Abstract
Purpose
The aim of this study was to evaluate the clinical outcome at 5-year follow-up of a one-step procedure combining anterior cruciate ligament (ACL) reconstruction and partial meniscus replacement using a polyurethane scaffold for the treatment of symptomatic patients with previously failed ACL reconstruction and partial medial meniscectomy. Moreover, the implanted scaffolds have been evaluated by MRI protocol in terms of morphology, volume, and signal intensity.
Methods
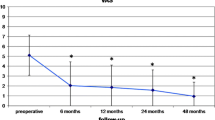
Twenty patients with symptomatic knee laxity after failed ACL reconstruction and partial medial meniscectomy underwent ACL revision combined with polyurethane-based meniscal scaffold implant. Clinical assessment at 2- and 5-year follow-ups included VAS, Tegner Activity Score, International Knee Documentation Committee (IKDC), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and the Lysholm Score. MRI evaluation of the scaffold was performed according to the Genovese scale with quantification of the scaffold’s volume at 1- and 5-year follow-ups.
Results
All scores revealed clinical improvement as compared with the preoperative values at the 2- and 5-year follow-ups. However, a slight, but significant reduction of scores was observed between 2 and 5 years. Concerning the MRI assessment, a significant reduction of the scaffold’s volume was observed between 1 and 5 years. Genovese Morphology classification at 5 years included two complete resorptions (Type 3) and all the remaining patients had irregular morphology (Type 2). With regard to the Genovese Signal at the 5-year follow-up, three were classified as markedly hyperintense (Type 1), 15 as slightly hyperintense (Type 2), and two as isointense (Type 1).
Conclusion
Simultaneous ACL reconstruction and partial meniscus replacement using a polyurethane scaffold provides favourable clinical outcomes in the treatment of symptomatic patients with previously failed ACL reconstruction and partial medial meniscectomy at 5 years. However, MRI evaluation suggests that integration of the scaffold is not consistent.
Level of evidence
Level IV.

Similar content being viewed by others
References
Barber FA (2018) Editorial commentary: polyurethane meniscal scaffold: a perfect fit or flop? Arthroscopy 34:1628–1630
Cengiz IF, Maia FR, da Silva Morais A, Silva-Correia J, Pereira H, Canadas RF et al (2020) Entrapped in cage (EiC) scaffolds of 3D-printed polycaprolactone and porous silk fibroin for meniscus tissue engineering. Biofabrication 12:025028
Cengiz IF, Pereira H, de Girolamo L, Cucchiarini M, Espregueira-Mendes J, Reis RL et al (2018) Orthopaedic regenerative tissue engineering en route to the holy grail: disequilibrium between the demand and the supply in the operating room. J Exp Orthop 5:1–14
Cengiz IF, Pereira H, Espregueira-Mendes J, Kwon IK, Reis RL, Oliveira JM (2019) Suturable regenerated silk fibroin scaffold reinforced with 3D-printed polycaprolactone mesh: biomechanical performance and subcutaneous implantation. J Mater Sci Mater Med 30:1–17
Cengiz IF, Pereira H, Espregueira-Mendes J, Oliveira JM, Reis RL (2017) Treatments of meniscus lesions of the knee: current concepts and future perspectives. Regen Eng Transl Med 3:32–50
Cengiz IF, Pereira H, Silva-Correia J, Ripoll PL, Espregueira-Mendes J, Kaz R et al (2017) Meniscal lesions: from basic science to clinical management in footballers. In: Espregueira-Mendes J, van Dijk CN, Neyret P, Cohen M, Della Villa S, Pereira H, Oliveira JM (eds) Injuries and health problems in football. Springer, New York, pp 145–163
Cengiz IF, Silva-Correia J, Pereira H, Espregueira-Mendes J, Oliveira JM, Reis RL (2017) Advanced regenerative strategies for human knee meniscus. In: Oliveira JM, Rui L (eds) ReisRegenerative strategies for the treatment of knee joint disabilities. Springer, New York, pp 271–285
