Abstract
Summary
Fractures often cause irreversible harm in Duchenne muscular dystrophy (DMD). This study investigated the trajectory of bone mineral density (BMD) using group-based trajectory modeling and identified that BMD acts as an early-stage indicator of clinically significant bone fragility. The greater the early-stage BMD, the better the 4-year bone health outcome.
Purpose
Most Duchenne muscular dystrophy (DMD) children suffer bone loss after long-term glucocorticoid (GC) exposure, which induces scoliosis and fragility fractures. To assess the BMD progression pattern and individual medical risk markers for these phenotypes in young ambulatory boys with DMD, and provide evidence-based suggestions for clinical management of bone health.
Methods
A retrospective longitudinal cohort study of 153 boys with DMD in West China Second University Hospital (2016–2023) was performed. Group-based trajectory modeling was used to study the BMD progression pattern, and potential predictors were further analyzed by logistic regression and survival analysis.
Results
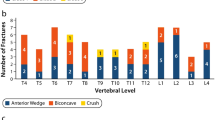
One hundred and fifty-three participants were included, 71 of which had more than 3 BMD records. Three BMD trajectories were identified. Baseline BMD and age-started GC and were independent predictors of trajectory attribution. The median survival time of the first observation of low BMD in GC-treated DMD boys was 5.32 (95% CI 4.05–6.59) years, and a significant difference was tested (P < 0.001) among the three trajectory groups.
Conclusion
BMD may serve as a novel early indicating marker for monitoring bone fragility for DMD. We proposed a bone health risk stratification through BMD progression trajectory that allows us to adapt the osteoporosis warning sign in DMD from a fixed threshold approach to a more individualized strategy, where baseline BMD and age of glucocorticoid initiation can provide an earlier prediction of bone loss. Better management of primary BMD may be able to delay or avoid the onset of adverse bone health outcomes in the fifth year in children with DMD.


Similar content being viewed by others
Data availability
All datasets generated and analyzed during the current study are not publicly available but are available from the corresponding author on a reasonable request.
Change history
06 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00198-024-07034-3
Abbreviations
- DMD:
-
Duchenne muscular dystrophy
- GC:
-
Glucocorticoid
- BMD:
-
Bone mineral density
- GBTM:
-
Group-based trajectory modeling
- QCT:
-
Quantitative computed tomography
- OR:
-
Odd ratio
- IQR:
-
Interquartile range
References
Patterson G, Conner H, Groneman M et al (2023) Duchenne muscular dystrophy: current treatment and emerging exon skipping and gene therapy approach. Eur J Pharmacol 947:175675. https://doi.org/10.1016/j.ejphar.2023.175675
Crisafulli S, Sultana J, Fontana A et al (2020) Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis. Orphanet J Rare Dis 15:141. https://doi.org/10.1186/s13023-020-01430-8
Wood CL, Straub V (2018) Bones and muscular dystrophies: what do we know? Curr Opin Neurol 31:583–591. https://doi.org/10.1097/WCO.0000000000000603
Larson CM, Henderson RC (2000) Bone mineral density and fractures in boys with Duchenne muscular dystrophy. J Pediatr Orthop 20:71–74
Birnkrant DJ, Bushby K, Bann CM et al (2018) Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol 17:347–361. https://doi.org/10.1016/S1474-4422(18)30025-5
Bushby K, Finkel R, Birnkrant DJ et al (2010) Diagnosis and management of Duchenne muscular dystrophy, part 2: implementation of multidisciplinary care. Lancet Neurol 9:177–189. https://doi.org/10.1016/S1474-4422(09)70272-8
Ryder S, Leadley RM, Armstrong N et al (2017) The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis 12:79. https://doi.org/10.1186/s13023-017-0631-3
Grover M, Bachrach LK (2017) Osteoporosis in children with chronic illnesses: diagnosis, monitoring, and treatment. Curr Osteoporos Rep 15:271–282. https://doi.org/10.1007/s11914-017-0371-2
Bianchi ML, Mazzanti A, Galbiati E et al (2003) Bone mineral density and bone metabolism in Duchenne muscular dystrophy. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 14:761–767. https://doi.org/10.1007/s00198-003-1443-y
Tsaknakis K, Jäckle K, Lüders KA et al (2022) Reduced bone mineral density in adolescents with Duchenne muscular dystrophy (DMD) and scoliosis. Osteoporos Int 33:2011–2018. https://doi.org/10.1007/s00198-022-06416-9
Joseph S, Wang C, Bushby K et al (2019) Fractures and linear growth in a nationwide cohort of boys with Duchenne muscular dystrophy with and without glucocorticoid treatment: results from the UK NorthStar Database. JAMA Neurol 76:701–709. https://doi.org/10.1001/jamaneurol.2019.0242
Nagin DS (2014) Group-based trajectory modeling: an overview. Ann Nutr Metab 65:205–210. https://doi.org/10.1159/000360229
