Abstract
Introduction and hypothesis
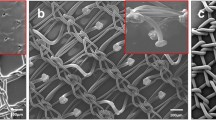
Polypropylene (PP) mesh shrinkage represents a serious complication, as a significant cause of pain and recurrence of pelvic organ prolapse or ventral hernias, frequently requiring several surgical interventions. The retraction seems to be caused by the host, in response to the implantation, through the occurrence of periprosthetic adhesions and fibrosis. We hypothesized that avoiding the postoperative adhesions can prevent PP mesh shrinkage.
Methods
Sixty rats were randomly assigned to three groups. A standardized hernia defect was induced on the abdominal wall, which was repaired using an extraperitoneal PP mesh alone (group 1), with application of a hyaluronate carboxymethylcellulose-based bioresorbable membrane (Seprafilm®, group 2), or an auto-cross-linked polysaccharide hyaluronan-based solution (Hyalobarrier® gel, group 3). Eight weeks after the procedure, a repeat laparotomy was performed. After scoring the adhesion and measuring the mesh surface, a microscopic study of the prosthesis-host tissue interfaces was performed.
Results
Group 1 displayed a median shrinkage of 29 % of the mesh. The Seprafilm® group (p = 0.0238) and Hyalobarrier® gel group (p = 0.0072) displayed a significantly smaller reduction of 19.12 and 17 %, respectively. Control group 1 displayed a significantly greater adhesion score (30.40) than the Seprafilm® (11.67, p = 0.0028) and Hyalobarrier® gel groups (11.19, p = 0.0013). The fibrosis was reduced in the Hyalobarrier® gel group only.
Conclusion
This experimental study revealed that Hyalobarrier® gel and Seprafilm® can prevent PP mesh shrinkage and postoperative adhesions. They might be integrated in a mesh size-saving strategy, which should preserve the quality and durability of the surgical repair and limit the postoperative pain.



Similar content being viewed by others
References
Amid PK (2001) Polypropylene prostheses. In: Bendavid R, Abrahamson J, Arregui ME, Flament JB, Phillips EH, Stoppa R, Read RC (eds) Abdominal wall hernias: principles and management. Springer, New York, pp 272–278
Amato G, Agrusa A, Romano G (2012) Fixation-free inguinal hernia repair using a dynamic self-retaining implant. Surg Technol Int 22:107–112
http://www.fda.gov/downloads/medicaldevices/safety/alertsandnotices/UCM262760.pdf. Accessed 21 Aug 2013
Lucot JP, Fritel X, Debodinance P, Bader G, Cosson M, Giraudet G, Collinet P et al (2013) PROSPERE randomized controlled trial: laparoscopic sacropexy versus vaginal mesh for cystocele POP repair. J Gynecol Obstet Biol Reprod (Paris) 42(4):334–341
de Tayrac R, Alves A, Thérin M (2007) Collagen-coated vs noncoated low-weight polypropylene meshes in a sheep model for vaginal surgery. A pilot study. Int Urogynecol J Pelvic Floor Dysfunct 18(5):513–520
Bellows CF, Alder A, Helton WS (2006) Abdominal wall reconstruction using biological tissue grafts: present status and future opportunities. Expert Rev Med Devices 3(35):657–675
Caquant F, Collinet P, Debodinance P, Berrocal J, Garbin O, Rosenthal C, Clave H, Villet R, Jacquetin B, Cosson M (2008) Safety of trans vaginal mesh procedure: retrospective study of 684 patients. J Obstet Gynaecol Res 34(4):449–456
Feiner B, Maher C (2010) Vaginal mesh contraction: definition, clinical presentation, and management. Obstet Gynecol 115(2 Pt1):325–330
Deprest J, Feola A (2013) The need for preclinical research on pelvic floor reconstruction. BJOG 120(2):141–143
Bako A, Dhar R (2009) Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct 20(1):103–111
Nohuz E, Darcha C, Moreno W, Tamburro S, Yanez M, Mulliez A, Grizard G, Mage G, Canis M (2009) Efficiency of TachoSil to prevent postsurgical adhesion development on laparoscopic rat model. Gynecol Surg 6(4):323–329
Diamond MP, Burns EL, Accomando B, Mian S, Holmdahl L (2012) Seprafilm® adhesion barrier: (1) a review of preclinical, animal, and human investigational studies. Gynecol Surg 9(3):237–245
Binda MM, Koninckx PR (2009) Prevention of adhesion formation in a laparoscopic mouse model should combine local treatment with peritoneal cavity conditioning. Hum Reprod 24(6):1473–1479
