Abstract
Summary
Using case vignette methodology, this study shows that only 4% of patients are maintained on oral bisphosphonates over 5 years, and prescribers switch or stop the treatment in 20–30% of cases at each visit. There are few determinants of these changes. More information on appropriate follow-up could help in patients’ management.
Introduction
Persistence to oral bisphosphonates, the most commonly prescribed anti-osteoporotic treatments, is low. The aim of this study was to evaluate the role of rheumatologists on the treatment patterns, and to assess the determinants of treatment changes.
Methods
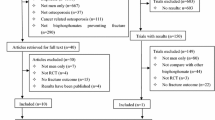
We used the methodology of case vignettes with the participation of 142 rheumatologists. Three baseline clinical vignettes were presented: (1) the physician was asked to indicate the most appropriate period to schedule the next visit over 5 years, (2) the physician was tested about parameters for follow-up (including traps), and (3) various results (both clinical, biological, densitometric, and radiological) were given by random and analyzed as determinants of treatment changes.
Results
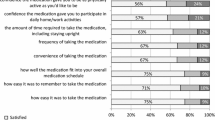
The study allowed assessment of 426 virtual clinical cases. Clinical examinations, patient’s height, inquiries about falls, and adherence to treatment were deemed necessary in > 90% of cases. Bone mineral density was measured in 22, 40, and 71% of cases at 2, 3, and 5 years, respectively. Dental follow-up was recommended in less than 25% of cases. Only 4.2% of patients were maintained on the same treatment at 5 years, and a change of treatment (stop or switch) occurs in 20–30% of cases at each visit. Significant determinants were adherence to treatment, serum C-terminal crosslinking telopeptide of type 1 collagen (CTX) value, change in patient’s height, and the occurrence of an incident vertebral fracture.
Conclusion
Our study shows that maintenance of oral bisphosphonate in postmenopausal women managed by rheumatologists is low; there are few determinants of these changes and more information on appropriate follow-up could help in patients’ management.

Similar content being viewed by others
References
Bliuc D, Milch VE, Nguyen TV et al (2009) Mortality risk, associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoportic Fracture Research Group. Arch Intern Med 159:1215–1220
Black DM, Rosen CJ (2016) Post-menopausal osteoporosis. N Engl J Med 374:254–262
Franek E, Talalaj M, Wichrowska H et al (2008) Common drug switching during long-term antiresorptive treatment: experience of four osteoporosis centers in Poland (2001–2005). Aging Clin Exp Res 20(6):528–532
Blouin J, Dragomir A (2007) Ste.-Marie LG, et al. Discontinuation of antiresorptive therapies: a comparison between 1998–2001 and 2002–2004 among osteoporotic women. J Clin Endocrinol Metab 92:887–894
Netelenbos JC, Geusens PP, Ypma G, Buijs SJE (2011) Adherence and profile of non-persistence in patients treated for osteoporosis—a large-scale, long-term retrospective study in the Netherlands. Osteoporos Int 22:1537–1546
Tosteson ANA, Do TP, Wade SW et al (2010) Persistence and switching patterns among women with varied osteoporosis medication histories: 12-month results from POSSIBLE US™. Osteoporos Int 21:1769–1780
Siris ES, Harris ST, Rosen CJ et al (2006) Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and non-vertebral fractures from 2 US claims database. Mayo Clin Proc 81:1013–1022
Landfeldt E, Ström O, Robbins S, Borgström F (2012) Adherence to treatment of primary osteoporosis and its association to fractures—the Swedish Adherence Register Analysis (SARA). Osteoporos Int 23:433–443
Solomon DH, Brown EM, Chandler D et al (2014) Patterns of treatment among a cohort of older low-income adults starting new medications for osteoporosis. Osteoporos Int 25:2255–2262
Rossini M, Bianchi G, Di Munno O et al (2006) Treatment of osteoporosis in clinical practice. Osteoporos Int 17:914–921
