Abstract
Purpose
Acute illness severity predicts mortality in intensive care unit (ICU) patients, however, its predictive value decreases over time in ICU. Typically after 10 days, pre-ICU (antecedent) characteristics become more predictive of mortality, defining the onset of persistent critical illness (PerCI). How patient frailty affects development and death from PerCI is unknown.
Methods
We conducted a secondary analysis of data from a prospective binational cohort study including 269,785 critically ill adults from 168 ICUs in Australia and New Zealand, investigating whether frailty measured with the Clinical Frailty Scale (CFS) changes the timing of onset and risk of developing PerCI and of subsequent in-hospital mortality. We assessed associations between frailty (CFS ≥ 5) and mortality prediction using logistic regression and area under the receiver operating characteristics (AUROC) curves.
Results
2190 of 50,814 (4.3%) patients with frailty (CFS ≥ 5) versus 6624 of 218,971 (3%) patients without frailty (CFS ≤ 4) developed PerCI (P < 0.001). Among patients with PerCI, 669 of 2190 (30.5%) with frailty and 1194 of 6624 without frailty (18%) died in hospital (P < 0.001). The time point defining PerCI onset did not vary with frailty degree; however, with increasing length of ICU stay, inclusion of frailty progressively improved mortality discrimination (0.1% AUROC improvement on ICU day one versus 3.6% on ICU day 17).
Conclusion
Compared to patients without frailty, those with frailty have a higher chance of developing and dying from PerCI. Moreover the importance of frailty as a predictor of mortality increases with ICU length of stay. Future work should explore incorporation of frailty in prognostic models, particularly for long-staying patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This population-based study of 269,785 critically ill patients in Australia and New Zealand demonstrates that frailty significantly increases the risk of developing persistent critical illness. Incorporation of frailty status into mortality prediction models also better discriminates survivors from non-survivors, with frailty better able to predict death the longer patients stay in the ICU. |
Introduction
Acute illness severity at admission in intensive care unit (ICU) predicts mortality in critical illness. Its predictive strength, however, decreases the longer a patient stays in the ICU. Concurrently, the relative importance of pre-admission patient characteristics in determining death in ICU increases. The point at which acute illness severity is no longer more predictive of mortality than antecedent (pre-ICU) patient characteristics defines the onset of a condition known as persistent critical illness (PerCI). In a study of over a million ICU patients, this transition point occurred 10 days after ICU admission [1]. Moreover, the importance of this syndrome is highlighted by observations that patients with PerCI have a mortality rate of 25–30% [2], use one-quarter of all ICU bed-days, have high rates of discharge to permanent chronic care facilities, and generate extremely high healthcare costs—more than $20 billion annually in the US alone [3, 4]. The magnitude of the healthcare impact and negative patient outcomes associated with PerCI have now been confirmed and characterized in various populations worldwide [5,6,7]. However, the relationship between pre-ICU frailty and PerCI is unknown. This is an important knowledge gap, because frailty is present in around 30% of patients admitted to ICU, and is itself associated with longer ICU stay and adverse outcomes [8, 9].
Accordingly, we performed a population-based study of patients admitted to ICUs in Australia and New Zealand (ANZ), to investigate the interplay between frailty and PerCI. Our primary aim was to test the hypothesis that frailty increases the risk of developing PerCI and subsequently dying in hospital. Our secondary aims were to investigate whether the degree of frailty affected the transition point between acute illness and antecedent components in mortality prediction, resource use associated with PerCI, and whether including frailty in predictive models could improve their ability to discriminate PerCI survivors from non-survivors at different time points during an ICU admission.
Methods
We conducted a population-level, observational, retrospective study using prospectively gathered data from patients admitted to 168 ICUs in ANZ between January 2017 and September 2020 contained in the ANZ Intensive Care Society Adult Patient Database (ANZICS APD). Patients aged > 16 years at time of ICU admission were included. We excluded patients admitted solely for organ donation or palliative care, those transferred between ICUs (with uncertain duration of total ICU exposure), or those re-admitted to ICU during the index hospitalisation.
