Abstract
Objective
To investigate the accuracy of lung ultrasonography (LUS) in the quantification of lung water in critically ill patients by using quantitative computed tomography (CT) as the gold standard for the determination of lung weight.
Methods
Twenty consecutive patients admitted to an intensive care unit who underwent chest CT as a step in their clinical management were evaluated within 4 h by LUS. Lung weight, lung volume, and physical lung density were calculated from the CT scans using ad hoc software. Semiquantitative ultrasound assessment of lung water was performed by determining the ultrasound B-line score, defined as the total number of B-lines detectable in an anterolateral LUS examination.
Results
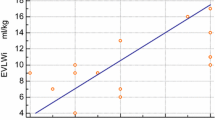
Good correlations were found between the B-line score and lung weight (r = 0.75, p < 0.05) and density (r = 0.82, p < 0.01), that only marginally increased when the lung density of the first 10 mm of subpleural lung tissue was evaluated (r = 0.83, p < 0.01). Moreover, values of subpleural lung density were not significantly different from values of the whole lung density (0.34 ± 0.11 vs. 0.37 ± 0.16 g/ml, p = ns). Very good correlations were found between the B-line score and both the weight (r = 0.85, p < 0.01) and the density (r = 0.88, p < 0.01) of the upper lobes. The weight of the lower lobes was not correlated with the B-line score (r = 0.14, p = ns).
Conclusions
Lung ultrasound B-lines are correlated with lung weight and density determined by CT. LUS may provide a reliable, simple and radiation-free lung densitometry in the intensive care setting.






Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Sakka SG, Klein M, Reinhart K, Meier-Hellmann A (2002) Prognostic value of extravascular lung water in critically ill patients. Chest 122:2080–2086
Martin GS, Eaton S, Mealer M, Moss M (2005) Extravascular lung water in patients with severe sepsis: a prospective cohort study. Crit Care 9:R74–R82
Isakow W, Schuster DP (2006) Extravascular lung water measurements and hemodynamic monitoring in the critically ill: bedside alternatives to the pulmonary artery catheter. Am J Physiol Lung Cell Mol Physiol 291:L1118–L1131
Tatsushi M, Kazumata K, Ajiki M, Ushikoshi S, Terasaka S (2007) Goal-directed fluid management by bedside transpulmonary hemodynamic monitoring after subarachnoid hemorrhage. Stroke 38:3218–3224
Pistolesi M, Giuntini C (1978) Assessment of extravascular lung water. Radiol Clin North Am 15:551–574
Rouby JJ, Puybasset L, Cluzel P, Richecoeur J, Lu Q, Grenier P (2000) Regional distribution of gas and tissue in acute respiratory distress syndrome. II. Physiological correlations and definition of an ARDS severity score: CT scan ARDS study group. Intensive Care Med 26:1046–1056
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 100:9–15
Roch A, Michelet P, Lambert D, Delliaux S, Saby C, Perrin G, Ghez O, Bregeon F, Thomas P, Carpentier JP, Papazian L, Auffray JP (2004) Accuracy of the double indicator method for measurement of extravascular lung water depends on the type of acute lung injury. Crit Care Med 32:811–817
Sakka SG, Reinhart K, Meier-Hellmann A (1999) Comparison of pulmonary artery and arterial thermodilution cardiac output in critically ill patients. Intensive Care Med 25:843–846
Rossi P, Wanecek M, Rudehill A, Konrad D, Weitzberg E, Oldner A (2006) Comparison of a single indicator and gravimetric technique for estimation of extravascular lung water in endotoxemic pigs. Crit Care Med 34:1437
Picano E (2004) Sustainability of medical imaging. BMJ 328:578–580
Lichtenstein D, Meziere G, Biderman P, Gepner A, Barre O (1997) The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 156:1640–1646
Picano E, Frassi F, Agricola E, Gligorova S, Gargani L, Mottola G (2006) Ultrasound lung comets: a clinically useful sign of extravascular lung water. J Am Soc Echocardiogr 19:356–363
Copetti R, Soldati G, Copetti P (2008) Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 6:16
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS) (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591
Gargani L (2011) Lung ultrasound: a new tool for the cardiologist. Cardiovasc Ultrasound 9:6
Lichtenstein D, Meziere G, Biderman P, Gepner A (2000) The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med 26:1434–1440
Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S (2002) Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT – initial experience. Radiology 225:210–214
Lichtenstein D, Pinsky MR, Jardin F (2007) General ultrasound in the critically ill. Springer, Berlin
Gryminski J, Krakowka P, Lypacewicz G (1976) The diagnosis of pleural effusion by ultrasonic and radiologic techniques. Chest 70:33
Yang P, Luh K, Chang D, Wu H, Yu C, Kuo S (1992) Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. AJR Am J Roentgenol 159:29