Brookhart MA, Avorn J, Katz JN et al (2007) Gaps in treatment among users of osteoporosis medications: the dynamics of noncompliance. Am J Med 120:151–156
Belhassen M, Confavreux CB, Cortet B et al (2017) Anti-osteoporotic treatments in France: initiation, persistence and switches over 6 years of follow-up. Osteoporos Int 28:853–862
Roux C, Briot K (2014) How long should we treat? Osteoporosis Int 25:1659–1666
Combs BP, Rappaport M, Coverly TJ et al (2013) Due for a scan: examining the utility of monitoring densitometry. JAMA Int Med 173:2007–2009
Yun H, Curtis JR, Guo L et al (2014) Patterns and predictors of osteoporosis medication discontinuation and switching among medicare beneficiaries. BMC Musculoskeletal Disorders 15:112
Bauer DC, Schwartz A, Palermo L et al (2014) Fracture prediction after discontinuation of 4 to 5 years of alendronate therapy: the FLEX study. JAMA Intern Med 174:1126–1134
Cosman F, Cauley JA, Eastell R et al (2014) Reassessment of fracture risk in women after 3 years of treatment with zoledronic acid: when is it reasonable to discontinue treatment? J Clin Endocrinol Metab 99:4546–4554
Schwartz AV, Bauer DC, Cummings SR et al (2010) Efficacy of continued alendronate for fractures in women with and without prevalent vertebral fracture: the FLEX trial. J Bone Miner Res. 25:976–982
Confavreux CB, Canoui-Poitrine F, Schott AM et al (2012) Persistence at 1 year of oral antiosteoporotic drugs: a prospective study in a comprehensive health insurance database. European Journal of Endocrinology 166:735–741
Khan AA, Morrison A, Kendler DL et al (2016) International Task Force on Osteonecrosis of the Jaw. Case-based review of osteonecrosis of the jaw (ONJ) and application of the international recommendations for management from the International Task Force on ONJ. J Clin Densitom Pli:S1094–6950(16):30196–30192
Peabody JW, Luck J, Glassman P, Dersselhaus TR, Lee M (2000) Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA 283:1715–1722
Peabody JW, Luck J, Glassman P et al (2004) Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med 141:771–780
Veloski J, Tai S, Evans AS, Nash DB (2005) Clinical vignette-based surveys: a tool for assessing physician practice variation. Am J Med Qual 20:151–157
Acknowledgements
We are grateful for all physicians who participated in the study.
Funding
The study was funded by AMGEN. The CRO Fast 4 (Director B. Roux) received a grant from AMGEN. The funder did not have any role in the study design, data collection, analysis of data, decision to publish, and preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
C. Roux in occasional interventions received honoraria as an expert or speaker for Alexion, Amgen, Lilly, Pfizer, and UCB. C. Roux also received financial support to research organization from Ultragenyx. G. Baron has none to declare. K. Briot in occasional interventions received honoraria as an expert or speaker for Amgen, Lilly, MSD, and Pfizer. B. Roux received grant from AMGEN. B. Cortet in occasional interventions received honoraria as an expert or speaker for Amgen, Expanscience, Ferring, Lilly (France), MSD, Medtronic, and Roche diagnostics. B. Cortet also received financial support (indirect interests) to a research organization from Amgen and MSD. T. Thomas has received advisory board or speaker fees from Abbvie, Amgen, BMS, Chugai, Expanscience, Gilead, HAC-Pharma, Eli Lilly, Medac, MSD, Teva, Thuasne, and UCB and research grants or investigator fees from Amgen, Bone Therapeutics, Chugai/Roche, HAC-Pharma, LCA, MSD, Novartis, Pfizer, Servier, and UCB.
Rights and permissions
About this article
Cite this article
Roux, C., Baron, G., Briot, K. et al. Management of oral bisphosphonates treatment by rheumatologists and determinants of therapeutic changes: a case-vignette-based study. Osteoporos Int 28, 3339–3345 (2017). https://doi.org/10.1007/s00198-017-4188-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4188-8