Clinical data collectors measured frailty on ICU admission using the Canadian Study of Health and Aging Clinical Frailty Scale (CFS) [10]. The CFS is a judgement-based categorical scale based on patients’ baseline fitness, which correlates well with the original 70-item frailty index used in this original study. It is also valid and reliable when applied to a range of acutely ill populations, and is the dominant frailty scale used in ICUs worldwide [8, 11,12,13]. The CFS is modified in the ANZICS-APD to eight categories: CFS = 1 (very fit), CFS = 2 (well), CFS = 3 (managing well), CFS = 4 (vulnerable), CFS = 5 (mildly frail), CFS = 6 (moderately frail), CFS = 7 (severely frail), or CFS = 8 (very severely frail). Terminally ill patients, usually scored 9 on the CFS, are instead scored in the APD on their level of frailty. The CFS was analysed in four categories (CFS 1–2, 3–4, 5–6, 7–8), and also dichotomised (frail: CFS = 5–8, non-frail: CFS = 1–4). The study was approved by the Alfred Hospital Human Research Ethics Committee, individual patient consent was not required (HREC-ref. 584/18). During the study period of interest (January 2017–September 2020), 196 ICUs from Australia and New Zealand contributed data to the APD representing more than 90% of all ICU admissions during this period. A total of 86% (168/196) of these sites contributed patient information pertaining to frailty.
Statistical analysis
The primary outcome was in-hospital mortality during index hospitalization. Exposure variables were frailty, calculated using the CFS, and risk of death predictions calculated separately using antecedent characteristics or acute illness components as previously described [1]. The antecedent characteristics included features related to the patient (age, smoking status, comorbidities, treatment limitations), the admitting ICU (location, size, type) and temporal trends relating to the timing of admission (hour, day, month, and year).
The acute illness prediction model included features collected in the 24 h following ICU admission and include Acute Physiology and Chronic Health Evaluation (APACHE) admission diagnosis; APACHE III acute physiology scores; ICU admission source (emergency department, operating theatre, ward); ICU care type (ICU vs high-dependency unit); pre-ICU length of hospital stay; mechanical ventilation; medical emergency team call, respiratory arrest, or cardiac arrest in the previous 24 h. Models were calculated using parameter estimates outlined above derived from 514,117 patients included in the 2000–2014 cohort in which PerCI was first described [1]. Primary multivariable analyses for in-hospital mortality were conducted using logistic regression, individually analyzing patients still in ICU with separate regression models conducted each day between day 1 (the day of ICU admission) and day 21. To enable prediction models to be constructed using all available data, where data was missing for categorical variables, an additional category was created and fitted to account for missingness. Where continuous physiological variables were missing, single imputation with normal value substitution was conducted in accordance with standard clinical risk modelling [14]. No imputation was performed for the primary exposure variable (frailty).
The contribution of acute and antecedent characteristics to in-hospital mortality risk prediction were examined via differences in the area under the receiver operating characteristics (AUROC) curve for each regression, with statistical comparison performed using chi-square tests. To establish the increased risk of death associated with frailty, patients from the highest frailty category (CFS 7–8) were compared against patients from the lowest frailty category (CFS 1–2), adjusting for both acute and antecedent characteristics, with results presented as odds ratios (95% CI). Two additional sets of models were further constructed to determine the independent discriminatory capacity of frailty to predict in-hospital mortality. These models include the following: (a) incorporating the antecedent risk of death prediction, the acute illness risk of death prediction, and an interaction term between the two, and (b) the same model with the addition of frailty status, and interaction terms between frailty and the existing model variables as defined in (a). To further model the effect of frailty-data missingness, a sensitivity analysis was conducted on a subset of ICUs that had high completion (> 80%) of frailty data for the entire study period.
Multivariable analysis for the prediction of PerCI (a priori defined as an intensive care stay in excess of 10 days) was performed using logistic regression adjusting for characteristics that have been previously identified as being associated with PerCI [1]. Variables included in the model pertain to the ICU (location, type and size), time (hour, day and year), patient (frailty, age, gender and comorbidities), ICU admission (care type, source, treatment limitations and Pre-ICU length of stay) and patient severity (admission diagnosis and physiological derangement). Results are presented as odds ratios (95% CI). Raw comparison of proportions were compared using chi-square tests for equal proportion.
All analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and to increase the robustness of our analysis a two sided P value of 0.001 was used to indicate statistical significance.
