Abstract
Purpose
Lateral meniscus posterior root tears (LMPRTs) are commonly found in patients with anterior cruciate ligament (ACL) injuries. However, risk factors for LMPRTs are not well known. This study was designed to systematically review the available evidence regarding risk factors associated with LMPRTs.
Methods
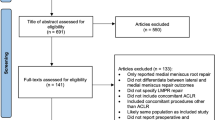
The PubMed, EMBASE, Cochrane Library, and Web of Science databases were searched for papers containing the key words “lateral meniscus posterior root tears”, “LMPRTs” and “risk factor”. Inclusion screening, data extraction, and quality assessment of the included articles were conducted independently by two authors. Statistical analysis was conducted to determine risk factors for LMPRTs.
Result
Seventeen studies with a total sample size of 6, 589 patients were identified. The pooled prevalence of LMPRTs was 9.6% (range, 5.1–33.8%) for ACL injury. Significant risk factors included a patient age of < 30 [OR = 1.4, 95% CI (1.07, 1.84), p = 0.01], male sex [OR = 1.50, 95% CI (1.24,1.81), p = 0.01], higher body mass index (BMI) [MD = 0.45, 95% CI (0.13, 0.76), p < 0.01], higher lateral posterior tibial slope (LPTS) [MD = 2.22, 95% CI (1.37, 3.07), p < 0.01], deep sulcus sign [OR = 5.76, 95% CI (1.35, 24.52), p < 0.01] and bone bruises on lateral femoral condyle [OR = 4.88, 95% CI (1.27, 18.77), p < 0.01], lateral meniscal extrusion > 1 mm [OR = 5.56, 95% CI (1.52, 20.29), p < 0.01] and > 3 mm [OR = 12.91 95% CI (1.28, 130.01), p < 0.01], medial meniscal tears [OR = 1.40, 95% CI (1.12, 1.75), p < 0.01], and medial ramp lesions [OR = 2.29, 95% CI (1.35, 3.89), p < 0.01].
Conclusion
Age below 30, male, higher BMI, higher LPTS, deep sulcus sign, bone bruises on lateral femoral condyle, lateral meniscal extrusion, medial meniscal tear, and medial ramp lesion are risk factors for LMPRTs.
Level of evidence
Level IV.









Similar content being viewed by others
References
Asai K, Nakase J, Oshima T, Shimozaki K, Toyooka K, Tsuchiya H (2020) Lateral meniscus posterior root tear in anterior cruciate ligament injury can be detected using MRI-specific signs in combination but not individually. Knee Surg Sports Traumatol Arthrosc 28:3094–3100
Bernholt D, DePhillipo NN, Aman ZS, Samuelsen BT, Kennedy MI, LaPrade RF (2021) Increased posterior tibial slope results in increased incidence of posterior lateral meniscal root tears in ACL reconstruction patients. Knee Surg Sports Traumatol Arthrosc 29:3883–3891
Bernholt DL, DePhillipo NN, Crawford MD, Aman ZS, Grantham WJ, LaPrade RF (2020) Incidence of displaced posterolateral tibial plateau and lateral femoral condyle impaction fractures in the setting of primary anterior cruciate ligament tear. Am J Sports Med 48:545–553
Berthold DP, Muench LN, Herbst E, Mayr F, Chadayammuri V, Imhoff AB, Feucht MJ (2021) High prevalence of a deep lateral femoral notch sign in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 29:1018–1024
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42:3016–3030
Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM (2013) A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med 41:1801–1807
Bordoni V, di Laura FG, Previtali D, Tamborini S, Candrian C, Cristallo Lacalamita M, Del Grande F, Filardo G (2019) Bone bruise and anterior cruciate ligament tears: presence, distribution pattern, and associated lesions in the pediatric population. Am J Sports Med 47:3181–3186
Brody JM, Lin HM, Hulstyn MJ, Tung GA (2006) Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 239:805–810
Choi CJ, Choi YJ, Lee JJ, Choi CH (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26:1602–1606
Feucht MJ, Bigdon S, Mehl J, Bode G, Müller-Lantzsch C, Südkamp NP, Niemeyer P (2015) Risk factors for posterior lateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 23:140–145
Feucht MJ, Salzmann GM, Bode G, Pestka JM, Kuhle J, Sudkamp NP, Niemeyer P (2015) Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 23:119–125
Gee SM, Tennent DJ, Cameron KL, Posner MA (2020) The burden of meniscus injury in young and physically active populations. Clin Sports Med 39:13–27
Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ, Jung KA (2012) Risk factors for medial meniscus posterior root tear. Am J Sports Med 40:1606–1610
Kamatsuki Y, Furumatsu T, Fujii M, Kodama Y, Miyazawa S, Hino T, Ozaki T (2018) Complete tear of the lateral meniscus posterior root is associated with meniscal extrusion in anterior cruciate ligament deficient knees. J Orthop Res 36:1894–1900
Kim SH, Seo JH, Kim DA, Lee JW, Kim KI, Lee SH (2022) Steep posterior lateral tibial slope, bone contusion on lateral compartments and combined medial collateral ligament injury are associated with the increased risk of lateral meniscal tear. Knee Surg Sports Traumatol Arthrosc 30:298–308
Koenig JH, Ranawat AS, Umans HR, Difelice GS (2009) Meniscal root tears: diagnosis and treatment. Arthroscopy 25:1025–1032
Kolbe R, Schmidt-Hebbel A, Forkel P, Pogorzelski J, Imhoff AB, Feucht MJ (2019) Steep lateral tibial slope and lateral-to-medial slope asymmetry are risk factors for concomitant posterolateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 27:2585–2591
