Abstract
Summary
Information on bone loss in treated non-Hodgkin’s lymphoma patients is limited. In this study, we used CT to analyze bone loss as well as prevalent and incident fractures. We found severe bone loss, a high rate of fractures, and a novel association between bone loss and the international prognostic index.
Introduction
To investigate bone loss and fracture risk in non-Hodgkin-lymphoma (NHL) patients by (i) comparing treatment-related vertebral density (VD) loss in NHL patients with control subjects and (ii) investigating associations of VD loss versus fracture risk. Further, associations of VD loss and clinical parameters were investigated.
Methods
VD of 123 NHL patients was measured pre- and post-treatment in the L1, L2, and L3 vertebrae in routine computed tomography (CT) scans, performed between Jan 2016 and Mar 2017. Control measurements (n = 52) were obtained from CT colonographies between Sept 2003 and Sept 2017 and their subsequent follow-up-exams (10–137 months).
Prevalent and incident (between baseline and follow-up) fractures were assessed in all subjects, and VD loss per year was calculated. Linear regression models were used to (i) compare VD loss between patients and controls and (ii) identify associations between VD loss and clinical parameters. Using logistic regression models, ORs for fractures per SD change in VD were assessed in patients. Analyses were adjusted for age, sex, and contrast application.
Results
NHL patients experienced significantly greater VDL1–3 loss than controls (P = 0.003), and greater VDL1–3 loss was associated with a greater likelihood of incident fractures (OR, [95%-CI], P 1.90, [1.03, 3.51], 0.04). Patients with an initial international prognostic index (IPI) of 5 suffered significantly greater VD loss compared with an IPI of 0 (P = 0.01).
Conclusion
Using VD measurements in routine CT scans, substantial vertebral bone loss in NHL patients could be documented with a high incidence of fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The current incidence rate of non-Hodgkin lymphoma (NHL) is 20 cases/100,000 persons per year, and in 2016, there were 694,704 patients living with NHL within the USA [1]. With advances in therapy, the relative 5-year survival rose from 47% in the 1970s to currently 72%. In diffuse large-B cell lymphoma (DLBCL), cure could be achieved in up to 80% of patients with a complete remission as response to first-line therapy [2,3,4]. Common first-line therapies for different subtypes of B cell-NHL are R-CHOP, a combination of cyclophosphamide, doxorubicin, vincristine, and prednisolone (CHOP) and the monoclonal CD20-antibody rituximab and similar regimens such as R-CODOX-M (rituximab, cyclophosphamide, vincristine, doxorubicin, and methotrexate), R-CVP (rituximab, cyclophosphamide, vincristine, prednisolone), or R-EPOCH (rituximab, etoposide, prednisolone, vincristine, cyclophosphamide, doxorubicin) [5, 6]. Numerous studies have shown an increase in bone loss and fracture risk in patients treated for NHL, and the chemotherapeutics used have been linked to bone loss through various mechanisms [7,8,9,10,11,12]. Furthermore, during a typical treatment cycle, patients receive 100 mg prednisolone/day for 5 days and patients undergo up to six cycles within 18 weeks. With a cumulative dose of 3000 mg prednisolone in 126 days, the average daily dose of prednisolone is 23.8 mg/day within this interval, a dose that has been shown to be capable of significantly increasing the incidence of vertebral fractures [9, 13].
Despite these findings, the majority of patients treated with R-CHOP or similar regimens do not receive osteoporosis preventing medication, and to date, there is inadequate information about the risk of osteoporotic fractures in patients undergoing chemotherapeutic treatment of NHL, as limitations of previous studies include lack of control cohorts or clinical associations with bone loss and small fracture sample sizes [7, 9, 14]. Moreover, current treatment guidelines (e.g., the National Comprehensive Cancer Network and the European Society for Medical Oncology for the treatment of DLBCL) neither require pre-treatment bone mineral density (BMD) assessments nor do they implement treatments for accelerated BMD loss [9, 15, 16].
The purpose of our study was therefore (i) to compare treatment-related vertebral density loss (VD) in NHL patients with control subjects, (ii) to investigate associations between baseline VD and VD loss and prevalent as well as incident fractures, and (iii) to identify patients at risk of severe VD loss and osteoporotic fractures. The overarching and long-term goal of this study was to provide pertinent information on risk factors of treatment-associated bone loss in NHL patients and associated osteoporotic fractures and thus justify preventative therapies, such as administration of bone preserving medication by clinicians.
Methods
Subject selection
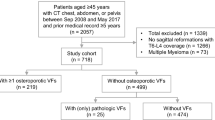
Patients seen at our institution between Jan 1, 2016 and Mar 31, 2017 were retrospectively identified through our clinical database and screened for the following study inclusion criteria: (i) diagnosis of high-grade B cell lymphoma (e.g., DLBCL), (ii) first-line therapy with R-CHOP or similar intensive regimen, (iii) availability of staging computed tomography of the chest, abdomen, and pelvis (CAP) at baseline and after first-line treatment (closest to 12 months). To reduce the impact of differences in bone marrow attenuation due to contrast enhancement, baseline and follow-up CAP-scans were required to be either both contrast-enhanced or both without contrast administration [17]. By reviewing patient medical records, we obtained baseline variables: age, body mass index (BMI), sex, lactate dehydrogenase (LDH), stage of disease at diagnosis, presence of bone marrow involvement, receipt of radiation therapy (other than lumbar spine), use of bone active medication (e.g., vitamin D, calcium, bisphosphonates), the chemotherapy regimen utilized as well as the number of cycles and response to therapy. Moreover, the international prognostic index (IPI) score was calculated in patients, which is a prognostic tool based on five parameters (age, Ann Arbor stage of disease, Eastern Cooperative Oncology Group (ECOG) performance status, serum LDH level, extranodal manifestation) [18]. IPI scores were not calculated in four of 123 patients due to incomplete data. Patients were assigned to risk groups based on individual IPI scores (IPI risk: low, intermediate low, intermediate high and high), as previously reported [19]. Exclusion criteria included lymphoma manifestations within the spine and status post radiation therapy including lumbar spine and pelvis. Using the defined criteria, 123 patients with 246 CAP CT scans at two time points were included in this analysis.