Results
Patient characteristics
Of 522,788 eligible patients, 269,785 patients with complete frailty scores were available for analysis (Fig. 1). Patients diagnosed with frailty (CFS ≥ 5) were older than patients without frailty (CFS ≤ 4), (mean [SD] age 72.5 [14.2] vs. 60.4 [17.6] years), with higher illness severity scores (mean [SD] APACHE III-j score 61 [23] vs. 45 [21]), more likely to be female, and to be admitted with medical (e.g. sepsis) vs surgical (e.g. trauma/cardiac surgical) diagnoses. These associations were more pronounced with increasing frailty degree (Table 1).
Frailty and persistent critical illness
A total of 4.3% (2190 of 50,814) patients with frailty and 3% (6624 of 218,971) patients without frailty developed PerCI (P < 0.001). The risk of developing PerCI was greater with increasing frailty degree; 4.8% of patients with CFS 7–8 vs. 2.8% of patients with CFS 1–2 developing PerCI (Table 1). Each one unit increase in CFS was associated with an adjusted odds ratio (95% CI) for development of PerCI of 1.08 (1.06–1.1), P < 0.001 (Supplementary Table 6).
Frailty and mortality in patients with persistent critical illness
Among patients with PerCI, 30.5% (669 of 2190) patients with frailty vs. 18% (1194 of 6624) patients without frailty died in hospital (P < 0.001). When stratified by frailty degree and at all time-points over the ICU course, patients with persistent critical illness who were in the highest frailty categories had significantly greater in-hospital mortality than those in lower frailty categories (Fig. 2). The greater mortality rate associated with advanced frailty (CFS 7–8) increased disproportionately over time compared to lower degrees of frailty. Thus, the case fatality rate was 33% (304 of 905) for CFS 7–8 patients compared with 11% (433 of 3786) for CFS 1–2 patients who were still in ICU on day seven and 39% (36 of 92) CFS 7–8 patients vs 14% (88 of 624) of CFS 1–2 patients who were still in ICU on day 21 (Fig. 2). When compared with CFS 1–2 patients, those with CFS 7–8 had between a two and four-fold greater odds of death on any given day in ICU, a risk which increased from day five onwards (Supplementary Fig. 1).
Adjusted hospital mortality, stratified by Clinical Frailty Status. Probability of death is derived from logistic regression including both the acute and post-ICU risk scores. Error bars are SEs. The shaded area relates to the onset of persistent critical illness. The numbers under the x-axis refer to all patients in the ICU at risk on any day, stratified by frailty degree
The impact of frailty on resource utilisation with persistent critical illness
A total of 3.3% (8814 of 269,785) of patients admitted to ICU developed PerCI; these patients used 23.3% (165,496 of 709,544) of all ICU bed-days and 9.9% (341,173 of 3,449,273) of all hospital bed-days. A total of 0.8% of patients admitted to ICU were patients with frailty who developed PerCI. This cohort accounted for 5.6% of all ICU bed-days and 2.4% of all hospital bed-days.
The impact of frailty on mortality prediction
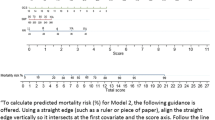
After 10 days in the ICU, illness severity was no longer more predictive of mortality than antecedent patient characteristics (Supplementary Fig. 2). This transition point, which defines the onset of PerCI, varied little by the degree of frailty (Fig. 3). When comparing the AUROC, the addition of frailty as a continuous variable to predictive models had minimal impact on discriminatory power for mortality over the first five days in ICU, but progressively improved discrimination over the subsequent two weeks for all patients (0.1% improvement on ICU day one vs. 3.6% improvement on day 17, P < 0.001) (Fig. 4, Supplementary Table 5).
Area under the curve for mortality prediction over time for models (blue line) incorporating antecedent and acute illness factors (“full model”) and (orange line) incorporating frailty, antecedent and acute illness factors (“full model + frailty”). Curves demonstrate increasing discrimination for mortality with the addition of frailty beyond ICU admission day five. Error bars are SEs
Sensitivity analysis
When considering patients with complete vs. missing frailty scores, those with complete vs. missing frailty data were older (mean [SD] age 62.7 [17.7] vs. 61.9 [17.6] years), with higher illness severity scores (mean [SD] APACHE III-j score 50 [24] vs. 48 [23]) and lower in-hospital mortality (6.1% vs. 7.1%), although the magnitude of these differences was small (Supplementary Table 1). Sensitivity analyses including only the 76 ICUs that had > 80% complete frailty data were consistent in demonstrating that the magnitude of importance of antecedent factors in mortality determination was higher for patients in the CFS 7–8 category (Supplementary Fig. 3).