Cengiz IF, Silva-Correia J, Pereira H, Espregueira-Mendes J, Oliveira JM, Reis RL (2017) Basics of the meniscus. In: Oliveira JM, Rui L (eds) Regenerative strategies for the treatment of knee joint disabilities. Springer, New York, pp 237–247
Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM (2011) Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 63(Suppl 11):S208-228
Dangelmajer S, Familiari F, Simonetta R, Kaymakoglu M, Huri G (2017) Meniscal transplants and scaffolds: a systematic review of the literature. Knee Surg Relat Res 29:3–10. https://doi.org/10.5792/ksrr.16.059
de Caro F, Perdisa F, Dhollander A, Verdonk R, Verdonk P (2020) Meniscus scaffolds for partial meniscus defects. Clin Sports Med 39:83–92
DeFranco MJ, Bach BR Jr (2009) A comprehensive review of partial anterior cruciate ligament tears. J Bone Jt Surg Am 91:198–208
Denti M, Lo Vetere D, Bait C, Schonhuber H, Melegati G, Volpi P (2008) Revision anterior cruciate ligament reconstruction: causes of failure, surgical technique, and clinical results. Am J Sports Med 36:1896–1902
Faivre B, Bouyarmane H, Lonjon G, Boisrenoult P, Pujol N, Beaufils P (2015) Actifit(R) scaffold implantation: Influence of preoperative meniscal extrusion on morphological and clinical outcomes. Orthop Traumatol Surg Res 101:703–708
Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M (2015) Meniscal scaffolds: results and indications. A systematic literature review. Int Orthop 39:35–46
Genovese E, Angeretti MG, Ronga M, Leonardi A, Novario R, Callegari L et al (2007) Follow-up of collagen meniscus implants by MRI. Radiol Med 112:1036–1048
Gorschewsky O, Klakow A, Putz A, Mahn H, Neumann W (2007) Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 15:1284–1292
Grassi A, Zicaro JP, Costa-Paz M, Samuelsson K, Wilson A, Zaffagnini S et al (2020) Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg Sports Traumatol Arthrosc 28:418–431
Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE et al (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8:141–150
Haefeli M, Elfering A (2006) Pain assessment. Eur Spine J 15(Suppl 1):S17-24
Houck DA, Kraeutler MJ, Belk JW, McCarty EC, Bravman JT (2018) Similar clinical outcomes following collagen or polyurethane meniscal scaffold implantation: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:2259–2269
Leroy A, Beaufils P, Faivre B, Steltzlen C, Boisrenoult P, Pujol N (2017) Actifit(R) polyurethane meniscal scaffold: MRI and functional outcomes after a minimum follow-up of 5 years. Orthop Traumatol Surg Res 103:609–614
Menetrey J, Duthon VB, Laumonier T, Fritschy D (2008) “Biological failure” of the anterior cruciate ligament graft. Knee Surg Sports Traumatol Arthrosc 16:224–231
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 2011:CD005960
Monllau JC, Poggioli F, Erquicia J, Ramirez E, Pelfort X, Gelber P et al (2018) Magnetic resonance imaging and functional outcomes after a polyurethane meniscal scaffold implantation: minimum 5-year follow-up. Arthroscopy 34:1621–1627
Pereira H, Cengiz I, Silva-Correia J, Oliveira J, Reis R, Espregueira-Mendes J (2015) Human meniscus: from biology to tissue engineering strategies. Sports injuries. Springer, Berlin, pp 1089–1102
Pereira H, Cengiz IF, Gomes S, Espregueira-Mendes J, Ripoll PL, Monllau JC et al (2019) Meniscal allograft transplants and new scaffolding techniques. EFORT Open Rev 4:279–295
Pereira H, Cengiz IF, Silva-Correia J, Cucciarini M, Gelber PE, Espregueira-Mendes J et al (2016) Histology-ultrastructure-biology. In: Hulet C, Pereira H, Peretti G, Denti M (eds) Surgery of the meniscus. Springer, New York, pp 23–33
