Abstract
Summary
One year of high-dose bisphosphonate (BPs) therapy in dogs allowed the increased accumulation of advanced glycation end-products (AGEs) and reduced postyield work-to-fracture of the cortical bone matrix. The increased accumulation of AGEs in these tissues may help explain altered bone matrix quality due to the administration of BPs in animal models
Introduction
Non-enzymatic glycation (NEG) is a posttranslational modification of the organic matrix that results in the formation of advanced glycation end-products (AGEs). In bone, the accumulation of AGEs play an important role in determining fracture resistance, and elevated levels of AGEs have been shown to adversely affect the bone’s propensity to brittle fracture. It was thus hypothesized that the suppression of tissue turnover in cortical bone due to the administration of bisphosphonates would cause increased accumulation of AGEs and result in a more brittle bone matrix.
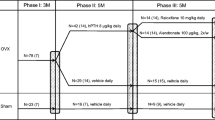
Methods
Using a canine animal model (n = 12), we administered daily doses of a saline vehicle (VEH), alendronate (ALN 0.20, 1.00 mg/kg) or risedronate (RIS 0.10, 0.50 mg/kg). After a 1-year treatment, the mechanical properties, intracortical bone turnover, and the degree of nonenzymatic cross-linking of the organic matrix were measured from the tibial cortical bone tissue of these animals.
Results
There was a significant accumulation of AGEs at high treatment doses (+49 to + 86%; p < 0.001), but not at doses equivalent to those used for the treatment of postmenopausal osteoporosis, compared to vehicle. Likewise, postyield work-to-fracture of the tissue was significantly reduced at these high doses (−28% to −51%; p < 0.001) compared to VEH. AGE accumulation inversely correlated with postyield work-to-fracture (r 2 = 0.45; p < 0.001), suggesting that increased AGEs may contribute to a more brittle bone matrix.
Conclusion
High doses of bisphosphonates result in the accumulation of AGEs and a reduction in energy absorption of cortical bone. The increased accumulation of AGEs in these tissues may help explain altered bone matrix quality due to the administration of BPs in animal models.







Similar content being viewed by others

References
Iwamoto J, Takeda T, Sato Y (2006) Efficacy and safety of alendronate and risedronate for postmenopausal osteoporosis. Curr Med Res Opin 22(5):919–28 May
Rodan GA, Fleisch HA (1996) Bisphosphonates: mechanisms of action. J Clin Invest 97(12):2692–6 Jun 15
Russell RG, Croucher PI, Rogers MJ (1999) Bisphosphonates: pharmacology, mechanisms of action and clinical uses. Osteoporos Int 9(Suppl 2):S66–80
Boivin G, Meunier PJ (2002) Effects of bisphosphonates on matrix mineralization. J Musculoskelet Neuronal Interact 2(6):538–43 Dec
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Delaney MF, Hurwitz S, Shaw J, LeBoff MS (2003) Bone density changes with once weekly risedronate in postmenopausal women. J Clin Densitom 6(1):45–50 Spring
Mashiba T, Turner CH, Hirano T, Forwood MR, Johnston CC, Burr DB (2001) Effects of suppressed bone turnover by bisphosphonates on microdamage accumulation and biomechanical properties in clinically relevant skeletal sites in beagles. Bone 28:524–31
Mashiba T, Hirano T, Turner CH, Forwood MR, Johnston CC, Burr DB (2000) Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res 15:613–20
Allen MR, Iwata K, Phipps R, Burr DB (2006) Alterations in canine vertebral bone turnover, microdamage accumulation, and biomechanical properties following 1-year treatment with clinical treatment doses of risedronate or alendronate. Bone 39(4):872–9 Oct
