Abstract
Rationale
In a subgroup of patients with obsessive–compulsive disorder (OCD), motor soft signs, tics and other movement disorders can be observed, indicating a special pathogenetic involvement of basal ganglia.
Objectives
The main objective of this study was to verify the hypothesis that such motor dysfunction characterises a subgroup of OCD patients with poor treatment response. For assessing even subtle motor dysfunction, a new method for kinematical analysis of hand movements has been applied.
Methods
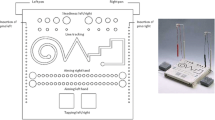
We examined the performance of 45 in-patients who met the DSM-IV criteria for OCD before and under therapy (sertraline and behaviour therapy) using a digitising tablet and kinematical analysis of simple handwriting and drawing movements. All subjects wrote a sentence, their signature and letter sequences. Moreover, they drew circles under different conditions. Three kinematical parameters (stroke duration, variation coefficient of peak velocity, stroke length) were calculated to quantify hand-motor performance.
Results
Prior to therapy, non-responders wrote with significantly smaller amplitudes than responders. Additionally, non-responders drew significantly larger circles with the non-dominant hand at baseline, as compared to responders. Disturbances of handwriting were more frequent in non-responders than in responders.
Conclusions
Kinematical analysis of handwriting movements seems to be interesting for the prediction of poor response to treatments in OCD patients.


Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders (DSM-IV), 4th edn. American Psychiatric Association, Washington, DC
Aylward EH, Harris GJ, Hoehn-Saric R, Barta PE, Machlin SR, Pearlson GD (1996) Normal caudate nucleus in obsessive–compulsive disorder assessed by quantitative neuroimaging. Arch Gen Psychiatry 53:577–584
Bihari K, Pato MT, Hill JL, Murphy DL (1991) Neurologic soft signs in obsessive–compulsive disorder [letter]. Arch Gen Psychiatry 48:278
Bolton D, Gibb W, Lees A, Raven P, Gray JA, Chen E, Shafran R (1998) Neurological soft signs in obsessive–compulsive disorder: standardised assessment and comparison with schizophrenia. Behav Neurol 11:197–204
Bolton D, Raven P, Madronal-Luque R, Marks IM (2000) Neurological and neuropsychological signs in obsessive–compulsive disorder: interaction with behavioural treatment. Behav Res Ther 38:695–708
Buchanan AW, Ko SM, Marks IM (1996) What predicts improvement and compliance during the behavioral treatment of obsessive–compulsive disorder? Anxiety 2:22–27
Castle DJ, Deale A, Marks IM, Cutts F, Chadhoury Y, Stewart A (1994) Obsessive–compulsive disorder: prediction of outcome from behavioural psychotherapy. Acta Psychiatr Scand 89:393–398
Chen EYH, Shapleske J, Luque R, McKenna PJ, Hodges JR, Calloway SP, Hymas NFS, Dening TR, Berrios GE (1995) The Cambridge Neurological Inventory: a clinical instrument for assessment of soft neurological signs in psychiatric patients. Psychiatry Res 56:183–204
Conde Lopez V, de la Gandara Martin JJ, Blanco Lozano ML, Cerezo Rodriguez P, Martinez Roig M, de Dios Francos A (1990) Minor neurological signs in obsessive–compulsive disorders. Actas Luso-Esp Neurol Psiquiatr Cienc Afines 18:143–164
Denckla MB (1989) Neurological examination. In: Rapoport JL (ed) Obsessive compulsive disorders in children and adolescents. American Psychiatric Press, Washington, DC, pp 107–118
Eichhorn T, Gasser T, Mai N, Marquardt C, Arnold G, Schwarz J, Oertel WH (1996) Computational analysis of open loop handwriting movements in Parkinson’s disease: a rapid method to detect dopamimetic effects. Mov Disord 11:289–297
Gallucci RM, Phillips JG, Bradshaw JL, Vaddadi KS, Pantelis C (1997) Kinematic analysis of handwriting movements in schizophrenic patients. Biol Psychiatry 41:830–833
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS (1989a) The Yale–Brown Obsessive–Compulsive-Scale. I. Development, use and reliability. Arch Gen Psychiatry 46:1006–1011
