Abstract
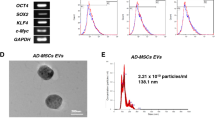
Muscle/bone interaction has been recently noted. Extracellular vesicles (EVs) play a vital role in physiological and pathophysiological processes by transferring microRNA (miRNA) to distant tissues. We previously reported that EVs secreted from C2C12 myoblasts (Myo-EVs) suppress osteoclast differentiation. In the present study, we identified 4 miRNAs in Myo-EVs that suppressed osteoclast-like cell formation in Raw264.7 cells using small RNA sequencing analysis. Among them, miR-196a-5p expression was higher in C2C12 cells compared to mouse osteoblasts and bone marrow cells. Transfection of miR-196a-5p mimic suppressed the mRNA levels of osteoclast-related genes and mitochondrial energy metabolism induced by receptor activator of nuclear factor-κB ligand in Raw264.7 cells. In contrast, miR-196a-5p mimic enhanced osteoblastic differentiation in ST-2 cells and MC3T3-E1 cells. In conclusion, we demonstrated that miR-196-5p suppresses osteoclast-like cell formation and mitochondrial energy metabolism in mouse cells, suggesting that it might be a crucial factor for muscle/bone interaction via EVs.





Similar content being viewed by others
Data Availability
The datasets generated and analysed during the present study are not publicly available but are available from the corresponding author upon reasonable request.
References
Kawao N, Kaji H (2015) Interactions between muscle tissues and bone metabolism. J Cell Biochem 116(5):687–695. https://doi.org/10.1002/jcb.25040
Kaji H (2016) Effects of myokines on bone. Bonekey Rep 5:826. https://doi.org/10.1038/bonekey.2016.48
Ikebuchi Y, Aoki S, Honma M, Hayashi M, Sugamori Y, Khan M, Kariya Y, Kato G, Tabata Y, Penninger JM, Udagawa N, Aoki K, Suzuki H (2018) Coupling of bone resorption and formation by RANKL reverse signalling. Nature 561(7722):195–200. https://doi.org/10.1038/s41586-018-0482-7
Cui YZ, Luan J, Li HY, Zhou XY, Han JX (2016) Exosomes derived from mineralizing osteoblasts promote ST2 cell osteogenic differentiation by alteration of microRNA expression. Febs Lett 590(1):185–192. https://doi.org/10.1002/1873-3468.12024
Li Q, Huang QP, Wang YL, Huang QS (2018) Extracellular vesicle-mediated bone metabolism in the bone microenvironment. J Bone Miner Metab 36(1):1–11. https://doi.org/10.1007/s00774-017-0860-5
Sun WJ, Zhao CY, Li YH, Wang L, Nie GJ, Peng J, Wang AY, Zhang PF, Tian WM, Li Q, Song JP, Wang C, Xu XL, Tian YH, Zhao DS, Xu Z, Zhong GH, Han BX, Ling SK, Chang YZ, Li YX (2016) Osteoclast-derived microRNA-containing exosomes selectively inhibit osteoblast activity. Cell Discov. https://doi.org/10.1038/celldisc.2016.15
Takafuji Y, Tatsumi K, Ishida M, Kawao N, Okada K, Kaji H (2020) Extracellular vesicles secreted from mouse muscle cells suppress osteoclast formation: roles of mitochondrial energy metabolism. Bone. https://doi.org/10.1016/j.bone.2020.115298
Cheng M, Yang JJ, Zhao XQ, Zhang E, Zeng QT, Yu Y, Yang L, Wu BW, Yi GW, Mao XB, Huang K, Dong NG, Xie M, Limdi NA, Prabhu SD, Zhang JY, Qin GJ (2019) Circulating myocardial microRNAs from infarcted hearts are carried in exosomes and mobilise bone marrow progenitor cells. Nat Commun 10:959. https://doi.org/10.1038/s41467-019-08895-7
Huan J, Hornick NI, Shurtleff MJ, Skinner AM, Goloviznina NA, Roberts CT Jr, Kurre P (2013) RNA trafficking by acute myelogenous leukemia exosomes. Cancer Res 73(2):918–929. https://doi.org/10.1158/0008-5472.CAN-12-2184