Subjects for the control cohort were selected from our PACS database using the following inclusion and exclusion criteria: (1) two non-contrast–enhanced CT scans of the abdomen and pelvis with at least 10 months between the exams, (2) no history of cancer or any type of chemotherapy during observation interval, and (3) no bone active medication at any time during or before the exams. In order to minimize the possible effects of different study protocols, the included exams were limited to CT colonographies. Information on systemic corticosteroid use and associated comorbidities (asthma, chronic obstructive pulmonary disease and rheumatologic disorders) were documented in all control subjects. Using the defined inclusion and exclusion criteria, a total of 52 subjects could be implemented in our control cohort.
CT imaging
Images for the case cohort were acquired using multidetector CT (Discovery 750 HD, Lightspeed VCT 64) and PET/CT (Discovery STE 16) scanners (GE Healthcare, Waukesha, WI, USA) using standard clinical routine imaging protocols: peak voltage 120 kVp, Pitch 0.984, 150 mAmin, 570 mAmax. For contrast-enhanced imaging studies, 0.5–0.7-ml/kg bodyweight Omnipaque 350 (GE Healthcare, Waukesha, WI, USA) was administered at 3 ml/s, and images were obtained in the portal-venous phase, 80 s after contrast administration. Images were reconstructed with a slice thicknesses of 1.25 mm, 2.5 mm, and 5 mm in the axial plane routinely. In addition, coronal and sagittal reformations were obtained in all patients with a slice thickness of 3 mm and 5 mm, respectively. Consistent slice thickness was used at baseline and follow-up, if available. In cases lacking consistent slice thickness, slices with matching thickness were reconstructed from thinner slices.
Images for the control cohort were acquired with the same set of CT scanners using the department’s standard clinical imaging protocol for virtual colonoscopy: peak voltage 120 kVp, Pitch 1.375, 50 mA. Imaging studies in the control cohort were not contrast enhanced. Axial views with a slice thickness of 1.25 mm were obtained in all exams, and sagittal and coronal reformations were acquired in all patients with a slice thickness of 5 mm and 3 mm, respectively.
Vertebral density measurements
Vertebral density (VD) measurements in Hounsfield units (HU) were obtained from CAP CT scans in the patient cohort and digital colonography CT scans in the control cohort, respectively, using AGFA Impax 6.0 (Agfa-Gevaert, Mortsel, Belgium). Two readers (D.S., J.B.) placed elliptical regions of interest (ROIs) in an axial mid-vertebral slice in L1–3, covering the largest possible area of trabecular bone while excluding cortical bone as previously described [20]. Vertebrae with pathological changes (e.g., fractures or other deformities) were excluded from the analysis. Use of HU as a surrogate measure for BMD has been previously described and validated by Pickhardt et al. [17, 21]. Figure 1b shows an axial section through L1 with an elliptical ROI placed for HU measurements.
Assessment of vertebral density (VD) and vertebral fractures. Vertebrae with pathologic changes (e.g., fractures) were excluded from VD measurements. a Left: Pre-treatment CT exam. L2 (►) is intact. Right: Incident fracture of L2 (►) during treatment. Of note, new disc vacuum phenomenon can be observed in L1/2. b Left: Sagittal view of the lumbar spine with slice orientation of the axial view (horizontal line). Right: Axial view of L3 with region of interest (ROI) placement for vertebral density measurements. The elliptical ROI is placed on mid-height of the vertebral body, excluding cortical bone and the basivertebral foramen (★)
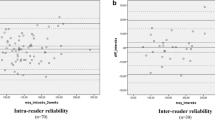
Interobserver reproducibility measurements for VD were obtained in 30 vertebrae by two readers (T.M.L and J.B.). Intra-observer reproducibility measurements were performed by a single reader (J.B.) with at least 4 weeks between both readings.
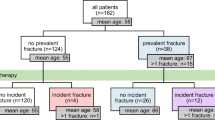
Fracture assessment and patient cohort sub-groups
Fractures were documented in both cohorts using methods similar to those described by Bauer et al. [22]. Fractures of the hips, pelvis, spine, and ribs were defined as “overall” fractures. “Spine” fractures were also documented separately. All fractures were assessed on axial, sagittal, and coronal reconstructions of each CT exam at baseline and individual follow-up. Exams were read by two radiologists in consensus (patient cohort: D.S. (5 years of experience), T.M.L. (25 years of experience); control cohort: J.B. (3 years of experience) and T.M.L.). Deformities of the vertebral bodies with more than 20% height loss were defined as fractures according to Genant et al. [23]. Figure 1a shows an incident fracture at the lumbar spine. Individuals in the patient cohort were assigned to groups (fracture versus no fracture) for prevalent and incident fractures, respectively. Incident fractures were defined as fractures that occurred between the baseline and follow-up CT exam of each individual, respectively. Fracture numbers in the control cohort were too low to assign corresponding groups.
