Abstract
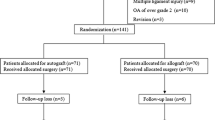
Although many different interventions have been proposed for treating cartilage lesions at the time of ACL reconstruction, the normal healing response of these injuries has not been well documented. To address this point, we compared the arthroscopic status of chondral lesions at the time of ACL reconstruction with that obtained at second-look arthroscopy. We hypothesized that there might be a location-specific difference in the healing response of damaged articular cartilage. Between September 1998 and March 2000, 383 patients underwent arthroscopically-assisted hamstring ACL reconstruction without any intervention to the articular cartilage. Among these patients, 84 patients underwent second-look arthroscopy (ranging from 6 to 52 months following initial surgery) and make up the population of the present study. Chondral injuries, left untreated at ACL reconstruction, were arthroscopically evaluated using the Outerbridge classification, and were again evaluated at second-look arthroscopy. At second-look arthroscopy, there was significant recovery of chondral lesions by Outerbridge grading on both the medial and lateral femoral condyles. Among the recovered chondral lesions, 69% of cases of the medial femoral condyle, 88% of cases of the lateral femoral condyle were partial thickness injuries (grade I and II). Conversely, there was no significant recovery of chondral lesions observed at the patello-femoral joint or tibial plateaus. Our study revealed that there was a location-specific difference in the natural healing response of chondral injury. Untreated cartilage lesions on the femoral condlyes had a superior healing response compared to those on the tibial plateaus, and in the patello-femoral joint.




Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Buckwalter JA, Mankin HJ (1997) Articular cartilage: part II: degeneration and osteoarthritis, repair, regeneration, and transplantation. J Bone Joint Surg Am 79:612–632
Newman AP (1998) Articular cartilage repair. Am J Sports Med 26:309–324
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthr Cartil 10:432–463
Landells JW (1957) The reactions of injured human articular cartilage. J Bone Joint Surg Br 39:548–562
DePalma AF, McKeever CD, Subin DK (1966) Process of repair of articular cartilage demonstrated by histology and autoradiography with tritiated thymidine. Clin Orthop 48:229–242
Fuller JA, Ghadially FN (1972) Ultrastructural observations on surgically produced partial-thickness defects in articular cartilage. Clin Orthop 86:193–205
Ghadially FN, Thomas I, Oryschak AF, Lalonde JM (1977) Long-term results of superficial defects in articular cartilage: a scanning electron-microscope study. J Pathol 121:213–217
Hunziker EB, Rosenberg LC (1996) Repair of partial-thickness defects in articular cartilage: cell recruitment from the synovial membrane. J Bone Joint Surg Am 78:721–733
Noyes FR, Bassett RW, Grood ES, Butler DL (1980) Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am 62:687–695
Indelicato PA, Bittar ES (1985) A perspective of lesions associated with ACL insufficiency of the knee. A review of 100 cases. Clin Orthop Relat Res 198:77–80
Hirshman HP, Daniel DM, Miyasaka K (1990) The fate of unoperated knee ligament injuries. In: Daniel DM, Akeson WH, O’Connor JJ (eds) Knee ligaments: structure, function, injury and repair. Raven Press, New York, pp 481–503
DeHaven KE (1980) Diagnosis of acute knee injuries with haemarthrosis. Am J Sports Med 8:9–14
Fowler PJ, Messieh SS (1987) Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med 15:553–557
Alfredson H, Thorsen K, Lorentzon R (1999) Treatment of tear of the anterior cruciate ligament combined with localised deep cartilage defects in the knee with ligament reconstruction and autologous periosteum transplantation. Knee Surg Sports Traumatol Arthrosc 7:69–74
Bobic V (1996) Arthroscopic osteochondral autograft transplantation in anterior cruciate ligament reconstruction: a preliminary clinical study. Knee Surg Sports Traumatol Arthrosc 3:262–264
Klinger HM, Baums MH, Otte S, Steckel H (2003) Anterior cruciate reconstruction combined with autologous osteochondral transplantation. Knee Surg Sports Traumatol Arthrosc 11:366–371
Peterson L, Minas T, Brittberg M, Nilsson A, Sjogren-Jansson E, Lindahl A (2000) Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res 374:212–234
Amin AA, Bartlett W, Gooding CR, Sood M, Skinner JA, Carrington RW, Briggs TW, Bentley G (2006) The use of autologous chondrocyte implantation following and combined with anterior cruciate ligament reconstruction. Int Orthop 30:48–53
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85(Suppl 2):25–32
Toritsuka Y, Shino K, Horibe S, Mitsuoka T, Hamada M, Nakata K, Nakamura N, Yoshikawa H (2004) Second-look arthroscopy of anterior cruciate ligament grafts with multistranded hamstring tendons. Arthroscopy 20:287–293
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43:752–757
Wozney JM, Rosen V, Byrne M, Celeste AJ, Moutsatsos I, Wang EA (1990) Growth factors influencing bone development. J Cell Sci Suppl 13:149–156
Eppley BL, Woodell JE, Higgins J (2004) Platelet quantification and growth factor analysis from platelet-rich plasma: implications for wound healing. Plast Reconstr Surg 114:1502–1508
Prockop DJ (1997) Marrow stromal cells as stem cells for nonhematopoietic tissues. Science 276:71–74
De Bari C, Dell’Accio F, Tylzanowski P, Luyten FP (2001) Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum 44:1928–1942
Wickham MQ, Erickson GR, Gimble JM, Vail TP, Guilak F (2003) Multipotent stromal cells derived from the infrapatellar fat pad of the knee. Clin Orthop 412:196–212
Roufosse CA, Direkze NC, Otto WR, Wright NA (2004) Circulating mesenchymal stem cells. Int J Biochem Cell Biol 36:585–597
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Arnoczky SP, Rubin RM, Marshall JL (1979) Microvasculature of the cruciate ligaments and its response to injury. An experimental study in dogs. J Bone Joint Surg Am 61:1221–1229
Maekawa K, Furukawa H, Kanazawa Y, Hijioka A, Suzuki K, Fujimoto S (1996) Electron and immunoelectron microscopy on healing process of the rat anterior cruciate ligament after partial transection: the roles of multipotent fibroblasts in the synovial tissue. Histol Histopathol 11:607–619
Murray MM, Martin SD, Martin TL, Spector M (2000) Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am 82:1387–1397
Arnoczky SP, Warren RF, Spivak JM (1988) Meniscal repair using an exogenous fibrin clot. An experimental study in dogs. J Bone Joint Surg Am 70:1209–1217
Kimura M, Shirakura K, Hasegawa A, Kobuna Y, Niijima M (1995) Second look arthroscopy after meniscal repair. Factors affecting the healing rate. Clin Orthop Relat Res 314:185–191
Miyamoto A, Deie M, Yamasaki T, Nakamae A, Shinomiya R, Adachi N, Ochi M (2007) The role of the synovium in repairing cartilage defects. Knee Surg Sports Traumatol Arthrosc 15:1083–1093
Cameron ML, Briggs KK, Steadman JR (2003) Reproducibility and reliability of the Outerbridge classification for grading chondral lesions of the knee arthroscopically. Am J Sports Med 31:83–86
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakamura, N., Horibe, S., Toritsuka, Y. et al. The location-specific healing response of damaged articular cartilage after ACL reconstruction: short-term follow-up. Knee Surg Sports Traumatol Arthr 16, 843–848 (2008). https://doi.org/10.1007/s00167-008-0565-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0565-3