Discussion
Key findings
In this retrospective study of over quarter of a million patients in 168 ICUs, frailty was associated with increased risk of developing and dying from persistent critical illness. Patients in the highest frailty categories had almost twice the risk of PerCI compared to patients with lower degrees of frailty, exceeding a threefold increased risk of death after ICU day 10. Incorporation of frailty with pre- and post-ICU patient factors also improved mortality discrimination over time in the ICU; however, frailty degree did not materially affect the time of transition to PerCI, which still occurred at the 10th post-ICU admission day.
Relationship to prior literature
In the study by Iwashyna and colleagues, the hospital case fatality rate was initially very high on admission, then reduced over time in the ICU for patients with a high (> 66%) and moderate (33–66%) risk of death on admission [1]. In contrast, we observed that in patients with higher frailty categories (associated with higher predicted risk of death on admission) the risk of dying progressively increased the longer the patient stayed in the ICU. This suggests that frailty is an important negative prognostic modifier of outcome over time in the ICU. The importance of including frailty in dynamic risk prediction over time has been observed in other hospitalised populations [15], however, it has not previously been studied in the ICU context.
We found that the time of transition to PerCI (day 10) in our study was similar to a study of 17,000 patients from Alberta, Canada (day nine) [7], and the same as the previous study by Iwashyna and colleagues examining a historical cohort of more than a million patients [1]. The finding that this transition point has not changed in a more contemporary ICU population from the same region lends further construct validity to this concept, and its use to define PerCI.
Small single-centre studies have previously demonstrated nosocomial factors associated with progression to PerCI such as new sepsis, delirium and pneumonia during early ICU admission [16,17,18]. However, no previous studies have been able to identify patient factors present prior to ICU admission that are consistently associated with its development- neither age, comorbidities, nor illness severity on admission [6, 19]. This study, then, is the first to identify that frailty not only increases the risk of progression to PerCI, but also of death, in those who develop PerCI.
We have previously shown that the addition of frailty degree improves the discrimination for mortality of the APACHE III score at ICU admission [8]; however, this is the first study to demonstrate the improvement in mortality discrimination over time in PerCI patients. This improvement increased with time in ICU, from a 1% increase in the AUROC at day seven to 3% at admission day 20, although predictive ability overall remained modest. This reinforces the notion that frailty measurement on admission to the ICU is especially relevant at the population level for that cohort who go on to develop PerCI.
Implications of study findings
Our findings suggest that patients with frailty are at greater risk of developing persistent critical illness, with substantial resource utilisation. Moreover, they imply if the proportion of patients with frailty admitted to ICU rises, demand for ICU beds to care for patients with PerCI will also rise disproportionately. In addition, these findings imply that although patients in the highest frailty categories have a much greater risk of developing PerCI, that frailty does not alter the transition point of its occurrence. Finally, they demonstrate that frailty is associated with an increasing mortality from the fifth ICU admission day onward, and that incorporation of frailty with pre- and post-ICU patient factors progressively improves mortality discrimination after ICU day five. Future research should seek to develop risk-prediction models for the development of PerCI, incorporating baseline frailty status, and also aim to operationalise tools that can be re-applied during prolonged ICU admissions for more dynamic risk prediction.
Strengths and limitations
Our study has several strengths. We used a validated approach to the diagnosis of persistent critical illness now confirmed in many populations and settings worldwide. We included over a quarter of a million patients in 168 ICUs from two countries, thus comprising one of the largest studies examining PerCI and frailty worldwide. Our study population, admitted within the last 5 years, was also reflective of modern ICU practice in our region.