Statistical analyses
Statistical analyses were performed using STATA software, version 15 (StataCorp, College Station, TX, USA) with a two-sided threshold of P < 0.05. Differences in subject characteristics between patient and control cohorts were calculated using a Pearson’s chi-square test for the categorical variable (sex) and linear regression models for continuous variables (age, BMI, follow-up interval). The average VD (VDL1–3) was calculated as average of VDL1, VDL2, and VDL3, at baseline and follow-up, in each individual. Further, absolute and percent changes in VD per year were calculated for each measurement and the average VD (L1, L2, L3, L1–3), by subtracting baseline values from follow-up values, on an individual basis. VDL1–3 was defined as primary outcome, while VDL1, L2, L3 were treated as secondary outcomes. Coefficients of variation (CVs) for repeated VD measurements were calculated to determine the reproducibility of ROI placement.
Baseline VD
Linear regression models were used to compare baseline VD between the control and patient cohorts. Using logistic regression models, odds for prevalent and incident fractures per 1 SD difference in VD were calculated. Baseline VDL1–3 of controls with prednisone use or pre-existing comorbidities (mentioned above) was compared with the remaining control cohort using a linear regression model.
Change in VD
Linear regression models were used to compare change in VD per year (absolute and percent) between the patient and control cohorts. Logistic regression models were used to determine the odds for fractures (prevalent and incident) in patients with greater change in VD (percent). Percent VDL1–3 loss in controls with prednisone use or pre-existing comorbidities (mentioned above) was compared with the remaining control cohort using a linear regression model.
In order to facilitate interpretation, logistic regression models used standardized values for baseline VD and VD loss (percent). Standardized values were calculated by subtracting the mean VD across all cases from individual values and dividing by the standard deviation (SD). Implementing a post hoc power analysis, the probability of a true significant difference in percent VDL1–3 loss between patients and controls was investigated (power = 80%, alpha = 0.05, N2/N1 = 0.4228, mean difference = 19, SD1 = 3; SD2 = 21). Further, the minimal sample size required to find significant differences was retrospectively calculated.
Clinical parameters
Linear regression models were used to determine associations between categorical (IPI risk, bone marrow involvement, use of bone active medication (e.g., vitamin D, calcium, bisphosphonates), chemotherapy regimen, response to therapy), and continuous (BMI, IPI score, number of treatment cycles) clinical parameters and VDL1–3 loss (percent) in the patient cohort.
All regression models were adjusted for age, sex, and contrast administration. Statistical adjustments were implemented to account for potential confounding variables that are associated with both the exposure and outcome [24]. A sensitivity analysis was conducted to determine if the results differ with and without adjustment for intravenous contrast.
Results
Cohort characteristics
A total of 296 NHL patients were seen at our institution between January 2016 and March 2017. Of those, 89 were excluded due to missing baseline and/or follow-up CT scans. Four patients were treated with rituximab as single-agent and 27 received other chemotherapy regimens prior or during the study and were thus excluded. Of the remaining 176 patients, imaging in 53 was not consistently performed with or without contrast. No further exclusions were made due to skeletal deformities or poor-quality scans. The remaining 123 individuals were included in the patient cohort. A summary of subject characteristics for patient and control cohorts as well as patient cohort sub-groups is provided in Table 1. Subject age was significantly different in patient and control cohorts (mean ± SD, controls: 67.04 ± 8.92; patients: 59.19 ± 15.27, P = 0.001). Moreover, the percentage of females was significantly greater in the control cohort compared with the patient cohort. DLBCL (112 (91.06)) and other high-grade b cell lymphomas (5 (4.07)) accounted for most of NHL cases, while primary mediastinal B cell lymphoma (PMBCL) accounted for 6 (4.88) cases. Out of 123 individuals in our patient cohort, scans in 102 were contrast-enhanced.
Follow-up intervals ranged from 4 to 17 months in the patient cohort and from 10 to 137 months in the control cohort. A total of 66 prevalent fractures (39 vertebral fractures) were observed in 28 patients. While nine of the patients had only one prevalent, the average number of fractures was 2.64. In 16 patients with incident fractures, we found 27 “overall” fractures, of which 17 were vertebral fractures. Only one patient suffered both, an incident vertebral fracture and three more incident fractures at the ribs. Use of systemic corticosteroids was found in one control subject, three controls were diagnosed with chronic obstructive pulmonary disease and two with asthma at the time of inclusion.
Baseline vertebral density and fractures
Inter- and intra-observer reproducibility for VD measurements both showed excellent agreement with an average coefficient of variation of 2.84% and 1.82%, respectively. Unadjusted baseline average VDL1–3 in the control cohort (mean ± SD; 134.74 HU ± 44.24 HU) was significantly lower compared to the patient cohort (183.14 ± 57.52) (P < 0.001). However, no significant differences were found between cohorts when adjusted for age, sex, and contrast (P = 0.48). Similar observations were made in VDL1, VDL2, and VDL3: While unadjusted analyses showed significantly greater VD in the patient cohort (P < 0.001), differences became insignificant when adjusted for age, sex, and contrast (P ≥ 0.28, respectively). Notably, VDL1–3 in controls with pre-existing COPD, asthma or prednisone use (81.44 ± 21.48) was lower than in the remaining control cohort (141.69 ± 41.70) (P = 0.005). Performing a sensitivity analysis to compare VD measurements in patient and control CT scans without adjustment for contrast demonstrated significantly higher VD in the patient cohort (P < 0.001, respectively).
No significant differences in VD were observed in patients with prevalent or incident fractures compared with patients without fractures (“overall” and “spine”, respectively) (P ≥ 0.05, for VDL1–3 and VDL1, L2, L3, respectively) (Table 2). However, statistical trends towards lower VD were observed in the prevalent spine fracture subgroup, for the primary outcome VDL1–3 and the secondary outcome VDL1 (P = 0.08 and 0.05, respectively). Moreover, patients with incident spine fractures during follow-up interval showed a trend towards lower VDL1–3 (143.48 HU ± 46.16 HU) compared with patients without incident spine fractures (187.42 HU ± 57.16) (P = 0.05). Statistical trends suggesting a greater likelihood of prevalent spine fractures were found per 1 SD increase in VDL1–3 and the secondary outcome VDL1 (OR [95%-CI], P value; 1.79 [0.91, 3.55], 0.09 and 2.11 [0.97, 4.60], 0.06, respectively) (Table 2).