Diamond MP, Burns EL, Accomando B, Mian S, Holmdahl L (2012) Seprafilm® adhesion barrier: (2) a review of the clinical literature on intraabdominal use. Gynecol Surg 9(3):247–257
Renier D, Bellato P, Bellini D, Pavesio A, Pressato D, Borrione A (2005) Pharmacokinetic behaviour of ACP gel, an autocrosslinked hyaluronan derivative, after intraperitoneal administration. Biomaterials 26(26):5368–5374
Beksac MS, Salman MC, Dogan NU (2011) A new technique for surgical treatment of vaginal agenesis using combined abdominal-perineal approach. Case Rep Med 2011:120175. doi:10.1155/2011/120175
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12(1):63–69
Deffieux X, Letouzey V, Savary D, Sentilhes L, Agostini A, Mares P, Pierre F et al (2012) Prevention of complications related to the use of prosthetic meshes in prolapse surgery: guidelines for clinical practice. Eur J Obstet Gynecol Reprod Biol 165(2):170–180
Klinge U, Klosterhalfen B, Müller M, Ottinger AP, Schumpelick V (1998) Shrinking of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg 164(12):965–969
Celik A, Altinli E, Koksal N, Celik AS, Ozkan OF, Gumrukcu G (2009) The shrinking rates of different meshes placed intraperitoneally: a long-term comparison of the TiMesh, VYPRO II, Sepramesh, and DynaMesh. Surg Laparosc Endosc Percutan Tech 19(4):e130–e134
Yelimlieş B, Alponat A, Cubukçu A, Kuru M, Oz S, Erçin C, Gönüllü N (2003) Carboxymethylcellulose coated on visceral face of polypropylene mesh prevents adhesion without impairing wound healing in incisional hernia model in rats. Hernia 7(3):130–133
Garcia-Ureña MA, Vega Ruiz V, Díaz Godoy A, Báez Perera JM, Marin Gómez LM, Carnero Hernández FJ, Velasco García MA (2007) Differences in polypropylene shrinkage depending on mesh position in an experimental study. Am J Surg 193(4):538–542
van Geelen JM, Dwyer PL (2013) Where to for pelvic organ prolapse treatment after the FDA pronouncements? A systematic review of the recent literature. Int Urogynecol J 24(5):707–718
Miller D, Lucente V, Babin E, Beach P, Jones P, Robinson D (2011) Prospective clinical assessment of the transvaginal mesh technique for treatment of pelvic organ prolapse-5-year results. Female Pelvic Med Reconstr Surg 17(3):139–143
Jacquetin B, Hinoul P, Gauld J, Fatton B, Rosenthal C, Clavé H, Garbin O, Berrocal J, Villet R, Salet-Lizée D, Debodinance P, Cosson M (2013) Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 5-year prospective follow-up study. Int Urogynecol J 24(10):1679–1686
Lo TS, Pue LB, Tan YL, Wu PY (2013) Long-term outcomes of synthetic transobturator nonabsorbable anterior mesh versus anterior colporrhaphy in symptomatic, advanced pelvic organ prolapse surgery. Int Urogynecol J (in press)
http://www.gynerisq.fr/Accueil/SaisiedEPRCibl%C3%A9/tabid/85/Default.aspx. Accessed 21 Aug 2013
Rogowski A, Bienkowski P, Tosiak A, Jerzak M, Mierzejewski P, Baranowski W (2013) Mesh retraction correlates with vaginal pain and overactive bladder symptoms after anterior vaginal mesh repair. Int Urogynecol J 24(12):2087–2092
Dietz HP, Erdmann M, Shek KL (2011) Mesh contraction: myth or reality. Am J Obstet Gynecol 204(2):173.e1–173.e4
Svabík K, Martan A, Masata J, El-Haddad R, Hubka P, Pavlikova M (2011) Ultrasound appearances after mesh implantation—evidence of mesh contraction or folding? Int Urogynecol J 22(5):529–533
Acknowledgments
With great appreciation to our colleagues of the Statistical and Pathology Departments of the University Hospital of Clermont-Ferrand, to Dr. Bilal El Drayi and Mrs. Inga El Drayi for their cooperation in processing these results.
Conflicts of interest
Bernard Jacquetin holds the patent for TVM, for which he received royalties from Ethicon (the Prolift® has been withdrawn from the global market), and had a consultancy position with Ethicon.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nohuz, E., Alaboud, M., Darcha, C. et al. Effectiveness of Hyalobarrier and Seprafilm to prevent polypropylene mesh shrinkage: a macroscopic and histological experimental study. Int Urogynecol J 25, 1081–1087 (2014). https://doi.org/10.1007/s00192-014-2357-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2357-2