We acknowledge several limitations. Missing frailty data affected almost half of the eligible patient cohort over the study period, however, baseline demographic and outcome data between missing and included cohorts were similar, and our findings remained consistent in sensitivity analyses including only the 76 ICUs with low levels of frailty missingness. We only incorporated severity of illness on ICU admission, and did not recalculate it on subsequent ICU admission days. This approach, however, is consistent with previous studies of the concept of persistent critical illness, and is perhaps more clinically relevant to the question of ICU triage for high-risk patients, particularly those with advanced frailty. It is uncertain to what degree our results apply to jurisdictions with greater access to long-term acute care hospitals (not a major component of post-ICU discharge in our region). We were unable to measure to what degree subsequent withdrawal of active organ supports or treatment limitation contributed to the higher mortality observed with increased frailty over time in the ICU. We note, however, that overall ICU and hospital length of stay was almost twice as long for patients in the highest vs. lowest frailty categories, thus curtailing of active ICU management is unlikely to have preferentially affected those patients with advanced frailty. We were also unable to assess to what degree frailty status on triage to ICU may have affected our modelling (as our database includes only ICU-admitted patients), nor were we able to follow patients after hospital discharge. Thus, it is unclear whether frailty affects longer term outcomes after PerCI. It is noteworthy, however, that prior studies have demonstrated particularly poor long-term survival after PerCI (25–50% of initial survivors dead at 1-year), with mortality increasing with age [20, 21]. As the prevalence of frailty is considerably greater in older critically ill patients, it is also likely to be an important factor contributing to the disproportionately poor long-term outcomes for older survivors of PerCI. Further research is thus required to examine the interplay between age, frailty and other factors in determining the long-term outcomes of older survivors of PerCI [22].
Conclusion
Frailty affects the development and outcomes of PerCI. Higher degrees of frailty amplify the importance of pre-ICU antecedent characteristics in mortality determination, and incorporation of frailty into risk stratification progressively improves mortality prediction over the ICU stay. Given these findings, implementation of frailty measurement on ICU admission is desirable, and consideration of frailty status becomes of greater importance as ICU length of stay increases. As older patients are admitted to ICU, research targeted at reducing the incidence of PerCI and attenuating the impact of frailty on its development and outcome with concomitant vast resource consumption, is becoming a major public health priority.
References
Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, van Lint A, Chavan S, Bellomo R (2016) Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. Lancet Respir Med 4:566–573
Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S (2015) Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med 3:544–553
Nelson JE, Cox CE, Hope AA, Carson SS (2010) Chronic critical illness. Am J Respir Crit Care Med 182:446–454
Cox CE, Carson SS, Govert JA, Chelluri L, Sanders GD (2007) An economic evaluation of prolonged mechanical ventilation. Crit Care Med 35:1918–1927
Shaw M, Viglianti EM, McPeake J, Bagshaw SM, Pilcher D, Bellomo R, Iwashyna TJ, Quasim T (2020) Timing of onset, burden, and postdischarge mortality of persistent critical illness in Scotland, 2005–2014: a retrospective, population-based, observational study. Crit Care Explor 2:e0102
Viglianti EM, Bagshaw SM, Bellomo R, McPeake J, Wang XQ, Seelye S, Iwashyna TJ (2020) Hospital-level variation in the development of persistent critical illness. Intensive Care Med 46:1567–1575
Bagshaw SM, Stelfox HT, Iwashyna TJ, Bellomo R, Zuege D, Wang X (2018) Timing of onset of persistent critical illness: a multi-centre retrospective cohort study. Intensive Care Med 44:2134–2144
Darvall JN, Bellomo R, Bailey M, Paul E, Young PJ, Reid A, Rockwood K, Pilcher D (2021) Routine frailty screening in critical illness: a population-based cohort study in Australia and New Zealand. Chest 160:1292–1303
Darvall JN, Bellomo R, Bailey M, Paul E, Young PJ, Rockwood K, Pilcher D (2020) Frailty and outcomes from pneumonia in critical illness: a population-based cohort study. Br J Anaesth 125:730–738