Mathis G, Blank W, Reissig A, Lechleitner P, Reuss J, Schuler A, Beckh S (2005) Thoracic ultrasound for diagnosing pulmonary embolism: a prospective multicenter study of 352 patients. Chest 128:1531–1538
Reissig AK (2007) Sonographic diagnosis and follow-up of pneumonia: a prospective study. Respiration 74:537–547
Gargani L, Frassi F, Soldati G, Tesorio P, Gheorghiade M, Picano E (2008) Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnoea: a comparison with natriuretic peptides. Eur J Heart Fail 10:70–77
Soldati G, Copetti R, Sher S (2009) Sonographic interstitial syndrome: the sound of lung water. J Ultrasound Med 28:163–174
Volpicelli G, Caramello V, Cardinale L, Mussa A, Bar F, Frascisco MF (2008) Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med 26:585–591
Jambrik Z, Monti S, Coppola V, Agricola E, Mottola G, Miniati M, Picano E (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 15:1265–1270
Agricola E, Bove T, Oppizzi M, Marino G, Zangrillo A, Margonato A, Picano E (2005) “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127:1690–1695
Gargani L, Lionetti V, Di Cristofano C, Bevilacqua G, Recchia FA, Picano E (2007) Early detection of acute lung injury uncoupled to hypoxemia in pigs using ultrasound lung comets. Crit Care Med 35:2769–2774
Lichtenstein D (2012) Fluid administration limited by lung sonography: the place of lung ultrasound in assessment of acute circulatory failure (the FALLS-protocol). Expert Rev Respir Med 6:155–162
Martin K, Ibáñez L, Avila L, Barré S, Kaspersen J (2005) Integrating segmentation methods from the insight toolkit into a visualization application. Med Image Anal 9:579–593
Drummond GB (1998) Computed tomography and pulmonary measurements. Br J Anaesth 80:665–671
Malbouisson LM, Preteux F, Puybasset L, Grenier P, Coriat P, Rouby JJ (2001) Validation of a software designed for computed tomographic (CT) measurement of lung water. Intensive Care Med 27:602–608
Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, Losappio S, Gattinoni L, Marini JJ (2001) Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med 164:122–130
Patroniti N, Bellani G, Manfio A, Maggioni E, Giuffrida A, Foti G, Pesenti A (2004) Lung volume in mechanically ventilated patients: measurement by simplified helium dilution compared to quantitative CT scan. Intensive Care Med 30:282–289
Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby JJ (2000) Regional distribution of gas and tissue in acute respiratory distress syndrome. I. Consequences for lung morphology. CT scan ARDS study group. Intensive Care Med 26:857–869
Gargani L, Doveri M, D’Errico L, Frassi F, Bazzichi ML, Delle Sedie A, Scali MC, Monti S, Mondillo S, Bombardieri S, Caramella D, Picano E (2009) Ultrasound lung comets in systemic sclerosis: a chest sonography hallmark of pulmonary interstitial fibrosis. Rheumatology (Oxford) 48:1382–1387
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ (2011) Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med 183:341–347
Bouhemad B, Liu ZH, Arbelot C, Zhang M, Ferarri F, Le-Guen M, Girard M, Lu Q, Rouby JJ (2010) Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med 38:84
Bellani G, Messa C, Guerra L, Spagnolli E, Foti G, Patroniti N, Fumagalli R, Musch G, Fazio F, Pesenti A (2009) Lungs of patients with acute respiratory distress syndrome show diffuse inflammation in normally aerated regions: a [18F]-fluoro-2-deoxy-d-glucose PET/CT study. Crit Care Med 37:2216
Mallamaci F, Benedetto F, Tripepi R, Rastelli S, Castellino P, Tripepi G, Picano E, Zoccali C (2010) Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging 3:586–594
Bedetti G, Gargani L, Corbisiero A, Frassi F, Poggianti E, Mottola G (2006) Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc Ultrasound 4:34
Shah S, Noble VE, Umulisa I, Dushimiyimana JM, Bukhman G, Mukherjee J, Rich M, Epino H (2008) Development of an ultrasound training curriculum in a limited resource international setting: successes and challenges of ultrasound training in rural Rwanda. Int J Emerg Med 1(3):193–196
Jambrik Z, Gargani L, Adamicza A, Kaszaki J, Varga A, Forster T, Boros M, Picano E (2010) B-lines quantify the lung water content: a lung ultrasound versus lung gravimetry study in acute lung injury. Ultrasound Med Biol 36:2004–2010
Delle Sedie A, Doveri M, Frassi F, Gargani L, D’Errico G, Pepe P, Bazzichi L, Riente L, Caramella D, Bombardieri S (2010) Ultrasound lung comets in systemic sclerosis: a useful tool to detect lung interstitial fibrosis. Clin Exp Rheumatol 28(5 Suppl 62):S54
Author information
Authors and Affiliations
Corresponding author
Addendum: data analysis
Addendum: data analysis
Lung weight and volume
These variables are derived by summing voxel volumes (V v) and attenuation values (A v) over the voxels pertaining to the lungs. Therefore, the difference in the calculated lung weight and density between a fine-grained and a coarse-grained CT scan is due to the coarser approximation of the contour lung regions only. The average voxel volume was 1.21 ± 0.31 mm3.