Patients with lower VDL1–3 at baseline showed significantly increased likelihood of incident spine fractures during the follow-up interval (OR, [95%-CI], P value; 3.00, [1.08, 8.32], 0.04). In the secondary analyses, decreased VDL2 and VDL3 were also associated with an increased likelihood of incident spine fractures. However, these findings remained statistical trends (OR [95%-CI]; VDL2 2.59 [0.85, 7.93], 0.1; VDL3 2.57 [0.87, 7.55], 0.09). No significant associations were observed for any baseline VD measurements and prevalent or incident overall fractures.
Vertebral density loss and associations with incident and prevalent fractures in patients
Significantly greater absolute VD loss (HU/year) was found in patients for the primary (VDL1–3) and all secondary outcomes (VDL1, L2, L3), compared with controls (P ≤ 0.02, respectively), adjusted for age, sex, and contrast (Table 3). Differences between cohorts were even more evident in percent VD loss per year: Mean percent VDL1–3 loss in the patient cohort (− 20.96 ± 20.96) was significantly greater than in the control cohort (− 2.10 ± 2.73) (P = 0.004), and similar results were found for secondary outcomes (VDL1, L2, L3) (P < 0.001, respectively). Percent VDL1–3 loss in controls with pre-existing COPD, asthma, or prednisone use was not significantly different from the remaining control cohort (P = 0.75). Performing a sensitivity analysis to compare VD measurements in patient and control CT scans without adjustment for contrast demonstrated also significantly higher VD loss in the patients (P < 0.001, for absolute and percent loss, respectively). The power of the analysis investigating differences in percent VDL1–3 loss between patients and controls was found to be 1.00, and the minimal required sample size was found to be 8 individuals per cohort.
In patient cohort sub-groups, percent VDL1–3 loss was found to be significantly increased in the incident spine fracture subgroup (− 25.71% ± 21.35%) compared with the no incident spine fracture subgroup (− 15.83% ± 13.58%) (P = 0.04) (Table 4). VDL1 loss (%/year) was also greater in the patient subgroup with incident spine fractures (− 24.87% ± 19.61%) compared with those without (− 14.92% ± 13.86%); however, this result remained only a statistical trend (P = 0.08).
Investigating the associations between VD loss and risk of incident fractures, percent VDL1–3 loss per year was found to be significantly associated with an increased likelihood of incident spine fractures (1.90 [1.03, 3.51], P = 0.04) during the follow-up interval. Percent VDL2 loss was also associated with a greater risk of incident spine fractures, but the association remained a statistical trend (OR [95%-CI] 1.81 [0.92, 3.56], 0.09). No significant associations were found for percent VD-loss per year during the follow-up interval and prevalent fractures at baseline, and no significant results were found for the overall fracture sub-groups. Dropping the adjustment for contrast in the sensitivity analysis did not affect the results: VDL1–3 loss (%/year) in the incident fracture subgroup was significantly greater compared with the no incident fracture subgroup, with and without adjustment for contrast (P = 0.04 and 0.03, respectively).
Associations between vertebral density loss and clinical parameters
Distribution of clinical parameters in the patient cohort is provided in Table 5. Patients with a high risk (IPI risk) had significantly greater percent VDL1–3 loss (− 22.80% ± 16.98%) compared with patients with low risk (− 14.01% ± 11.89%) (coefficient, [95%-CI], P value; − 10.13 [− 17.87, − 2.40], 0.01), and patients with intermediate low risk trended to have greater VDL1–3 loss than low-risk patients (− 5.46 [− 11.72, 0.80], 0.09). Moreover, a significantly greater percent VDL1–3 loss was observed per one increase in IPI score in patients (− 2.60 [− 4.58, − 0.63], 0.01).
Notably, elevated LDH levels, which are part of the IPI scoring system, were not significantly correlated with increased VDL1–3 loss (P ≥ 0.25, respectively). Neither NHL subtype nor the chemotherapy regimen or stage of disease at diagnosis was significantly correlated with VDL1–3 loss (P > 0.05). Significant findings remained unchanged after dropping the adjustment for contrast in the sensitivity analysis (IPI score: P = 0.01; IPI risk (high vs. low): P = 0.01), and the trend towards greater VDL1–3 loss in patients with intermediate low risk versus patients with low risk persisted (P = 0.09).
Discussion
In this study, we analyzed VD loss in patients undergoing chemotherapeutic treatment of NHL versus non-lymphoma controls and its association with prevalent and incident fractures during treatment. We found that VD loss in all vertebral bodies was substantially greater in the NHL patient cohort compared with the control cohort. Moreover, we were able to identify two key factors, which provide novel information on bone loss in NHL patients and associated fractures: (i) Patients with low baseline VD were significantly more likely to suffer spine fractures during the treatment interval, and (ii) the international prognostic index score (IPI) was significantly associated with VDL1–3 loss in patients undergoing therapy and high-risk patients (initial IPI score ≥ 4) suffered significantly greater treatment-associated bone loss, which itself is also significantly associated with a higher fracture incidence.