Nagin DS, Odgers CL (2010) Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 6:109–138. https://doi.org/10.1146/annurev.clinpsy.121208.131413
Liu C, Yang D-D, Zhang L et al (2022) Bone mineral density assessment by quantitative computed tomography in glucocorticoid-treated boys with Duchenne muscular dystrophy: a linear mixed-effects modeling approach. Front Endocrinol 13:860413. https://doi.org/10.3389/fendo.2022.860413
Lee J-S, Kim K, Jeon YK et al (2020) Effects of traction on interpretation of lumbar bone mineral density in patients with Duchenne muscular dystrophy: a new measurement method and diagnostic criteria based on comparison of dual-energy X-ray absorptiometry and quantitative computed tomography. J Clin Densitom Off J Int Soc Clin Densitom 23:53–62. https://doi.org/10.1016/j.jocd.2018.07.006
Adams JE, Engelke K, Zemel BS et al (2014) Quantitative computer tomography in children and adolescents: the 2013 ISCD Pediatric Official Positions. J Clin Densitom Off J Int Soc Clin Densitom 17:258–274. https://doi.org/10.1016/j.jocd.2014.01.006
Aarestrup J, Blond K, Vistisen D et al (2022) Childhood body mass index trajectories and associations with adult-onset chronic kidney disease in Denmark: a population-based cohort study. PLoS Med 19:e1004098. https://doi.org/10.1371/journal.pmed.1004098
Klijn SL, Weijenberg MP, Lemmens P et al (2017) Introducing the fit-criteria assessment plot – a visualisation tool to assist class enumeration in group-based trajectory modelling. Stat Methods Med Res 26:2424–2436. https://doi.org/10.1177/0962280215598665
Van De Schoot R, Sijbrandij M, Winter SD et al (2017) The GRoLTS-Checklist: guidelines for reporting on latent trajectory studies. Struct Equ Model Multidiscip J 24:451–467. https://doi.org/10.1080/10705511.2016.1247646
Abrams SA (2003) Normal acquisition and loss of bone mass. Horm Res 60(Suppl 3):71–76. https://doi.org/10.1159/000074505
Tsaknakis K, Jäckle K, Lüders KA et al (2022) Reduced bone mineral density in adolescents with Duchenne muscular dystrophy (DMD) and scoliosis. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 33:2011–2018. https://doi.org/10.1007/s00198-022-06416-9
Bell JM, Shields MD, Watters J et al (2017) Interventions to prevent and treat corticosteroid-induced osteoporosis and prevent osteoporotic fractures in Duchenne muscular dystrophy. Cochrane Database Syst Rev 1:CD010899. https://doi.org/10.1002/14651858.CD010899.pub2
Gloss D, Moxley RT, Ashwal S, Oskoui M (2016) Practice guideline update summary: corticosteroid treatment of Duchenne muscular dystrophy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 86:465–472. https://doi.org/10.1212/WNL.0000000000002337
McAdam LC, Rastogi A, Macleod K, Douglas Biggar W (2012) Fat embolism syndrome following minor trauma in Duchenne muscular dystrophy. Neuromuscul Disord NMD 22:1035–1039. https://doi.org/10.1016/j.nmd.2012.07.010
Birnkrant DJ, Bushby K, Bann CM et al (2018) Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol 17:251–267. https://doi.org/10.1016/S1474-4422(18)30024-3
Birnkrant DJ, Bushby K, Bann CM et al (2018) Diagnosis and management of Duchenne muscular dystrophy, part 3: primary care, emergency management, psychosocial care, and transitions of care across the lifespan. Lancet Neurol 17:445–455. https://doi.org/10.1016/S1474-4422(18)30026-7
Biggar WD, Skalsky A, McDonald CM (2022) Comparing deflazacort and prednisone in Duchenne muscular dystrophy. J Neuromuscul Dis 9:463–476. https://doi.org/10.3233/JND-210776
Karaguzel G, Holick MF (2010) Diagnosis and treatment of osteopenia. Rev Endocr Metab Disord 11:237–251. https://doi.org/10.1007/s11154-010-9154-0
Crabtree NJ, Adams JE, Padidela R et al (2018) Growth, bone health & ambulatory status of boys with DMD treated with daily vs. intermittent oral glucocorticoid regimen. Bone 116:181–186. https://doi.org/10.1016/j.bone.2018.07.019
Rizzoli R, Biver E (2015) Glucocorticoid-induced osteoporosis: who to treat with what agent? Nat Rev Rheumatol 11:98–109. https://doi.org/10.1038/nrrheum.2014.188
Funding
This work was supported by grants from the Sichuan Science and Technology Support Program (2023YFG0284) and the Chengdu Municipal Health Commission Project (21PJ048).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The sentence beginning 'Better management of primary bone mineral density (BMD) may be able to delay or avoid the onset of adverse bone health outcomes in 5 years in children with DMD' in this article, the text 'in 5 years' should have read 'in the ffth year'.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, L., Zhou, H., Xu, H. et al. Different bone health progression patterns and early-stage risk marker in glucocorticoid-treated ambulatory Duchenne muscular dystrophy. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07018-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07018-3