Fang SJ, Deng Y, Gu P, Fan XQ (2015) MicroRNAs regulate bone development and regeneration. Int J Mol Sci 16(4):8227–8253. https://doi.org/10.3390/ijms16048227
Zhao X, Xu D, Li Y, Zhang J, Liu T, Ji Y, Wang J, Zhou G, Xie X (2014) MicroRNAs regulate bone metabolism. J Bone Miner Metab 32(3):221–231. https://doi.org/10.1007/s00774-013-0537-7
Zhang Y, Xie RL, Gordon J, LeBlanc K, Stein JL, Lian JB, van Wijnen AJ, Stein GS (2012) Control of mesenchymal lineage progression by MicroRNAs targeting skeletal gene regulators Trps1 and Runx2. J Biol Chem 287(26):21926–21935. https://doi.org/10.1074/jbc.M112.340398
Lozano C, Duroux-Richard I, Firat H, Schordan E, Apparailly F (2019) MicroRNAs : key regulators to understand osteoclast differentiation? Front Immunol 10:375. https://doi.org/10.3389/fimmu.2019.00375
Hosseinahli N, Aghapour M, Duijf PHG, Baradaran B (2018) Treating cancer with microRNA replacement therapy: a literature review. J Cell Physiol 233(8):5574–5588. https://doi.org/10.1002/jcp.26514
Ai GH, Meng M, Wang L, Shao XW, Li Y, Cheng JJ, Tong XW, Cheng ZP (2019) MicroRNA-196a promotes osteogenic differentiation and inhibit adipogenic differentiation of adipose stem cells via regulating beta-catenin pathway. Am J Transl Res 11(5):3081–3091
Hou T, Ou J, Zhao X, Huang X, Huang Y, Zhang Y (2014) MicroRNA-196a promotes cervical cancer proliferation through the regulation of FOXO1 and p27(Kip1). Brit J Cancer 110(5):1260–1268. https://doi.org/10.1038/bjc.2013.829
Takafuji Y, Hori M, Mizuno T, Harada-Shiba M (2019) Humoral factors secreted from adipose tissue-derived mesenchymal stem cells ameliorate atherosclerosis in Ldlr(-/-) mice. Cardiovasc Res 115(6):1041–1051. https://doi.org/10.1093/cvr/cvy271
Takafuji Y, Tatsumi K, Ishida M, Kawao N, Okada K, Matsuo O, Kaji H (2019) Plasminogen activator inhibitor-1 deficiency suppresses osteoblastic differentiation of mesenchymal stem cells in mice. J Cell Physiol 234(6):9687–9697. https://doi.org/10.1002/jcp.27655
Kawao N, Tamura Y, Okumoto K, Yano M, Okada K, Matsuo O, Kaji H (2013) Plasminogen plays a crucial role in bone repair. J Bone Miner Res 28(7):1561–1574. https://doi.org/10.1002/jbmr.1921
Kim K, Kim JH, Kim I, Lee J, Seong S, Park YW, Kim N (2015) MicroRNA-26a regulates RANKL-induced osteoclast formation. Mol Cells 38(1):75–80. https://doi.org/10.14348/molcells.2015.2241
Ishii K, Fumoto T, Iwai K, Takeshita S, Ito M, Shimohata N, Aburatani H, Taketani S, Lelliott CJ, Vidal-Puig A, Ikeda K (2009) Coordination of PGC-1 beta and iron uptake in mitochondrial biogenesis and osteoclast activation. Nat Med 15(3):259–266. https://doi.org/10.1038/nm.1910
Yu FY, Xie CQ, Sun JT, Peng W, Huang XW (2018) Overexpressed miR-145 inhibits osteoclastogenesis in RANKL-induced bone marrow-derived macrophages and ovariectomized mice by regulation of Smad3. Life Sci 202:11–20. https://doi.org/10.1016/j.lfs.2018.03.042
Li GW, Bu JY, Zhu YX, Xiao XY, Liang ZB, Zhang RK (2015) Curcumin improves bone microarchitecture in glucocorticoid-induced secondary osteoporosis mice through the activation of microRNA-365 via regulating MMP-9. Int J Clin Exp Patho 8(12):15684–15695
Yin YR, Tang L, Chen JY, Lu XB (2017) MiR-30a attenuates osteoclastogenesis via targeting DC-STAMP-c-Fos-NFATc1 signaling. Am J Transl Res 9(12):5743–5753