Komatsubara S, Mori S, Mashiba T, Ito M, Li J, Kaji Y, Akiyama T, Miyamoto K, Cao Y, Kawanishi J, Norimatsu H (2003) Long-term treatment of incadronate disodium accumulates microdamage but improves the trabecular bone microarchitecture in dog vertebra. J Bone Miner Res 18(3):512–20 Mar
Allen MR, Burr DB (2007) Three years of alendronate treatment results in similar levels of vertebral microdamage as after one year of treatment. J Bone Miner Res 22:1759–65
Monnier VM, Kohn RR, Cerami A (1984) Accelerated age-related browning of human collagen in diabetes mellitus. Proc Natl Acad Sci USA 81:583–587
Bailey AJ, Paul RG, Knott L (1998) Mechanisms of maturation and ageing of collagen. Mech of Ageing and Devel 106(1998):1–56
Reiser KM (1984) Nonenzymatic glycation of collagen in aging and diabetes. Proc Soc Exp Biol Med 196(1):17–29
Monnier VM, Sell DR, Abdul-Karim FW, Emancipator SN (1988) Collagen browing and cross-linking are increased in chronic experimental hyperglycemia: relevance to diabetes and ageing. Diabetes 37:867–872
Verzijl N, DeGroot J, Oldehinkel E, Bank RA, Thrope SR, Baynes JW, Bayliss MT, Bijlsma JWJ, Lafeber FPJG, TeKoppele JM (2000) Age-related accumulation of Maillard reaction products in human articular cartilage collagen. Biochem J 350:381–387
Odetti P, Rossi S, Monacelli F, Poggi A, Cirnigliaro F, Federici M, Federici A (2005) Advanced glycation end-products and bone loss during aging. Ann NY Acad Sci 1043:710–7
Vashishth D (2007) The role of the collagen matrix in skeletal fragility. Curr Osteoporos Rep 5(2):62–6 Jun
Vashishth D, Gibson GJ, Khoury JI, Schaffler MB, Kimura J, Fyhrie DP (2001) Influence of nonenzymatic glyation on biomechanical properties of cortical bone. Bone 22(2):195–201
Wang X, Shen X, Li X, Agrawal CM (2002) Age-related changes in the collagen network and toughness of bone. Bone 31(1):1–7
Viguet-Carrin S, Roux J, Arlot M, Merabet Z, Leeming D, Byrjalsen I, Delmas P, Bouxsein M (2006) Contribution of the advanced glycation end product pentosidine and of maturation of type I collagen to compressive biomechanical properties of human lumbar vertebrae. Bone 39(5):1073–9
Tang SY, Zeenath U, Vashishth D (2007) Effects of non-enzymatic glycation on cancellous bone fragility. Bone 40(4):1144–51 Apr
Allen MR, Follet H, Khurana M, Sato M, Burr DB (2006) Antiremodeling agents influence osteoblast activity differently in modeling and remodeling sites of canine rib. Calcif Tissue Int 79(4):255–61 Oct
Woessner JF (1964) The determination of hydroxyproline in tissue and proteins containing small proportions of this imino acid. Arch Biochem and Biophysics 93:440–447
Kivirikko KI, Prockop DJ (1967) Partial characterization of protocollagen from embryonic cartilage. Biochem J 102(2):432–42 Feb
Mashiba T, Hui S, Turner CH, Mori S, Johnston CC, Burr DB (2005) Bone remodeling at the iliac crest can predict the changes in remodeling dynamics, microdamage accumulation, and mechanical properties in the lumbar vertebrae of dogs. Calcif Tissue Int 77(3):180–5 Sep
Monnier VM (2003) Intervention against the Maillard reaction in vivo. Arch Biochem Biophys 419:1–15
Obayashi H, Nakano K, Shigeta H, Yamaguchi M, Yoshimori K, Fukui M, Fujii M, Kitagawa Y, Nakamura N, Nakamura K, Nakazawa Y, Ienaga K, Ohta M, Nishimura M, Fukui I, Kondo M (1996) Formation of crossline as a fluorescent advanced glycation end product in vitro and in vivo. Biochem Biophys Res Commun 226(1):37–41 Sep 4
