Abstract
Introduction and Hypothesis
The primary objective is to identify determinants of dissatisfaction after surgical treatment of vaginal prolapse ± rectal prolapse, using laparoscopic mesh sacrohysteropexy (LSH) or sacrocolpopexy (LSC) ± ventral mesh rectopexy (VMR). The secondary objective is the evaluation of complications and objective/subjective recurrence rates.
Methods
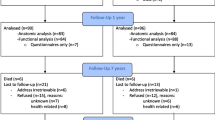
The study performed was a single-surgeon retrospective review of prospectively collected data. LSH/LSC ± VMR were performed between July 2005 and September 2022. Primary investigated outcome was patients’ satisfaction, assessed using the Patient Global Impression of Improvement (PGI-I) score and the bother visual analog scale (VAS) obtained postoperatively (at a 1-month interval and on a 6-month/yearly basis thereafter). We looked for a correlation between the level of satisfaction (as reflected by the VAS) and potential determinants.
Results
There were 355 patients with a mean age of 62 ±12 years. Nearly all the patients (94.3%) had a stage 3 or 4 prolapse according to the POP-Q classification. The mean postoperative bother VAS was 1.8, with only 12.7% of patients reporting a bother VAS score ≥ 3/10, indicating a dissatisfaction. PGI-I showed improvement in the vast majority of patients (96.4% scoring 1 to 3). Patients with anal incontinence preoperatively scored higher on the bother VAS postoperatively (r=0.175, p < 0.05). The use of a posterior arm mesh (for posterior vaginal prolapse) correlated with better satisfaction overall (r= −0.178, p = 0.001), whereas the performance of VMR was associated with a bothering sensation (r = 0.232, p < 0.001). A regression analysis confirmed the impact of posterior mesh and VMR on satisfaction levels, with odds of dissatisfaction being 2.18 higher when VMR was combined with LSH/LSC.
Conclusions
Posterior mesh use improves patient satisfaction when the posterior compartment is affected. In patients with concomitant vaginal and rectal prolapse, combining VMR with anterior LSC/LSH appears to negatively impact patients’ satisfaction. Preoperative anal incontinence was demonstrated to be a risk factor for postoperative dissatisfaction.


Similar content being viewed by others
References
Kirby AC, Luber KM, Menefee SA. An update on the current and future demand for care of pelvic floor disorders in the United States. Am J Obstet Gynecol. 2013;209(6):584.e1–5. https://doi.org/10.1016/j.ajog.2013.09.011.
Scottish Government. Halt in use of transvaginal mesh. Published 12 September 2018. https://www.gov.scot/news/halt-in-use-of-transvaginal-mesh/.
Meriwether KV, Antosh DD, Olivera CK, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129–146.e2. https://doi.org/10.1016/j.ajog.2018.01.018.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014. https://doi.org/10.1002/14651858.CD004014.pub5.
Izett-Kay ML, Rahmanou P, Cartwright RJ, Price N, Jackson SR. Laparoscopic sacrohysteropexy versus vaginal hysterectomy and apical suspension: 7-year follow-up of a randomized controlled trial. Int Urogynecol J. 2022;33(7):1957–65. https://doi.org/10.1007/s00192-021-04932-6.
Lewis CM, Culligan P. Sacrohysteropexy followed by successful pregnancy and eventual reoperation for prolapse. Int Urogynecol J. 2012;23(7):957–9. https://doi.org/10.1007/s00192-011-1631-9.
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013;24(9):1481–7. https://doi.org/10.1007/s00192-012-2041-3.
Jha S, Cutner A, Moran P. The UK National Prolapse Survey: 10 years on. Int Urogynecol J. 2018;29(6):795–801. https://doi.org/10.1007/s00192-017-3476-3.
Rusavy Z, Najib B, Abdelkhalek Y, Grinstein E, Gluck O, Deval B. Outcomes of sacrocolpopexy/sacrohysteropexy with mesh placement targeted to affected compartment. Eur J Obstet Gynecol Reprod Biol. 2022;272:188–92. https://doi.org/10.1016/j.ejogrb.2022.03.037.
Maglinte DD, Kelvin FM, Fitzgerald K, Hale DS, Benson JT. Association of compartment defects in pelvic floor dysfunction. AJR Am J Roentgenol. 1999;172(2):439–44. https://doi.org/10.2214/ajr.172.2.9930799.
Smart NJ, Pathak S, Boorman P, Daniels IR. Synthetic or biological mesh use in laparoscopic ventral mesh rectopexy—a systematic review. Colorectal Dis. 2013;15(6):650–4. https://doi.org/10.1111/codi.12219.