Previous studies have shown that 30–60% of osteoporotic fractures among men and around 30% among perimenopausal women are connected to secondary causes [25, 26]. Chemotherapeutics, such as cyclophosphamide, doxorubicin and prednisolone, which are being used in NHL treatment, may induce secondary osteoporosis through different mechanisms [9, 10, 12]: Cyclophosphamide is capable of inducing a secondary hypogonadism, leading to substantial bone resorption, while doxorubicin in contrast has been shown to play a role in the direct inhibition of bone formation [27, 28]. Prednisolone induces osteoporosis by multiple, complex mechanisms, including a reduction of gastrointestinal calcium absorption and an increase of urinary calcium excretion [29]. Therefore, the 2017 American College of Rheumatology guideline suggests preventive measures for adults taking doses of prednisolone of ≥ 2.5 mg/day, doses that NHL patients receiving chemotherapy regimens including prednisolone (e.g., R-CHOP) regularly exceed. Recommendations for this group include the optimization of calcium intake (1000–1200 mg/day) and vitamin D intake (600–800 IU/day). Furthermore, oral bisphosphonates are suggested for adults of the age of 40 or older with a moderate or major fracture risk, assessed using the fracture risk assessment tool FRAX (https://www.shef.ac.uk/FRAX/tool.jsp) [30].
However, despite the fact that increased BMD loss in patients treated with R-CHOP for DLBCL is known, current guidelines for the treatment of NHL, such as the ESMO or NCCN guidelines, do not include recommendations on BMD assessment or osteoporosis prophylaxis before and during NHL treatment [9, 15, 16]. We found a significantly increased likelihood of incident spine fractures in patients with low baseline VDL1–3, which had received R-CHOP or similar chemotherapy regimens. As these findings demonstrate, identification of patients at vertebral fracture risk by assessing VD in pre-treatment staging scans is feasible. This novel information may further be used to determine whether fracture-preventing action should be initiated.
Numerous risk factors for severe loss of BMD like age, sex, previous fractures, and calcium deficiency have already been identified [31, 32]. Elevated LDH levels at the point of diagnosis have been reported to be associated with increased BMD loss measured by dual x-ray absorptiometry (DXA) by Paccou et al. [8]. LDH is one of five factors determining the IPI score, which is used to initially determine an NHL patient’s prognosis. While we did not find elevated bone loss in subjects with increased baseline LDH, we found a significant association between initial IPI and percent VDL1–3 loss. Moreover, significantly greater VDL1–3 loss in patients with “high risk” compared with “low risk” was found [19]. The interaction of LDH and other factors (age, Ann Arbor stage of disease, Eastern Cooperative Oncology Group (ECOG) performance status, and extranodal lymphoma manifestations) may thus have a stronger effect on VD loss than each factor individually. Since assessment of IPI scores is already established, identification of this score as risk factor for bone loss may provide substantial benefits for patients. Thus, this novel finding of an association between IPI and therapy-associated VD loss may serve as subject of future investigations.
We found a tenfold greater percent VDL1–3 loss per year in the patient cohort compared with the control cohort, providing evidence for the severity of CHOP-like chemotherapy-induced bone density loss. Similarly, high VD loss in NHL patients has been reported previously; however, this study did not include a control cohort [9]. By adding a control cohort, we were able to provide context to the severity of bone loss NHL patients experience. This finding is also emphasized by our control cohort’s mean age and sex distribution: Mean age was significantly greater in controls compared with the patient cohort, and the percentage of females in controls was significantly higher. Both of these characteristics are risk factors for bone loss; thus, our study design rather tended to underestimate the severity of VD loss in patients.
The likelihood of incident fractures was significantly increased in patients experiencing greater VDL1–3 loss during the follow-up interval. Thus, VD monitoring during treatment may also help in identifying subjects with substantial treatment–associated bone loss at risk of fractures, enabling preventive action. Possible measures to prevent fracture may include, but are not limited to, calcium and vitamin D supplementation and bisphosphonate use [33,34,35]. Moreover, the monoclonal anti-receptor activator of nuclear factor κ B (RANK)-ligand antibody denosumab has shown promising results by reducing fracture risk and increasing BMD [36, 37]. However, these results were observed in postmenopausal females undergoing breast cancer treatment and childhood cancer survivors. To the author’s best knowledge, no similar studies on the efficacy of denosumab in NHL patients have been conducted yet; thus, the applicability remains unclear.
In our patient cohort, 15 patients suffered incident fractures during the follow-up interval. The absolute number of fractures in our cohort was comparably large to other studies [8, 38]. However, our relative fracture incidence matches previously reported incidences per year among cancer patients of about 12–14% [9, 11]. Information on clinical and fracture data were previously reported. This dramatically high fracture incidence rate among cancer patients emphasizes the urgency to find practical screening methods to identify individuals in need of further diagnostic and therapeutic measures.
The measurement of VD in CT as a surrogate marker for BMD is a validated method that has been shown to provide reproducible results in previous studies [17, 39,40,41]. With decreasing radiation doses per scan and increasing number of scans per year, CT data are becoming increasingly available for larger patient cohorts [42]. Especially in cancer patients, who regularly undergo staging CT exams, scans are widely available and thus being investigated as possible opportunistic osteoporosis screening methods [20, 39]. Results of the reproducibility analysis for repeated VD measurements were excellent. Thus, we used routine clinical staging CT scans and digital colonography CT scans to assess VD measurements in our cohorts. Moreover, we used a published and validated method by Bauer et al. for fracture assessment, which was performed by two readers in consensus [22].
