Abstract
Introduction and hypothesis
The aim was to evaluate the relationship between age and the impact of pelvic floor disorders (PFD) using a multi-dimensional pelvic floor questionnaire
Methods
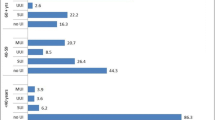
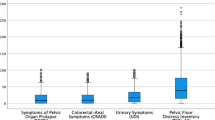
Questionnaire data on 4,311 women attending urogynaecology clinics with PFD were stratified by age into four groups: ≤35, 36–50, 51–65 and >65 years. The symptom frequency (ranging from 0 to 100) was divided in to mild (0–33), moderate (34–67), and severe (68–100) symptoms. Impact scores for equivalent levels of symptom frequency (mild, moderate and severe symptoms) were compared in women of different ages.
Results
Overall, bowel continence was associated with the greatest bother and constipation the least. Older women were significantly less bothered by mild to moderate urinary, bowel and vaginal symptoms (except IBS and vaginal capacity) than younger women. There was no difference in the impact of severe symptoms in different ages. In contrast, for sexual symptoms, there was a significant difference in the impact in older women for all grades of severity.
Conclusions
Women’s views and attitudes towards symptoms are variable and age is a significant factor. In women attending urogynaecology clinics with pelvic floor symptoms the impact of most symptoms (particularly sexual dysfunction) become less bothersome with age.

Similar content being viewed by others
References
Luber KM, Boero S, Choe JY (2001) The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol 184(7):1496–1501
Kepenekci I, Keskinkilic B, Akinsu F, Cakir P, Elhan AH, Erkek AB, Kuzu MA (2011) Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum 54(1):85–94
Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL (2006) Effect of patient age on increasing morbidity and mortality following urogynecological surgery. Am J Obstet Gynecol 194:1411–1417
Sung VW, Glasgow MA, Wohlrab KJ, Myers DL (2007) Impact of age on preoperative and postoperative urinary incontinence quality of life. Am J Obstet Gynecol 197:680.e1–680.e5
Sung VW, Joo K, Marques F, Myers DL (2009) Patient-reported outcomes after combined surgery for pelvic floor disorders in older compared to younger women. Am J Obstet Gynecol 201:534.e1–534.e5
Radley SC, Jones GL, Tanguy EA, Stevens VG, Nelson C, Mathers NJ (2006) Computer interviewing in urogynaecology, concept, development and psychometric testing of an electronic pelvic floor assessment questionnaire in primary and secondary care. BJOG 113:231–238
Jones GL, Radley SC, Lumb J, Farkas A (2009) Responsiveness of the electronic Personal Assessment Questionnaire – Pelvic Floor (ePAQ-PF). Int Urogynecol J Pelvic Floor Dysfunct 20:557–564
Jones GL, Radley SC, Lumb J, Jha S (2008) Electronic pelvic floor symptoms assessment: test of data quality of ePAQ-PF. Int Urogynecol J 19:1337–1347
Tennstedt SL, Fitzgerald MP, Nager CW et al (2006) Quality of life in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18:543–549
Pugsley H, Barbrook C, Mayne CJ et al (2005) Morbidity of incontinence surgery in women over 70 year old: a retrospective cohort study. BJOG 112:786–790
Freidman WH, Gallup DG, Burke JJ et al (2006) Outcomes of octogenarians and nonagenarians in elective major gynaecologic surgery. Am J Obstet Gynecol 195:547–553
Stepp KJ, Barber MD, Eun-Hee Y et al (2005) Incidence of perioperative complications of urogynecological surgery in elderly women. Am J Obstet Gynecol 192:1630–1636
Wang JY, Patterson TR, Hart SL, Varma MG (2008) Fecal incontinence: does age matter? Characteristics of older vs. younger women presenting for treatment of fecal incontinence. Dis Colon Rectum 51:426–431
Sinclair AJ, Ramsay IM (2011) The psychosocial impact of urinary incontinence in women. Obstet Gynaecol 13:143–148
Financial disclaimer
None.
Conflict of interest
Stephen Radley is a shareholder in EPAQ-PF Systems Ltd, an NHS spin-out technology company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dua, A., Radley, S., Jones, G. et al. The personal impact of pelvic floor symptoms and their relationship to age. Int Urogynecol J 25, 117–121 (2014). https://doi.org/10.1007/s00192-013-2167-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2167-y