To calculate the weight of a voxel we applied a previously described method [33–35]. The correctness of the calculation is based on some working assumptions: (1) there is a linear correlation between the A v in Hounsfield units and the physical density of the tissue it represents, (2) the physical density of non-aerated lung parenchyma (ρ) (including vessels and extravascular water) can be approximated as ρ = 1 kg/l, namely the same physical density of water, corresponding to 0 HU, (3) the physical density of air corresponds to attenuation values ≤−1,000 HU. This means a voxel with such an attenuation value contains only air.
For each lung voxel we calculated its weight in grams (W v) and its gas content in milliliters (G v) by considering three cases:
-
A v ≥ 0: V v is entirely represented by lung parenchyma and therefore W v = ρ × V v, whereas G v = 0
-
Av ≤ −1,000: V v is entirely represented by gas and therefore W v = 0, whereas G v = V v
-
−1,000 < A v < 0: V v is partially represented by gas and the rest by parenchyma. According to assumption 1, we can write G v = A v × V v/−1,000. Consequently, W v = (V v − G v) × ρ.
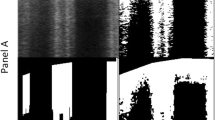
Segmentation algorithm
The first step in our algorithm was to segment the structures that are easily identifiable (e.g., trachea, main bronchi, bones) and to remove them from the image. In a second step, we selected a voxel as the starting point for the segmented region. Every voxel surrounding the segmented region was then automatically tested against an attenuation value threshold (0 HU or less) and included in the segmented region, if the test was passed. The process was repeated until no new voxels could be added to the segmented region. As a last step, we filtered the image in the segmented region to include smaller areas (e.g., consolidations, vessels, etc.) with attenuation values greater than 0 HU that did not pass the threshold test, but that were clearly inside the lung.
This computer-assisted methodology allowed us to perform lung segmentation in a very short time. Normal lungs could be segmented in less than 5 min which is much less time than is needed for manual segmentation. When lungs were very edematous, with pleural effusions and atelectasis, the time required increased and part of the segmentation task had to be performed manually.
Ultrasound beam simulation
Ultrasound energy is rapidly dissipated as the beam encounters alveolar air. Therefore, LUS actually provides information on a peripheral layer of subpleural lung tissue. The thickness of the LUS-explorable layer increases when the air content of the lung diminishes because the ultrasound beam is less reflected. We performed a mathematical simulation to estimate the distance traveled by the ultrasound beam as it is dissipated by the subpleural SLD extrapolated from CT images.
First, we segmented the CT scans considering only the anterolateral portions of the thorax corresponding to the lung surface evaluated by LUS. This was achieved by manually cutting the images at the mid-axillary lines. We then constructed a series of ten 1-mm thick concentric subpleural layers for each lung, and calculated their volume, weight and density (Fig. 1). Subpleural layers were automatically constructed by passing the segmented images through a distance filter that selects only voxels that are at most x millimeters away from the external contour of the lung, repeating the process for x in the range 1–10. We decided to construct ten layers corresponding to 1 cm of subpleural lung tissue because we estimated it to be the maximum distance reachable by the ultrasound beam. The upper and lower lobes were segmented using the same algorithm employed for construction of subpleural layers, simply increasing the distance filter tolerance.
We then used the resulting data to simulate the energy loss of the ultrasound beam as it travels through consecutive layers of tissue. The simulation is simply performed by calculating the energy reflection coefficient (R) between two interfaces with different acoustic impedance. More precisely R = [(Z 2−Z 1)/(Z 2 + Z 1)]2 where Z 1 and Z 2 are the acoustic impedances of two adjacent subpleural layers, respectively. We considered the point where 99 % of the beam energy is dissipated as the maximum distance (d M) reached by the beam. We use d M to calculate the density of the subpleural layer (SLD) with the corresponding thickness.
Our simulation of beam energy loss was based on the assumption that air and tissue are uniformly distributed in each layer. Since this is not the case in real lung, we obtained an overestimation of the maximum distance reached. However, the difference between SLD and total lung density was generally very small after the second subpleural layer (SLD − lung density = 0.03 ± 0.05 g/ml).
Rights and permissions
About this article
Cite this article
Baldi, G., Gargani, L., Abramo, A. et al. Lung water assessment by lung ultrasonography in intensive care: a pilot study. Intensive Care Med 39, 74–84 (2013). https://doi.org/10.1007/s00134-012-2694-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2694-x
Keywords
Profiles
- Francesco Forfori View author profile