Krych AJ, Hevesi M, Leland DP, Stuart MJ (2020) Meniscal root injuries. J Am Acad Orthop Surg 28:491–499
Kunze KN, Wright-Chisem J, Polce EM, DePhillipo NN, LaPrade RF, Chahla J (2021) Risk factors for ramp lesions of the medial meniscus: a systematic review and meta-analysis. Am J Sports Med 49:3749–3757
Li Y, He J, Hu Y (2020) Comparison of the efficiency and safety of total ankle replacement and ankle arthrodesis in the treatment of osteoarthritis: an updated systematic review and meta-analysis. Orthop Surg 12:372–377
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Magosch A, Mouton C, Nührenbörger C, Seil R (2020) Medial meniscus ramp and lateral meniscus posterior root lesions are present in more than a third of primary and revision ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 29:3059–3067
Minami T, Muneta T, Sekiya I, Watanabe T, Mochizuki T, Horie M, Katagiri H, Otabe K, Ohara T, Katakura M, Koga H (2018) Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc 26:1174–1181
Musahl V, Bedi A, Citak M, O’Loughlin P, Choi D, Pearle AD (2011) Effect of single-bundle and double-bundle anterior cruciate ligament reconstructions on pivot-shift kinematics in anterior cruciate ligament- and meniscus-deficient knees. Am J Sports Med 39:289–295
Nguyen JC, Baghdadi S, Lawrence JTR, Sze A, Guariento A, Ganley TJ, Johnson AM (2021) Lateral meniscus posterior root injury: MRI findings in children with anterior cruciate ligament tear. AJR Am J Roentgenol 217:984–994
Okoroha KR, Patel RB, Kadri O, Jildeh TR, Krause A, Gulledge C, Makhni EC, Moutzouros V (2019) Abnormal tibial alignment is a risk factor for lateral meniscus posterior root tears in patients with anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthrosc 27:590–595
Piggott T, Morgan RL, Cuello-Garcia CA, Santesso N, Mustafa RA, Meerpohl JJ, Schunemann HJ (2020) Grading of recommendations assessment, development, and evaluations (GRADE) notes: extremely serious, GRADE’s terminology for rating down by three levels. J Clin Epidemiol 120:116–120
Praz C, Vieira TD, Saithna A, Rosentiel N, Kandhari V, Nogueira H, Sonnery-Cottet B (2019) Risk factors for lateral meniscus posterior root tears in the anterior cruciate ligament-injured knee: an epidemiological analysis of 3956 patients from the SANTI study group. Am J Sports Med 47:598–605
Pula DA, Femia RE, Marzo JM, Bisson LJ (2014) Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury?: a case control study. Am J Sports Med 42:173–176
Shen JW, Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Prevalence of lateral meniscal extrusion for posterior lateral meniscal root lesion with and without concomitant midbody radial tear in anterior cruciate ligament injury. Arthroscopy 32:828–834
Shumborski SJ, Salmon LJ, Monk CI, Pinczewski LA (2021) Stable lateral meniscal posterior root tears left in situ at time of anterior cruciate ligament reconstruction are of minimal long-term clinical detriment. Arthroscopy 37:3500–3506
Song GY, Zhang H, Liu X, Zhang J, Xue Z, Qian Y, Feng H (2017) Complete posterolateral meniscal root tear is associated with high-grade pivot-shift phenomenon in noncontact anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 25:1030–1037
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Bone contusions after acute noncontact anterior cruciate ligament injury are associated with knee joint laxity, concomitant meniscal lesions, and anterolateral ligament abnormality. Arthroscopy 32:2331–2341
Wang YL, Yang T, Zeng C, Wei J, Xie DX, Yang YH, Long HZ, Xu B, Qian YX, Jiang SD, Lei GH (2017) Association Between tibial plateau slopes and anterior cruciate ligament injury: a meta-analysis. Arthroscopy 33:1248-1259.e4
Zheng T, Song GY, Feng H, Zhang H, Li Y, Li X, Zhang ZJ, Ni QK, Feng Z (2020) Lateral meniscus posterior root lesion influences anterior tibial subluxation of the lateral compartment in extension after anterior cruciate ligament injury. Am J Sports Med 48:838–846
Funding
This study was supported by Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (grant number CY2020-BJ03, CY2021-MS-B02), Gansu Natural Science Foundation Youth Project (20JR10RA712) and Natural Science Foundation of Gansu Province (21JR7RA393).
Author information
Authors and Affiliations
Contributions
WM and JJ conceived the project, the main conceptual ideas, and the proof sketch. LZC, DXW, and DYM extracted data and conducted the statistical analysis, WM and XYY wrote the manuscript, and WM, DXW, and DYM revised this manuscript. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that there is no conflict of interest.
Ethical approval
All data of this systematic review was extracted from the included articles that have been published previously. This systematic review does not contain any human participants or animal performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, M., Jiang, J., Liu, Z. et al. Age, male sex, higher posterior tibial slope, deep sulcus sign, bone bruises on the lateral femoral condyle, and concomitant medial meniscal tears are risk factors for lateral meniscal posterior root tears: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30, 4144–4155 (2022). https://doi.org/10.1007/s00167-022-06967-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06967-8