt B, Carlsson M et al (2005) Does L-dopa treatment contribute to reduction in body weight in elderly patients with Parkinson’s disease? Acta Neurol Scand 111:12–20
Toth MJ, Fishman PS, Poehlman ET (1997) Free-living daily energy expenditure in patients with Parkinson’s disease. Neurology 48:88–91
Abbott RA, Cox M, Markus H et al (1992) Diet, body size and micronutrient status in Parkinson’s disease. Eur J Clin Nutr 46:879–884
Lorefalt B, Ganowiak W, Palhagen S et al (2004) Factors of importance for weight loss in elderly patients with Parkinson’s disease. Acta Neurol Scand 110:180–187
Macia F, Perlemoine C, Coman I et al (2004) Parkinson’s disease patients with bilateral subthalamic deep brain stimulation gain weight. Mov Disord 19:206–212
Giroux ML (2007) Parkinson disease: managing a complex, progressive disease at all stages. Cleve Clin J Med 74:313–320
Boyd AE III, Lebovitz HE, Pfeiffer JB (1970) Stimulation of human-growth-hormone secretion by L-dopa. N Engl J Med 283:1425–1429
Sirtori CR, Bolme P, Azarnoff DL (1972) Metabolic responses to acute and chronic L-dopa administration in patients with parkinsonism. N Engl J Med 287:729–733
Deleu D, Sarre S, Ebinger G et al (1993) Simultaneous monitoring of levodopa, dopamine and their metabolites in skeletal muscle and subcutaneous tissue in different pharmacological conditions using microdialysis. J Pharm Biomed Anal 11:577–585
Pizzinat N, Marti L, Remaury A et al (1999) High expression of monoamine oxidases in human white adipose tissue: evidence for their involvement in noradrenaline clearance. Biochem Pharmacol 58:1735–1742
Morin N, Lizcano JM, Fontana E et al (2001) Semicarbazide-sensitive amine oxidase substrates stimulate glucose transport and inhibit lipolysis in human adipocytes. J Pharmacol Exp Ther 297:563–572
Adams F, Boschmann M, Schaller K et al (2006) Tyramine in the assessment of regional adrenergic function. Biochem Pharmacol 72:1724–1729
Bairras C, Ferrand C, Atgie C (2003) Effect of tyramine, a dietary amine, on glycerol and lactate release by isolated adipocytes from old rats. J Physiol Biochem 59:161–167
Boschmann M, Krupp G, Luft FC et al (2002) In vivo response to alpha(1)-adrenoreceptor stimulation in human white adipose tissue. Obes Res 10:555–558
Jordan J, Tank J, Stoffels M et al (2001) Interaction between beta-adrenergic receptor stimulation and nitric oxide release on tissue perfusion and metabolism. J Clin Endocrinol Metab 86:2803–2810
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Hughes AJ, Ben-Shlomo Y, Daniel SE et al (1992) What features improve the accuracy of clinical diagnosis in Parkinson’s disease: a clinicopathologic study. Neurology 42:1142–1146
Arner P, Bolinder J, Eliasson A et al (1988) Microdialysis of adipose tissue and blood for in vivo lipolysis studies. Am J Physiol 255:E737–E742
Janke J, Engeli S, Gorzelniak K et al (2002) Mature adipocytes inhibit in vitro differentiation of human preadipocytes via angiotensin type 1 receptors. Diabetes 51:1699–1707
Han SK, Mytilineou C, Cohen G (1996) L-DOPA up-regulates glutathione and protects mesencephalic cultures against oxidative stress. J Neurochem 66:501–510
Fellander G, Linde B, Bolinder J (1996) Evaluation of the microdialysis ethanol technique for monitoring of subcutaneous adipose tissue blood flow in humans. Int J Obes Relat Metab Disord 20:220–226
Stallknecht B, Lorentsen J, Enevoldsen LH et al (2001) Role of the sympathoadrenergic system in adipose tissue metabolism during exercise in humans. J Physiol 536:283–294
Kurpad A, Khan K, Calder AG et al (1994) Effect of noradrenaline on glycerol turnover and lipolysis in the whole body and subcutaneous adipose tissue in humans in vivo. Clin Sci 86:177–184
Smith JL, Ju JS, Saha BM et al (2004) Levodopa with carbidopa diminishes glycogen concentration, glycogen synthase activity, and insulin-stimulated glucose transport in rat skeletal muscle. J Appl Physiol 97:2339–2346
Smith JL, Patil PB, Minteer SD et al (2005) Possibility of autocrine beta-adrenergic signaling in C2C12 myotubes. Exp Biol Med 230:845–852
Rose S, Jenner P, Marsden CD (1988) The effect of carbidopa on plasma and muscle levels of L-dopa, dopamine, and their metabolites following L-dopa administration to rats. Mov Disord 3:117–125
Coppack SW, Persson M, Judd RL et al (1999) Glycerol and nonesterified fatty acid metabolism in human muscle and adipose tissue in vivo. Am J Physiol 276:E233–E240
Duncan RE, Ahmadian M, Jaworski K et al (2007) Regulation of lipolysis in adipocytes. Annu Rev Nutr 27:79–101
Mauras N, Haymond MW (2005) Are the metabolic effects of GH and IGF-I separable? Growth Horm IGF Res 15:19–27
Hellström L, Wahrenberg H, Reynisdottir S et al (1997) Catecholamine-induced adipocyte lipolysis in human hyperthyroidism. J Clin Endocrinol Metab 82:159–166
Dizdar N, Kullman A, Norlander B et al (1999) Human pharmacokinetics of L-3,4-dihydroxyphenylalanine studied with microdialysis. Clin Chem 45:1813–1820
Visentin V, Prevot D, Marti L et al (2003) Inhibition of rat fat cell lipolysis by monoamine oxidase and semicarbazide-sensitive amine oxidase substrates. Eur J Pharmacol 466:235–243
Lyytinen J, Kaakkola S, Ahtila S et al (1997) Simultaneous MAO-B and COMT inhibition in L-dopa-treated patients with Parkinson’s disease. Mov Disord 12:497–505
Flechtner-Mors M, Jenkinson CP, Alt A et al (2005) Studies of phosphodiesterase effects on adipose tissue metabolism in obese subjects by the microdialysis technique. J Physiol Pharmacol 56:355–368
Goossens GH, Blaak EE, Saris WH et al (2004) Angiotensin II-induced effects on adipose and skeletal muscle tissue blood flow and lipolysis in normal-weight and obese subjects. J Clin Endocrinol Metab 89:2690–2696
Sandyk R (1993) The relationship between diabetes mellitus and Parkinson’s disease. Int J Neurosci 69:125–130
Acknowledgements
The authors thank Henning Damm, Katrin Sprengel, and Janin Andres for expert technical assistance and the Department of Surgery at the Vivantes Klinikum Prenzlauer Berg in Berlin for providing us with adipose tissue samples.
Conflict of Interest
The authors declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adams, F., Boschmann, M., Lobsien, E. et al. Influences of levodopa on adipose tissue and skeletal muscle metabolism in patients with idiopathic Parkinson’s disease. Eur J Clin Pharmacol 64, 863–870 (2008). https://doi.org/10.1007/s00228-008-0532-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-008-0532-4