We acknowledge some limitations of our study. Sample sizes in our study sub-cohorts were relatively small. This may explain observed trends in our analyses, which did not reach statistical significance. However, the incidence of NHLs compared with other cancer types is relatively low. Despite the number of cases, we were able to demonstrate significant results regarding the association between average VD and spine fractures, and we could identify high IPI scores as potential risk factors for VD loss, an association that to our best knowledge has not been reported before. Future studies with bigger cohorts may be able to further investigate these associations. One variable determining a patient’s IPI is age, and age is a well-known risk factor for osteoporosis [31]. Age may have acted as confounder in associations found between VD loss and IPI in this study. However, all analyses were adjusted for patient age, and significant associations between IPI risk and VD loss were confined to the high-risk group, with IPI scores of 4–5. Thus, the impact of age on the associations found should be very limited. Due to the study design, analyzing the impact of individual chemotherapeutics on VD was not feasible, and this topic requires further investigation, particularly in light of possible dose reductions. However, from a clinical view, CHOP-like regimens are commonly used to treat NHL, and thus, particularly combined therapies with multiple drugs seem relevant. As our analyses were not adjusted for radiation therapy, scatter radiation may have impacted VD measurements in our patient cohort. Previous studies have shown that radiotherapy-induced bone loss strongly correlates with the radiation site, and also demonstrated excellent precision in modern radiotherapy [43, 44]. As patients with radiotherapy of the lumbar spine and pelvis were excluded from this study, the authors chose not to adjust for radiation therapy in favor of avoiding over-adjustment. Further, analyses were not adjusted for the stage of disease, possibly impacting the results of VD measurements, which are not tissue specific. However, as IPI was investigated as a clinical predictor, we preferred not to adjust for this clinical parameter. We used VD measurements as a surrogate marker for BMD. BMD measurements derived from DXA and quantitative CT (QCT) remain the reference standard in the diagnosis of osteoporosis. Nevertheless, VD has been shown to significantly correlate with BMD in various scenarios [20, 39,40,41]. Thus, especially in the context of opportunistic assessment, measuring VD is a useful method to investigate osteoporosis. Study protocols in control and patient cohort were different. However, VD measurements derived from virtual colonoscopies (control cohort) and VD measurements from enhanced and unenhanced routine abdominal CT exams have both been shown to significantly correlate with DXA-derived BMD measurements [20, 40, 41]. Moreover, similar study protocols were used in each individual for baseline and follow-up, respectively, further limiting the impact of study protocols on calculated VD loss per year.
In summary, identification of non-Hodgkin’s lymphoma (NHL) patients treated with CHOP-like chemotherapy regimens at risk of fragility fractures of the spine using routine CT-scan–derived vertebral density measurements is feasible. NHL patients suffer from significantly greater VD loss compared with controls and dramatically increased fracture risk under treatment. Fracture risk was found to be significantly increased in patients with lower baseline VD and in patients with greater percent VD loss per year, while high-risk individuals with an initial IPI score of 4–5 experienced significantly accelerated VD loss compared with patients with low risk (IPI score of 0–1). Thus, early and thorough clinical evaluation, necessary for the assessment of IPI, may help to identify patients at risk for therapy-induced bone loss. Given that (PET-)CT exams are part of standard clinical care in NHL patients, they may serve as opportunistic screening methods, to identify patients in need of further osteoporosis-specific diagnostic techniques (e.g., DXA, QCT) or drug treatment. Furthermore, due to the severe treatment-associated bone loss in NHL patients, intensified BMD surveillance of patients receiving CHOP-like chemotherapy regimens may be considered.
Data availability
Not applicable.
References
SEER Cancer Stat Facts: Non-Hodgkin lymphoma. National Cancer Institute. Bethesda, MD. https://seer.cancer.gov/statfacts/html/nhl.html. Accessed 10/11 2019
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346(4):235–242. https://doi.org/10.1056/NEJMoa011795
Pfreundschuh M, Schubert J, Ziepert M, Schmits R, Mohren M, Lengfelder E, Reiser M, Nickenig C, Clemens M, Peter N, Bokemeyer C, Eimermacher H, Ho A, Hoffmann M, Mertelsmann R, Trumper L, Balleisen L, Liersch R, Metzner B, Hartmann F, Glass B, Poeschel V, Schmitz N, Ruebe C, Feller AC, Loeffler M (2008) Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20+ B-cell lymphomas: a randomised controlled trial (RICOVER-60). Lancet Oncol 9(2):105–116. https://doi.org/10.1016/s1470-2045(08)70002-0