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS (1989b) The Yale–Brown Obsessive–Compulsive Scale. II. Validity. Arch Gen Psychiatry 46:1012–1016
Guy W (1976) ECDEU assessment manual for psychopharmacology. Department of Health, Education and Welfare, Washington, DC
Guz H, Aygun D (2004) Neurological soft signs in obsessive–compulsive disorder. Neurol India 52:72–75
Hamilton M, Guy W (1976) Hamilton depression scale. Beltz, Berlin
Hand I (1994) Expositions-Reaktions-Management. Prax Klin Verhalt Med Rehabil 26:64–68
Hauke W (1998) Praxis des Reizkonfrontationstrainings bei Zwangsstörungen. In: Zaudig M, Hauke W, Hegerl U (eds) Die Zwangsstörung—Diagnostik und Therapie. Schattauer, Stuttgart, pp 87–100
Hauke W, Niedermeier N (1998) Verhaltensanalyse und funktionales Bedingungsmodell bei Zwangsstörungen. In: Zaudig M, Hauke W, Hegerl U (eds) Die Zwangsstörung—Diagnostik und Therapie. Schattauer, Stuttgart, pp 51–55
Hauke W, Ruppert S, Unger H, Manzinger H, Schlehlein B, Zaudig M (1998) Multimodale stationäre Verhaltenstherapie bei Zwangsstörungen-Teil 2: Die therapeutische Praxis. Psychother Psychiatr Psychother Med Klin Psychol 3:224–233
Hikosaka O (1991) Basal ganglia—possible role in motor coordination and learning. Curr Opin Neurobiol 1:638–643
Hohagen F, Winkelmann G, Rasche-Ruchle H, Hand I, König A, Munchau N, Hiss H, Geiger-Kabisch C, Kappler C, Schramm P, Rey E, Aldenhoff J, Berger M (1998) Combination of behaviour therapy with fluvoxamine in comparison with behaviour therapy and placebo. Results of a multicentre study. Br J Psychiatry (Suppl.) 35:71–78
Hollander E, Schiffman E, Cohen B, Rivera-Stein MA, Rosen W, Gorman JM, Fyer AJ, Papp L, Liebowitz MR (1990) Signs of central nervous system dysfunction in obsessive–compulsive disorder. Arch Gen Psychiatry 47:27–32
Hollander E, DeCaria CM, Aronowitz B, Klein DF, Liebowitz MR, Shaffer D (1991a) A pilot follow-up study of childhood soft signs and the development of adult psychopathology. J Neuropsychiatry Clin Neurosci 3:186–189
Hollander E, DeCaria C, Saoud J, Klein DF, Liebowitz MR (1991b) Neurologic soft signs in obsessive–compulsive disorder [letter]. Arch Gen Psychiatry 48:278–279
Hollerbach JM (1981) An oscillation theory of handwriting. Biol Cybern 39:139–156
Hymas NFS, Lees A, Bolton D, Epps K, Head D (1991) The neurology of obsessional slowness. Brain 114:2203–2233
Insel TR (1992) Toward a neuroanatomy of obsessive–compulsive disorder. Arch Gen Psychiatry 49:739–744
Kanfer FH, Reinecker H, Schmelzer D (1996) Selbstmanagement-therapie. Springer, Berlin Heidelberg New York
Kejsers G, Hoogduin C, Schaap C (1994) Predictors of treatment outcome in the behavioral treatment of obsessive–compulsive disorder. Br J Psychiatry 165:781–786
Khanna S (1991) Soft neurological signs in obsessive compulsive disorder. Biol Psychiatry 29:442S
Lazarus A (1978) Multimodale Verhaltenstherapie. Fachbuchhandlung für Psychologie, Frankfurt am Main
Luxenberg JS, Swedo SE, Flament MF, Friedland RP, Rapoport JL, Rapoport SI (1988) Neuroanatomical abnormalities in obsessive–compulsive disorder detected with quantitative X-ray computed tomography. Am J Psychiatry 145:1089–1093
Mai N, Marquardt C (1992) CS—Computerunterstützte Analyse der Bewegungsabläufe beim Schreiben. Bedienungshandbuch (Version 4.3). MedCom, München
Marquardt C, Mai N (1994) A computational procedure for movement analysis in handwriting. J Neurosci Methods 52:39–45
Mataix-Cols D, Alonso P, Hernandez R, Deckersbach T, Savage CR, Manuel Menchon J, Vallejo J (2003) Relation of neurological soft signs to nonverbal memory performance in obsessive–compulsive disorder. J Clin Exp Neuropsychol 25:842–851
Mavrogiorgou P, Hegerl U (1998) Psychopharmakotherapie der Zwangsstörung. In: Zaudig M, Hauke W, Hegerl U (eds) Die Zwangsstörung—Diagnostik und Therapie. Schattauer, Stuttgart, pp 67–78
Mavrogiorgou P, Mergl R, Tigges P, El Husseini J, Schröter A, Juckel G, Zaudig M, Hegerl U (2001) Kinematic analysis of handwriting movements in patients with obsessive–compulsive disorder. JNNP 70:605–612