Rockwood K, Theou O (2020) Using the clinical frailty scale in allocating scarce health care resources. Can Geriatr J 23:210–215
De Biasio JC, Mittel AM, Mueller AL, Ferrante LE, Kim DH, Shaefi S (2020) Frailty in critical care medicine: a review. Anesth Analg 130:1462–1473
Elliott A, Taub N, Banerjee J, Aijaz F, Jones W, Teece L, van Oppen J, Conroy S (2021) Does the clinical frailty scale at triage predict outcomes from emergency care for older people? Ann Emerg Med 77:620–627
Pulok MH, Theou O, van der Valk AM, Rockwood K (2020) The role of illness acuity on the association between frailty and mortality in emergency department patients referred to internal medicine. Age Ageing 49:1071–1079
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9:591–597
Hatheway OL, Mitnitski A, Rockwood K (2017) Frailty affects the initial treatment response and time to recovery of mobility in acutely ill older adults admitted to hospital. Age Ageing 46:920–925
Darvall JN, Boonstra T, Norman J, Murphy D, Bailey M, Iwashyna TJ, Bagshaw SM, Bellomo R (2019) Persistent critical illness: baseline characteristics, intensive care course, and cause of death. Crit Care Resusc 21:110–118
Jeffcote T, Foong M, Gold G, Glassford N, Robbins R, Iwashyna TJ, Darvall J, Bagshaw SM, Bellomo R (2019) Patient characteristics, ICU-specific supports, complications, and outcomes of persistent critical illness. J Crit Care 54:250–255
Tseitkin B, Martensson J, Eastwood GM, Brown A, Ancona P, Lucchetta L, Iwashyna TJ, Robbins R, Bellomo R (2020) Nature and impact of in-hospital complications associated with persistent critical illness. Crit Care Resusc 22:378–387
Viglianti EM, Kruser JM, Iwashyna T (2019) The heterogeneity of prolonged ICU hospitalisations. Thorax 74:1015–1017
Laupland KB, Ramanan M, Shekar K, Edwards F, Clement P, Tabah A (2021) Long-term outcome of prolonged critical illness: a multicentered study in North Brisbane, Australia. PLoS ONE 16:e0249840
Moitra VK, Guerra C, Linde-Zwirble WT, Wunsch H (2016) Relationship between ICU length of stay and long-term mortality for elderly ICU survivors. Crit Care Med 44:655–662
Darvall JN, Bellomo R, Paul E, Subramaniam A, Santamaria JD, Bagshaw SM, Rai S, Hubbard RE, Pilcher D (2019) Frailty in very old critically ill patients in Australia and New Zealand: a population-based cohort study. Med J Aust 211:318–323
Acknowledgements
The authors and the ANZICS CORE management committee would like to thank clinicians, data collectors and researchers at contributing sites. This research was conducted during the tenure of a Health Research Council of New Zealand Clinical Practitioner Fellowship held by Paul Young. The Medical Research Institute of New Zealand is supported by Independent Research Organisation funding from the Health Research Council of New Zealand.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. No funding to declare.
Author information
Authors and Affiliations
Contributions
JD: study design, literature search, data analysis/interpretation, manuscript writing. RB, DP, PY, KR: study design, study supervision, data analysis, data interpretation, writing/revision of manuscript. MB: study design, data analysis, data interpretation, writing/revision of manuscript. All authors had access to the study data, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
KR has asserted copyright of the Clinical Frailty Scale through Dalhousie University’s Industry, Liaison, and Innovation Office. Use is free for education, research, and not-for-profit health care. Users agree not to change or commercialize the scale. In addition to academic and hospital appointments, KR is Co-founder of Ardea Outcomes, which (as DGI Clinical) in the last 3 years has contracts with pharma and device manufacturers (Hollister, INmune, Novartis, Nutricia, Roche, Takeda) on individualized outcome measurement. In 2020 he attended an advisory board meeting with Nutricia on dementia, and chaired a Scientific Workshop and Technical Review Panel on frailty for the Singapore National Research Foundation. Otherwise any personal fees are for invited guest lectures, rounds and academic symposia, received directly from event organizers, for presentations on frailty. He is Associate Director of the Canadian Consortium on Neurodegeneration in Aging, itself funded by the Canadian Institutes for Health Research, the Alzheimer Society of Canada and several other charities.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Darvall, J.N., Bellomo, R., Bailey, M. et al. Impact of frailty on persistent critical illness: a population-based cohort study. Intensive Care Med 48, 343–351 (2022). https://doi.org/10.1007/s00134-022-06617-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-022-06617-0