Pfreundschuh M, Kuhnt E, Trumper L, Osterborg A, Trneny M, Shepherd L, Gill DS, Walewski J, Pettengell R, Jaeger U, Zinzani PL, Shpilberg O, Kvaloy S, de Nully BP, Stahel R, Milpied N, Lopez-Guillermo A, Poeschel V, Grass S, Loeffler M, Murawski N (2011) CHOP-like chemotherapy with or without rituximab in young patients with good-prognosis diffuse large-B-cell lymphoma: 6-year results of an open-label randomised study of the MabThera International Trial (MInT) group. Lancet Oncol 12(11):1013–1022. https://doi.org/10.1016/s1470-2045(11)70235-2
Marcus R, Imrie K, Belch A, Cunningham D, Flores E, Catalano J, Solal-Celigny P, Offner F, Walewski J, Raposo J, Jack A, Smith P (2005) CVP chemotherapy plus rituximab compared with CVP as first-line treatment for advanced follicular lymphoma. Blood 105(4):1417–1423. https://doi.org/10.1182/blood-2004-08-3175
Dunleavy K, Pittaluga S, Maeda LS, Advani R, Chen CC, Hessler J, Steinberg SM, Grant C, Wright G, Varma G, Staudt LM, Jaffe ES, Wilson WH (2013) Dose-adjusted EPOCH-rituximab therapy in primary mediastinal B-cell lymphoma. N Engl J Med 368(15):1408–1416. https://doi.org/10.1056/NEJMoa1214561
Cabanillas ME, Lu H, Fang S, Du XL (2007) Elderly patients with non-Hodgkin lymphoma who receive chemotherapy are at higher risk for osteoporosis and fractures. Leuk Lymphoma 48(8):1514–1521. https://doi.org/10.1080/10428190701471973
Paccou J, Merlusca L, Henry-Desailly I, Parcelier A, Gruson B, Royer B, Charbonnier A, Ursu D, Desailloud R, Garidi R, Kamel S, Sevestre H, Marolleau JP, Fardellone P, Damaj G (2014) Alterations in bone mineral density and bone turnover markers in newly diagnosed adults with lymphoma receiving chemotherapy: a 1-year prospective pilot study. Ann Oncol 25(2):481–486. https://doi.org/10.1093/annonc/mdt560
Svendsen P, Shekhrajka N, Nielsen KL, Vestergaard P, Poulsen MO, Vistisen AK, Munksgaard PS, Severinsen MT, Jensen P, Johnsen HE, Jakobsen LH, Bogsted M, Frokjaer JB, El-Galaly TC (2017) R-CHOP(-like) treatment of diffuse large B-cell lymphoma significantly reduces CT-assessed vertebral bone density: a single center study of 111 patients. Leuk Lymphoma 58(5):1105–1113. https://doi.org/10.1080/10428194.2016.1233543
Westin JR, Thompson MA, Cataldo VD, Fayad LE, Fowler N, Fanale MA, Neelapu S, Samaniego F, Romaguera J, Shah J, McLaughlin P, Pro B, Kwak LW, Sanjorjo P, Murphy WA, Jimenez C, Toth B, Dong W, Hagemeister FB (2013) Zoledronic acid for prevention of bone loss in patients receiving primary therapy for lymphomas: a prospective, randomized controlled phase III trial. Clin Lymphoma Myeloma Leuk 13(2):99–105. https://doi.org/10.1016/j.clml.2012.11.002
D'Oronzo S, Stucci S, Tucci M, Silvestris F (2015) Cancer treatment-induced bone loss (CTIBL): pathogenesis and clinical implications. Cancer Treat Rev 41(9):798–808. https://doi.org/10.1016/j.ctrv.2015.09.003
Rana T, Chakrabarti A, Freeman M, Biswas S (2013) Doxorubicin-mediated bone loss in breast cancer bone metastases is driven by an interplay between oxidative stress and induction of TGFbeta. PLoS One 8(10):e78043. https://doi.org/10.1371/journal.pone.0078043
van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology (Oxford) 39(12):1383–1389. https://doi.org/10.1093/rheumatology/39.12.1383
Anargyrou K, Fotiou D, Vassilakopoulos TP, Christoulas D, Makras P, Dimou M, Ntanasis-Stathopoulos I, Masouridou S, Angelopoulou MK, Papatheodorou A, Tsionos K, Panayiotidis P, Dimopoulos MA, Terpos E (2019) Low bone mineral density and high bone turnover in patients with non-Hodgkin’s lymphoma (NHL) who receive frontline therapy: results of a multicenter prospective study. Hemasphere 3(6):e303. https://doi.org/10.1097/hs9.0000000000000303
Tilly H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, Lopez-Guillermo A, Walewski J, Andre M, Johnson PW, Pfreundschuh M, Ladetto M (2015) Diffuse large B-cell lymphoma (DLBCL): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26(Suppl 5):v116–v125. https://doi.org/10.1093/annonc/mdv304
Zelenetz AD, Gordon LI, Wierda WG, Abramson JS, Advani RH, Andreadis CB, Bartlett N, Byrd JC, Fayad LE, Fisher RI, Glenn MJ, Habermann TM, Lee Harris N, Hernandez-Ilizaliturri F, Hoppe RT, Horwitz SM, Kaminski MS, Kelsey CR, Kim YH, Krivacic S, AS LC, Lunning M, Nademanee A, Porcu P, Press O, Rabinovitch R, Reddy N, Reid E, Roberts K, Saad AA, Sokol L, Swinnen LJ, Vose JM, Yahalom J, Zafar N, Dwyer M, Sundar H (2016) Diffuse large B-cell lymphoma Version 1.2016. J Natl Compr Cancer Netw 14(2):196–231. https://doi.org/10.6004/jnccn.2016.0023
Lee SJ, Graffy PM, Zea RD, Ziemlewicz TJ, Pickhardt PJ (2018) Future osteoporotic fracture risk related to lumbar vertebral trabecular attenuation measured at routine body CT. J Bone Miner Res 33(5):860–867. https://doi.org/10.1002/jbmr.3383
Blood (1997) A clinical evaluation of the international lymphoma study group classification of non-Hodgkin’s lymphoma. The non-Hodgkin’s lymphoma classification project. Blood 89(11):3909–3918
Shipp (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329(14):987–994. https://doi.org/10.1056/nejm199309303291402
Pickhardt PJ, Lauder T, Pooler BD, Munoz Del Rio A, Rosas H, Bruce RJ, Binkley N (2016) Effect of IV contrast on lumbar trabecular attenuation at routine abdominal CT: correlation with DXA and implications for opportunistic osteoporosis screening. Osteoporos Int 27(1):147–152. https://doi.org/10.1007/s00198-015-3224-9
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93(11):1057–1063. https://doi.org/10.2106/jbjs.J.00160