Pereira H, Cengiz IF, Silva-Correia J, Ripoll PL, Varatojo R, Oliveira JM, Reis RL, Espregueira-Mendes J (2016) In: Randelli P, van Dejour D, Dijk C, Denti M, Seil R (eds) Meniscal Repair: Indications, Techniques, and Outcome. Arthroscopy. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-49376-2_11
Pereira H, Frias AM, Oliveira JM, Espregueira-Mendes J, Reis RL (2011) Tissue engineering and regenerative medicine strategies in meniscus lesions. Arthroscopy 27:1706–1719
Prodromos C, Fu G, Gobbi H et al (2008) The economics of anterior cruciate ligament reconstruction. The anterior cruciate ligament: reconstruction and basic science. Saunders Elsevier, Philadelphia, pp 79–83
Reale D, Previtali D, Andriolo L, Grassi A, Candrian C, Zaffagnini S et al (2022) No differences in clinical outcome between CMI and Actifit meniscal scaffolds: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30:328–348. https://doi.org/10.1007/s00167-021-06548-1
Samuelsson K, Andersson D, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 25:1139–1174
Siddiq F, Bains NK, Herbert JP, Akhtar IN, Thomas AJ, Kan P et al (2021) Reliability of an automated computerized hematoma volumetric analysis protocol in patients with chronic subdural hemorrhage. World Neurosurg 150:e372–e377
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Thomas NP, Pandit HG (2008) Revision anterior cruciate ligament. In: Prodromos B, Fu FH, Georgoulis AD, Gobbi A, Howell SM et al (eds) The anterior cruciate ligament: reconstruction and basic science. Saunders Elsevier, Philadelphia, pp 443–457
Verdonk R (2011) The meniscus: past, present and future. Knee Surg Sports Traumatol Arthrosc 19:145–146
Verhaeghe L, Boeren K (2018) A rare complication after synthetic meniscus replacement. J Belg Soc Radiol 102:63
Vrancken AC, Buma P, van Tienen TG (2013) Synthetic meniscus replacement: a review. Int Orthop 37:291–299
Zhong M, Lu W, Zhu W (2020) Comment on medial meniscus scaffold implantation in combination with concentrated bone marrow aspirate injection: minimum 3-year follow-up. J Knee Surg. https://doi.org/10.1055/s-0040-1721037
Acknowledgements
IFC thanks the TERM RES-Hub, Tissue Engineering and Regenerative Medicine Infrastructure project, funded by the Portuguese Foundation for Science and Technology (FCT), and the funding through the project 2IQBIONEURO (ref. 0624_2IQBIONEURO_6_E). The FCT distinctions attributed to IFC under the Estímulo ao Emprego Científico program (2021.01969.CEECIND), and to JS-C under the Investigator FCT program (IF/00115/2015) are also greatly acknowledged.
Funding
The TERM RES-Hub, Tissue Engineering and Regenerative Medicine Infrastructure project, funded by the Portuguese Foundation for Science and Technology (FCT), the project 2IQBIONEURO (ref. 0624_2IQBIONEURO_6_E), and the Estímulo ao Emprego Científico program of FCT (2021.01969.CEECIND).
Author information
Authors and Affiliations
Contributions
HP: conceptualization and methodology, and manuscript writing and review; IFC: manuscript writing and review; JS-C: manuscript writing and review; JMO: manuscript writing and review, and funding acquisition; JCV: manuscript writing and review; SG: manuscript writing and review; PLR: manuscript writing and review RLR: manuscript review, and funding acquisition; JE-M: manuscript review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study received approval from the local Ethical Committee.
Informed consent
Patients gave their informed written consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pereira, H., Cengiz, I.F., Silva-Correia, J. et al. Integration of polyurethane meniscus scaffold during ACL revision is not reliable at 5 years despite favourable clinical outcome. Knee Surg Sports Traumatol Arthrosc 30, 3422–3427 (2022). https://doi.org/10.1007/s00167-022-06946-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06946-z