Abstract
Purpose
Volume replacement remains one of the pillars of sepsis therapy. The effect of different volume solutions on kidney function in sepsis still remains unclear. We therefore determined the impact of crystalloid and colloid solutions on kidney function in a rodent model of abdominal sepsis induced by cecal ligation and puncture (CLP).
Methods
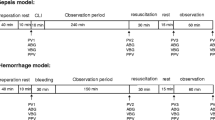
Anesthetized rats underwent the CLP procedure, whereas control animals were sham operated. Septic animals were treated with crystalloid and colloid solutions. Hemodynamic variables and blood gases were measured. After 24 h animals were re-anesthetized, the kidneys were harvested, and creatinine (crea), urea, cystatin C and neutrophil gelatinase-associated lipocalin (NGAL) were investigated.
Results
Septic animals exhibited a mortality rate of 19% after 24 h. Gelatin-treated animals showed significantly increased levels of crea and urea. Colloids [gelatin 4% (Gel) or hydroxyethyl starch 6% 130/0.4 (HES)] as volume replacement resulted in elevated levels of NGAL. The histopathological observations revealed that Gel- and HES-treated animals showed vesicles within epithelial cells of the tubulus system and an overall increased injury. In contrast, total injury scores in groups treated with crystalloids [0.9% NaCl (NaCl) and Sterofundin® ISO (SteroIso)] were not significantly different compared to sham-treated animals.
Conclusion
None of the examined volume solution was inert to the kidney. In a CLP rodent sepsis model, animals infused with balanced crystalloid SteroIso exhibited the least effects on kidney function. Both hydroxyethyl starch 6% 130/0.4 and gelatin 4% derogated the kidney, whereas gelatin was more harmful when compared with hydroxyethyl starch.
Similar content being viewed by others
Introduction
Sepsis is the major cause of death in most intensive care units (ICUs) despite the use of specific antibiotics, surgical intervention, invasive monitoring, volume substitution and organ replacement [1]. Moreover, sepsis has been recognized as an independent risk factor for acute renal failure (ARF) [2]. Sepsis-related ARF occurs in 20% of patients with moderate sepsis to more than 64% in cases of septic shock [3, 4]. However, the use of the ideal fluid substitution is still controversially discussed, especially regarding kidney function [5–7]. In European ICUs, hydroxyethyl starch and gelatin are commonly used as synthetic colloids in combination with crystalloids for volume resuscitation, whereas in North America crystalloids are preferred [2]. In recent years, several studies have yielded conflicting results for volume resuscitation using hydroxyethyl starch in critically ill patients, particularly with ARF [2, 5–12]. Administration of HES 10% (200/0.5) was associated with increased ARF and need for renal replacement therapy in septic patients [6]. HES 6% (200/0.6–0.66) was an independent risk factor for the development of ARF in patients with severe sepsis in a randomized multicenter study [5]. It has been suggested that HES 6% (130/0.4) may cause fewer side effects in kidney function compared to the old generation preparations. For other colloids, such as Gel, possible effects on renal function in sepsis have not been investigated in detail. However, new data from Schabinski et al. [13] suggest that the use of HES 6% (130/0.4) as well as gelatin 4% may be associated with a higher risk of ARF. Currently, the effects of colloids on renal function in severe sepsis remain unclear. Therefore, this study was designed to compare possible effects of different infusion solutions on renal function and histology in a rodent sepsis model.
Materials and methods
Animals
After animal care committee approval (Laboratory Animal Care and Use Committee of the District of Unterfranken, Germany), experiments were performed on 37 male Sprague–Dawley rats [330 ± 33 g bodyweight (BW), Harlan Winkelmann, Germany]. Animals were cared for according to the guidelines of the US National Institutes of Health as well as those of Germany. All rats were maintained on a standard diet with water ad libitum and 12-h day and night cycles. Animals were not fasted prior to or after the CLP procedure.
Experimental protocol
Animals were randomized to groups I–V (n = 6/group), group I: sham, group II: NaCl (NaCl 0.9% Fresenius Kabi, Germany), group III: SteroIso (Sterofundin® ISO B. Braun Melsungen AG, Germany), group IV: Gel (Gelafundin 4%, B. Braun Melsungen AG, Germany), group V: HES (6% HES 130/0,4, Voluven®, Fresenius Kabi, Germany), and anesthetized using isoflurane (Forene®, Abbott, Germany)/ nitrous oxide inhalation. For volume replacement and drug application, the right jugular vein was cannulated, and for continuous blood pressure measurement, heart rate (Hewlett Packard Model 88S) and gaining blood samples, the left carotid artery was canulated. Median laparotomy was performed, the cecum was mobilized, and only groups II–V underwent standardized CLP, as has been described in detail previously by Singleton et al. [14]. In brief, 25% of the cecum was ligated and punctured twice using a sterile 18-gauge needle. Postoperatively, all rats received fluid resuscitation as follows: Animals of all groups received 0.5 ml/100 g BW/h NaCl. Additionally, all sepsis groups received 1 ml/100 g BW/h NaCl (group II), SteroIso (group III), Gel (group IV) or HES (group V), respectively (Fig. 1). Analgesia was performed by the following protocol: group I: 0.25 µg/100 g BW/h fentanyl (Fagron, Germany); groups II–V: 2.0 µg/100 g BW/h fentanyl. After 24 h rats were reanasthetized using Midazolam (Midazolam-ratiopharm®, Ratiopharm, Germany) 0.7 mg/100 g BW/h and Fentanyl 7 µg/100 g BW/h, and for a sufficient anesthetic depth, isofluran was adapted. For a sufficient oxygenation (SaO2 > 93% and PaO2 > 60 mmHg) a tracheotomy was performed, and rats were mechanically ventilated with FiO2 0.4 using a Rodent Ventilator (Type: 7025, Hugo Sachs Elektronic KG, Germany). For cardiac output (CO) measurements, the right femoral artery was canulated, and a thermocatheter (MLT1402 T-type Ultra Fast Thermocouple, ADInstruments) was introduced. CO was measured by thermodilution using PowerLab® (ADInstruments). Parameters were calculated as described previously [15]. Blood gas values were measured using the ABL505 blood gas analyzer (Radiometer, Copenhagen). Animals that died before 24 h or had MAP levels <70 mmHg during the 24 h after CLP were excluded from the study.