Bauer JS, Muller D, Ambekar A, Dobritz M, Matsuura M, Eckstein F, Rummeny EJ, Link TM (2006) Detection of osteoporotic vertebral fractures using multidetector CT. Osteoporos Int 17(4):608–615. https://doi.org/10.1007/s00198-005-0023-8
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1148. https://doi.org/10.1002/jbmr.5650080915
Cochran WG, Rubin DB (1973) Controlling bias in observational studies: a review. Sankhya: The Indian Journal of Statistics, Series A (1961–2002) 35(4):417–446
(2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285(6):785–795. https://doi.org/10.1001/jama.285.6.785
Fitzpatrick LA (2002) Secondary causes of osteoporosis. Mayo Clin Proc 77(5):453–468. https://doi.org/10.4065/77.5.453
Kenney LB, Laufer MR, Grant FD, Grier H, Diller L (2001) High risk of infertility and long term gonadal damage in males treated with high dose cyclophosphamide for sarcoma during childhood. Cancer 91(3):613–621
Pfeilschifter J, Diel IJ (2000) Osteoporosis due to cancer treatment: pathogenesis and management. J Clin Oncol 18(7):1570–1593. https://doi.org/10.1200/jco.2000.18.7.1570
Lane NE, Lukert B (1998) The science and therapy of glucocorticoid-induced bone loss. Endocrinol Metab Clin N Am 27(2):465–483. https://doi.org/10.1016/s0889-8529(05)70017-7
Buckley L, Guyatt G, Fink HA, Cannon M, Grossman J, Hansen KE, Humphrey MB, Lane NE, Magrey M, Miller M, Morrison L, Rao M, Robinson AB, Saha S, Wolver S, Bannuru RR, Vaysbrot E, Osani M, Turgunbaev M, Miller AS, McAlindon T (2017) 2017 American College of Rheumatology Guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheum 69(8):1521–1537. https://doi.org/10.1002/art.40137
Holm JP, Hyldstrup L, Jensen J-EB (2016) Time trends in osteoporosis risk factor profiles: a comparative analysis of risk factors, comorbidities, and medications over twelve years. Endocrine 54(1):241–255. https://doi.org/10.1007/s12020-016-0987-5
Ross PD (1998) Risk factors for osteoporotic fracture. Endocrinol Metab Clin N Am 27(2):289–301. https://doi.org/10.1016/s0889-8529(05)70006-2
Delmas P, Balena R, Confravreux E, Hardouin C, Hardy P, Bremond A (1997) Bisphosphonate risedronate prevents bone loss in women with artificial menopause due to chemotherapy of breast cancer: a double-blind, placebo-controlled study. J Clin Oncol 15(3):955–962
Saarto T, Blomqvist C, Välimäki M, Mäkelä P, Sarna S, Elomaa I (1997) Clodronate improves bone mineral density in post-menopausal breast cancer patients treated with adjuvant antioestrogens. Br J Cancer 75(4):602–605
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337(10):670–676
Gnant M, Pfeiler G, Dubsky PC, Hubalek M, Greil R, Jakesz R, Wette V, Balic M, Haslbauer F, Melbinger E, Bjelic-Radisic V, Artner-Matuschek S, Fitzal F, Marth C, Sevelda P, Mlineritsch B, Steger GG, Manfreda D, Exner R, Egle D, Bergh J, Kainberger F, Talbot S, Warner D, Fesl C, Singer CF, Austrian B, Colorectal Cancer Study G (2015) Adjuvant denosumab in breast cancer (ABCSG-18): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 386(9992):433–443. https://doi.org/10.1016/S0140-6736(15)60995-3
Huang T-H, Liu H-C, Hou J-Y, Chang C-Y, Sun F-J, Yeh T-C (2019) Efficacy and safety of denosumab therapy for low bone mineral density in childhood cancer survivors: a report of preliminary experience. Pediatr Blood Cancer 66(10):e27927–e27927. https://doi.org/10.1002/pbc.27927
Kim SH, Lim SK, Hahn JS (2004) Effect of pamidronate on new vertebral fractures and bone mineral density in patients with malignant lymphoma receiving chemotherapy. Am J Med 116(8):524–528. https://doi.org/10.1016/j.amjmed.2003.12.019
Lee SJ, Binkley N, Lubner MG, Bruce RJ, Ziemlewicz TJ, Pickhardt PJ (2016) Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos Int 27(3):1131–1136. https://doi.org/10.1007/s00198-015-3318-4
Pickhardt PJ, Lee LJ, Muñoz del Rio A, Lauder T, Bruce RJ, Summers RM, Pooler BD, Binkley N (2011) Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res 26(9):2194–2203
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158(8):588–595
Brenner DJ, Hall EJ (2007) Computed tomography—an increasing source of radiation exposure. N Engl J Med 357(22):2277–2284
Wei RL, Jung BC, Manzano W, Sehgal V, Klempner SJ, Lee SP, Ramsinghani NS, Lall C (2016) Bone mineral density loss in thoracic and lumbar vertebrae following radiation for abdominal cancers. Radiother Oncol 118(3):430–436. https://doi.org/10.1016/j.radonc.2016.03.002
Baskar R, Lee KA, Yeo R, Yeoh K-W (2012) Cancer and radiation therapy: current advances and future directions. Int J Med Sci 9(3):193–199. https://doi.org/10.7150/ijms.3635
Code availability
Not applicable.
Funding
Open Access funding provided by Projekt DEAL. This study was funded through the NIH/NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases grant R01AR064771). This study was also supported by the grants from the National Scientific Foundation of China (NSFC, Nos. 31630025 and 81320108013).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional review board
This study was approved by the institutional review board and was performed in accordance with the ethical standards defined in the 1964 Declaration of Helsinki and its amendments.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bodden, J., Sun, D., Joseph, G.B. et al. Identification of non-Hodgkin lymphoma patients at risk for treatment-related vertebral density loss and fractures. Osteoporos Int 32, 281–291 (2021). https://doi.org/10.1007/s00198-020-05577-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05577-9