Ahmad N, Stefan S, Adukia V, Naqvi S, Khan J. Laparoscopic ventral mesh rectopexy: functional outcomes after surgery. Surg J. 2018;4(4):e205–11. https://doi.org/10.1055/s-0038-1675358.
Stevenson ARL. What does the future hold for ventral rectopexy? EClinicalMedicine. 2019;16:2–3. https://doi.org/10.1016/j.eclinm.2019.10.010.
Ulrich D, Guzman Rojas R, Dietz HP, Mann K, Trutnovsky G. Use of a visual analog scale for evaluation of bother from pelvic organ prolapse. Ultrasound Obstet Gynecol. 2014;43(6):693–7. https://doi.org/10.1002/uog.13222.
Voutilainen A, Pitkäaho T, Kvist T, Vehviläinen-Julkunen K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72(4):946–57. https://doi.org/10.1111/jan.12875.
Rusavy Z, Grinstein E, Gluck O, Abdelkhalek Y, Deval B. Long-term development of surgical outcome of laparoscopic sacrohysteropexy with anterior and posterior mesh extension. Int Urogynecol J. 2023;34(1):191–200. https://doi.org/10.1007/s00192-022-05102-y.
Obut M, Oğlak SC, Akgöl S. Comparison of the quality of life and female sexual function following laparoscopic pectopexy and laparoscopic sacrohysteropexy in apical prolapse patients. Gynecol Minim Invasive Ther. 2021;10(2):96–103. https://doi.org/10.4103/GMIT.GMIT_67_20.
Srikrishna S, Robinson D, Cardozo L. Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–8. https://doi.org/10.1007/s00192-009-1069-5.
Lukacz ES, Lawrence JM, Burchette RJ, Luber KM, Nager CW, Galen BJ. The use of Visual Analog Scale in urogynecologic research: a psychometric evaluation. Am J Obstet Gynecol. 2004;191(1):165–70. https://doi.org/10.1016/j.ajog.2004.04.047.
Farghali MM, Abdelzaher A, Abdelazim IA. Surgical and quality of life outcomes after pelvic organ prolapse surgery in older postmenopausal women. Przeglad Menopauzalny Menopause Rev. 2021;20(1):21–8. https://doi.org/10.5114/pm.2021.104473.
Deval B, Jeffry L, Al Najjar F, Soriano D, Darai E. Determinants of patient dissatisfaction after a tension-free vaginal tape procedure for urinary incontinence. J Urol. 2002;167(5):2093–7.
Izett-Kay ML, Aldabeeb D, Kupelian AS, et al. Long-term mesh complications and reoperation after laparoscopic mesh sacrohysteropexy: a cross-sectional study. Int Urogynecol J. 2020;31(12):2595–602. https://doi.org/10.1007/s00192-020-04396-0.
Hunter JG, Spight DH, Sandone C, Fairman JE. Rectopexy and posterior mesh repair for rectal prolapse. In: Atlas of Minimally Invasive Surgical Operations. McGraw-Hill Education; 2018. Accessed 18 May 2023. accesssurgery.mhmedical.com/content.aspx?aid=1162531962.
Gluck O, Grinstein E, Deval B. Effect of age on surgical outcomes and rate of complication in women undergoing laparoscopic sacrocolpopexy and sacrohysteropexy. J Minim Invasive Gynecol. 2021;28(11):S101. https://doi.org/10.1016/j.jmig.2021.09.132.
Larsen MD, Lose G, Guldberg R, Gradel KO. Discrepancies between patient-reported outcome measures when assessing urinary incontinence or pelvic-prolapse surgery. Int Urogynecol J. 2016;27(4):537–43. https://doi.org/10.1007/s00192-015-2840-4.
Author information
Authors and Affiliations
Contributions
W.A.: data collection, manuscript writing; D.L.: data collection, manuscript writing; M.M.: statistical data processing; M.B.: manuscript review and editing; B.D.: project development, manuscript review and editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Handling Editor: Catherine Matthews
Editor in Chief: Maria Bortolini
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arab, W., Lukanović, D., Matjašič, M. et al. Determinants of Dissatisfaction After Laparoscopic Cure of Vaginal and/or Rectal Prolapse using Mesh: a Comprehensive Retrospective Cohort Study. Int Urogynecol J 35, 457–465 (2024). https://doi.org/10.1007/s00192-023-05701-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05701-3