Tessier F, Obrenovich M, Monnier VM (1999) Structure and mechanism of formation of human lens fluorophore LM-1. Relationship to vesperlysine A and the advanced Maillard reaction in aging diabetes, and cataractogenesis. J Biol Chem 274(30):20796–804 Jul 23
Gibson GJ, Verner JJ, Nelson FR, Lin DL (2001) Degradation of the cartilage collagen matrix associated with changes in chondrocytes in osteoarthrosis. Assessment by loss of background fluorescence and immunodetection of matrix components. J Orthop Res 19(1):33–42 Jan
Dyer DG, Dunn JA, Thorpe SR, Bailie KE, Lyons TJ, McCance DR, Baynes JW (1993) Accumulation of Mallard reaction products in skin collagen in diabetes and aging. J Clin Invest 91:2463–9
Katayama Y, Akatsu T, Yamamoto M, Kugai N, Nagata N (1996) Role of nonenzymatic glycosylation of Type I collagen in diabetic osteopenia. J Bone Miner Res 11:931–937
Vlassara H, Bucala R, Striker L (1994) Pathogenic effects of advanced glycosylation: biochemical, biologic, and clinical implications for diabetes and aging. Lab Invest 70:138–151
Allen MR, Gineyts E, Leeming DJ, Burr DB, Delmas PD (2008) Bisphosphonates alter trabecular bone collagen cross-linking and isomerization in beagle dog vertebra. Osteoporos Int 19(3):329–37 Mar
Yamagishi S, Takeuchi M, Inagaki Y, Nakamura K, Imaizumi T (2003) Role of advanced glycation end products (AGEs) and their receptor (RAGE) in the pathogenesis of diabetic microangiopathy. Int J Clin Pharmacol Res 23:129–134
Kimmel DB, Jee WS (1982) A quantitative histologic study of bone turnover in young adult beagles. Anat Rec 203(1):31–45 May
Burstein AH, Zika JM, Heiple KG, Klein L (1975) Contribution of collagen and mineral to the elastic-plastic properties of bone. J Bone Joint Surg Am 57(7):956–61
Hernandez CJ, Tang SY, Baumbach BM, Hwu PB, Sakkee AN, van der Ham F, DeGroot J, Bank RA, Keaveny TM (2005) Trabecular microfracture and the influence of pyridinium and non-enzymatic glycation-mediated collagen cross-links. Bone 37(6):825–32
Allen MR, Reinwald S, Burr DB (2008) Alendronate reduces bone toughness of ribs without significantly increasing microdamage accumulation in dogs following 3 years of daily treatment. Calcif Tissue Int 82(5):354–60 May
Allen MR, Burr DB (2007) Mineralization, microdamage, and matrix: how bisphosphonates influence material properties of bone. BoneKEy-Osteovision 4:49–60
Tang SY and Vashishth D (2008) A three dimensional analysis and segmentation of microdamage shows compromised microdamage production due to nonenzymatic glycation. Transactions of the 54th Annual Meeting of Orthopedic Research Society. San Francisco, CA, USA.
Acknowledgements
The authors gratefully thank Glenn Berard and Joseph Said for assistance in sample preparation. This work is supported by NIH grants AG20618, AR047838, and AR007581; and a research grant from The Alliance for Better Bone Health (P&G Pharmaceuticals and Sanofi-Aventis). Merck and Co. provided the alendronate. This investigation utilized an animal facility constructed with support from Research Facilities Improvement Program Grant Number C06RR10601 from the NIH National Center for Research Resources.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, S.Y., Allen, M.R., Phipps, R. et al. Changes in non-enzymatic glycation and its association with altered mechanical properties following 1-year treatment with risedronate or alendronate. Osteoporos Int 20, 887–894 (2009). https://doi.org/10.1007/s00198-008-0754-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0754-4