Zhang J, Zhao HY, Chen JP, Xia B, Jin YM, Wei W, Shen JJ, Huang YZ (2012) Interferon-beta-induced miR-155 inhibits osteoclast differentiation by targeting SOCS1 and MITF. Febs Lett 586(19):3255–3262. https://doi.org/10.1016/j.febslet.2012.06.047
Kim YJ, Bae SW, Yu SS, Bae YC, Jung JS (2009) miR-196a regulates proliferation and osteogenic differentiation in mesenchymal stem cells derived from human adipose tissue. J Bone Miner Res 24(5):816–825. https://doi.org/10.1359/jbmr.081230
Takayanagi H, Kim S, Koga T, Nishina H, Isshiki M, Yoshida H, Saiura A, Isobe M, Yokochi T, Inoue J, Wagner EF, Mak TW, Kodama T, Taniguchi T (2002) Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev Cell 3(6):889–901. https://doi.org/10.1016/S1534-5807(02)00369-6
Zhao BH, Takami M, Yamada A, Wang XG, Koga T, Hu XY, Tamura T, Ozato K, Choi YW, Ivashkiv LB, Takayanagi H, Kamijo R (2009) Interferon regulatory factor-8 regulates bone metabolism by suppressing osteoclastogenesis. Nat Med 15(9):1066–1071. https://doi.org/10.1038/nm.2007
Franceschetti T, Kessler CB, Lee SK, Delany AM (2013) miR-29 promotes murine osteoclastogenesis by regulating osteoclast commitment and migration. J Biol Chem 288(46):33347–33360. https://doi.org/10.1074/jbc.M113.484568
Krzeszinski JY, Wei W, Huynh H, Jin ZX, Wang XD, Chang TC, Xie XJ, He L, Mangala LS, Lopez-Berestein G, Sood AK, Mendell JT, Wan YH (2014) miR-34a blocks osteoporosis and bone metastasis by inhibiting osteoclastogenesis and Tgif2. Nature 512(7515):431–435. https://doi.org/10.1038/nature13375
Zhou L, Song HY, Gao LL, Yang LY, Mu S, Fu Q (2019) MicroRNA-100-5p inhibits osteoclastogenesis and bone resorption by regulating fibroblast growth factor 21. Int J Mol Med 43(2):727–738. https://doi.org/10.3892/ijmm.2018.4017
Li Y, Zhang MX, Chen HJ, Dong Z, Ganapathy V, Thangaraju M, Huang SA (2010) Ratio of miR-196s to HOXC8 messenger RNA correlates with breast cancer cell migration and metastasis. Cancer Res 70(20):7894–7904. https://doi.org/10.1158/0008-5472
Tsai MM, Wang CS, Tsai CY, Huang CG, Lee KF, Huang HW, Lin YH, Chi HC, Kuo LM, Lu PH, Lin KH (2016) Circulating microRNA-196a/b are novel biomarkers associated with metastatic gastric cancer. Eur J Cancer 64:137–148. https://doi.org/10.1016/j.ejca.2016.05.007
Ge J, Chen ZH, Li RX, Lu TL, Xiao GF (2014) Upregulation of microRNA-196a and microRNA-196b cooperatively correlate with aggressive progression and unfavorable prognosis in patients with colorectal cancer. Cancer Cell Int 14:128. https://doi.org/10.1186/s12935-014-0128-2
Suh YE, Raulf N, Gaken J, Lawler K, Urbano TG, Bullenkamp J, Gobeil S, Huot J, Odell E, Tavassoli M (2015) MicroRNA-196a promotes an oncogenic effect in head and neck cancer cells by suppressing annexin A1 and enhancing radioresistance. Int J Cancer 137(5):1021–1034. https://doi.org/10.1002/ijc.29397
Liu XH, Lu KH, Wang KM, Sun M, Zhang EB, Yang JS, Yin DD, Liu ZL, Zhou J, Liu ZJ, De W, Wang ZX (2012) MicroRNA-196a promotes non-small cell lung cancer cell proliferation and invasion through targeting HOXA5. Bmc Cancer 12:348. https://doi.org/10.1186/1471-2407-12-348
Brest P, Lapaquette P, Souidi M, Lebrigand K, Cesaro A, Vouret-Craviari V, Mari B, Barbry P, Mosnier JF, Hebuterne X, Harel-Bellan A, Mograbi B, Darfeuille-Michaud A, Hofman P (2011) A synonymous variant in IRGM alters a binding site for miR-196 and causes deregulation of IRGM-dependent xenophagy in Crohn’s disease. Nat Genet 43(3):242–245. https://doi.org/10.1038/ng.762