Mergl R, Tigges P, Schröter A, Möller H-J, Hegerl U (1999) Digitized analysis of handwriting and drawing movements in healthy subjects. Methods, results and perspectives. J Neurosci Methods 90:157–169
Mergl R, Juckel G, Rihl J, Henkel V, Karner M, Tigges P, Schröter A, Hegerl U (2004a) Kinematical analysis of handwriting movements in depressed patients. Acta Psychiatr Scand 109:383–391
Mergl R, Mavrogiorgou P, Juckel G, Zaudig M, Hegerl U (2004b) Effects of sertraline on kinematical aspects of hand movements in patients with obsessive–compulsive disorder. Psychopharmacology 171:179–185
Morasso P, Mussa Ivaldi FA (1982) Trajectory formation and handwriting. A computational model. Biol Cybern 45:131–142
Nickoloff SE, Radant AD, Reichler R, Hommer DW (1991) Smooth pursuit and saccadic eye movements and neurological soft signs in obsessive–compulsive disorder. Psychiatry Res 38:173–185
O’Sullivan G, Marks IM (1991) Follow-up studies of behavioural treatment of phobic and obsessive compulsive neuroses. Psychiatr Ann 21:368–373
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9:97–113
Phillips JG, Bradshaw JL, Chiu E, Bradshaw JA (1994) Characteristics of handwriting of patients with Huntington’s disease. Mov Disord 9:521–530
Pigott TA, L’Heureux F, Dubbert B, Bernstein S, Murphy DL (1994) Obsessive compulsive disorder: comorbid conditions. J Clin Psychiatry 55(Suppl.):15–32
Pine D, Shaffer D, Schonfeld IS (1993) Persistent emotional disorder in children with neurological soft signs. J Am Acad Child Adolesc Psych 32:1229–1236
Rasmussen SA, Eisen JL (1990). Epidemiology of obsessive–compulsive disorder. J Clin Psychiatry 51:10–13
Robinson D, Wu H, Munne RA, Ashtari M, Alvir JM, Lerner G, Koreen A, Cole K, Bogerts B (1995) Reduced caudate nucleus volume in obsessive–compulsive disorder. Arch Gen Psychiatry 52:393–398
Ruppert S, Zaudig M, Hauke W, Unger H, Manzinger H, Schlehlein B (1998) Multimodale stationäre Verhaltenstherapie bei Zwangsstörungen-Teil 1: Grundlagen und Methoden. Psychother Psychiatr Psychother Med Klin Psychol 3:215–223
Sabbe B, Hulstijn W, van Hoof JJM, Zitman F (1996) Fine motor retardation and depression. J Psychiatr Res 30:295–306
Schenk T, Walther EU, Mai N (2000) Closed- and open-loop handwriting performance in patients with multiple sclerosis. Eur J Neurol 7:269–279
Shaffer D, Schonfeld IS, O’Connor PA, Stokman C, Trautman P, Shafer S, Ng SC (1985) Neurological soft signs and their relationship to psychiatric disorder and intelligence in childhood and adolescence. Arch Gen Psychiatry 42:342–351
Slavin MJ, Phillips JG, Bradshaw JL, Hall KA, Presnell I (1999) Consistency of handwriting movements in dementia of the Alzheimer’s type: A comparison with Huntington’s and Parkinson’s diseases. J Int Neuropsychol Soc 5:20–25
Stein DJ (2001) Handwriting and obsessive–compulsive disorder [letter]. Lancet 358:524–525
Thienemann M, Koran LM (1995) Do soft signs predict treatment outcome in obsessive–compulsive disorder? J Neuropsychiatry Clin Neurosci 7:218–222
Tigges P, Mergl R, Frodl T, Meisenzahl EM, Gallinat J, Schröter A, Riedel M, Müller N, Möller H-J, Hegerl U (2000) Digitized analysis of abnormal hand motor performance in schizophrenic patients. Schizophr Res 45:133–143
Viviani P, Terzuolo CA (1980) Space–time invariance in learned motor skills. In: Stelmach GE, Requin CJ (eds) Tutorials in motor behaviour. North-Holland, Amsterdam, pp 525–533
World Medical Association (1997) World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA 277:925–926
Acknowledgements
This study was kindly supported by Pfizer, Germany. The evaluation of the present data was performed by Roland Mergl as part of his thesis for the acquisition of the Ph.D. degree.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mergl, R., Mavrogiorgou, P., Juckel, G. et al. Can a subgroup of OCD patients with motor abnormalities and poor therapeutic response be identified?. Psychopharmacology 179, 826–837 (2005). https://doi.org/10.1007/s00213-004-2115-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-004-2115-0