Cheng PH, Li CL, Chang YF, Tsai SJ, Lai YY, Chan AWS, Chen CM, Yang SH (2013) miR-196a ameliorates phenotypes of huntington disease in cell, transgenic mouse, and induced pluripotent stem cell models. Am J Hum Genet 93(2):306–312. https://doi.org/10.1016/j.ajhg.2013.05.025
Her LS, Mao SH, Chang CY, Cheng PH, Chang YF, Yang HI, Chen CM, Yang SH (2017) miR-196a enhances neuronal morphology through suppressing RANBP10 to provide neuroprotection in huntington’s disease. Theranostics 7(9):2452–2462. https://doi.org/10.7150/thno.18813
Candini O, Spano C, Murgia A, Grisendi G, Veronesi E, Piccinno MS, Ferracin M, Negrini M, Giacobbi F, Bambi F, Horwitz EM, Conte P, Paolucci P, Dominici M (2015) Mesenchymal progenitors aging highlights a miR-196 switch targeting HOXB7 as master regulator of proliferation and osteogenesis. Stem Cells 33(3):939–950. https://doi.org/10.1002/stem.1897
Xu Q, Cui YZ, Luan J, Zhou XY, Li HY, Han JX (2018) Exosomes from C2C12 myoblasts enhance osteogenic differentiation of MC3T3-E1 pre-osteoblasts by delivering miR-27a-3p. Biochem Bioph Res Co 498(1):32–37. https://doi.org/10.1016/j.bbrc.2018.02.144
Esen E, Lee SY, Wice BM, Long FX (2015) PTH promotes bone anabolism by stimulating aerobic glycolysis via IGF signaling. J Bone Miner Res 30(11):2137–2137. https://doi.org/10.1002/jbmr.2714
Liu ZB, Solesio ME, Schaffler MB, Frikha-Benayed D, Rosen CJ, Werner H, Kopchick JJ, Pavlov EV, Abramov AY, Yakar S (2019) Mitochondrial function is compromised in cortical bone osteocytes of long-lived growth hormone receptor null mice. J Bone Miner Res 34(1):106–122. https://doi.org/10.1002/jbmr.3573
Acknowledgements
The study was supported by the following grants: Japan Osteoporosis Foundation to K.T. and Y. T.; The Osaka Medical Research Foundation for Intractable Diseases to Y. T.; the Cooperative Research Program (Joint usage/Research Center program) of Institute for Frontier Life and Medical Sciences, Kyoto University to Y. T.; the 2019 Kindai University Research Enchancement Grant No. (SR03) to Y. T.; a JSPS KAKENHI Grant-in-Aid for Early Career Scientists (Grant No. 19K18480) to Y. T. and a Grant-in-Aid for Scientific Research on Innovative Areas (Grant No. 15H05935, “Living in Space”)/Grants-in-Aid for Scientific Research (Grant No. C:20K09514) to H.K. from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Contributions
YT, KT, NK and HK contributed to the conception and design of the research. YT, MM and KO performed the experiments. YT and HK interpreted the results of the experiments. YT analysed data, prepared the figures and drafted the manuscript. HK edited and revised the manuscript. All authors approved the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Yoshimasa Takafuji, Kohei Tatsumi, Naoyuki Kawao, Kiyotaka Okada, Masafumi Muratani and Hiroshi Kaji declare that there is no conflict of interest.
Human and Animal Rights and Informed Consent
All applicable international, national and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted. This study does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takafuji, Y., Tatsumi, K., Kawao, N. et al. MicroRNA-196a-5p in Extracellular Vesicles Secreted from Myoblasts Suppresses Osteoclast-like Cell Formation in Mouse Cells. Calcif Tissue Int 108, 364–376 (2021). https://doi.org/10.1007/s00223-020-00772-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-020-00772-6