Histopathology
Kidneys were removed 24 h after CLP for histopathological studies. Renal tissues were fixed in formaldehyde 3.5% (Otto Fischar, Germany) for more than 24 h. Tissues were then embedded in paraffin, and semi-thin sections (1 µm) were prepared and stained with hematoxylin and eosin for analyses of morphological alterations within the tissues. Additionally, PAS reactions served to document interstitial edema formation and possible ablation of epithelial cells from the basement membranes. The morphological alterations of kidneys were analyzed semi-quantitatively by a blinded investigator where 0 was given when no alterations were found, 1 for mild alterations, 2 for medium alterations and 3 for severe alterations. Criteria for histopathological assessment were formation of interstitial edema, dilatation of peritubular capillaries, vacuolization, ablation of tubular epithelium from the basement membrane, ablation of the brush border from the epithelium of the proximal tubuli and cell death (cell swelling and defragmentation of cell nuclei). Mean values from the scores of the latter criteria were taken together as the total injury score. Additionally, 25 randomly chosen glomeruli from tissue sections of each group were selected, and distal and proximal tubular cells around the glomeruli were analyzed under high-power fields (630× magnification), and a score of 0 to 4 was given: 0 = none; 1 = <25%, 2 = 25–50%, 3 = 50–75% and 4 = >75% of the epithelial cells displayed vesicles. Morphometric software was used to quantify the size of the vesicles.
Markers of kidney function
After 24-h plasma samples were drawn for determination of kidney function by measuring crea and urea by using routine laboratory methods; serum NGAL was measured in triplicate (ELISA Kit 041 dianova, Germany). Serum cystatin C was analyzed in triplicate by using a standardized ELISA (cystatin c ELISA KIT, AXXORA, Germany).
Statistical analysis
Values are expressed as mean ± standard error. Possible differences were assessed using Student’s t test and non-parametric Mann–Whitney statistics. SPSS 16.0 statistical software was used to analyze kidney functional, blood and vital parameters, and statistical significance was determined by analysis of variance (ANOVA followed by post-hoc Duncan test). Statistical significance was assumed at p < 0.05.
Results
Mortality
All sepsis animals exhibited a mortality rate of 19%, whereas all sham-operated animals survived and showed no signs of critical illness in the time course of the experiments. NaCl-treated animals showed the highest mortality rate of 50% (Fig. 2), followed by the colloid groups (25% each). Animals infused with the crystalloid SteroIso survived 24 h entirely.
Vital parameters
Among the groups there were no significant differences in mean arterial pressure (MAP), heart rate (HR), oxygen partial pressure (PaO2), oxygen saturation (SaO2), systemic vascular resistance index (SVR-I), pH, HCO3 − and SBE detectable (Table 1). Gel had a significantly lower hemoglobin (Hb) and arterial oxygen content (CaO2) compared to sham animals. The CIs and stroke volume index (SVI) increased significantly in the HES group. HES showed a significantly higher oxygen delivery index (DO2-I) compared to shams.
Histopathological observations
Histopathological observations revealed that total injury scores were significantly increased in the groups treated with the colloids HES 6% 130/0.4 and Gel 4% compared to the sham group, but not in the groups treated with crystalloids (Fig. 3a). Formation of interstitial edema was significantly increased only in the Gel group, although interstitial edema was also visible to some extent in the sham, NaCl and HES groups (Figs. 3b, 4). Dilatation of peritubular capillaries (PTC dilatation) was visible in SteroIso- as well as in Gel- and HES-treated animals. Detachment of epithelial cells from the basement membrane was not significantly different among groups, although the score tended to be higher in animals treated with colloids. Loss of brush border in the proximal tubuli was only increased in the Gel group. Cell death, verified by cell swelling and defragmentation of cell nuclei, appeared increased in kidneys of animals treated with HES and Gel, whereas no increased rate of cell death was detected in the other groups. Better than expected, in HES- and Gel-treated animals a large number of vesicles within the epithelial cells of the tubulus system were observed (see the arrows in Fig. 4g, i, j). This effect was most pronounced in the proximal tubuli. In all other groups (crystalloid and sham groups), such vesicles were not detectable (Fig. 4a–f). Additionally, the number of vesicles/area was counted, which demonstrated that both groups treated with colloids had significantly more vesicles than the other groups (Table 2). Gel-infused animals tended to have higher numbers of vesicles/area compared to the HES group. Quantification of vesicle sizes revealed that HES-treated animals displayed larger vesicles/area than the animals of the Gel group.
Representative images of the renal cortex after HE staining (a, c, e, g, i) and following PAS reactions (b, d, f, h, j) are shown. Some of the lesion criteria are exemplified. Therefore, magnifications of some areas are shown on the right (as indicated by the white arrows, b′, d′, f′, h′, j′, j″). Arrowheads in f, h, h′ point to peritubular dilatation. Arrows with broad heads in h′, j and j′ point to interstitial edema. Lines without arrowheads in j″ show tubular epithelial cells with defragmented nuclei. Arrows in g, i, j show vesicles in epithelial cells of the tubuli. Inset in g shows ablation of the tubular epithelium from the basement membrane (arrowheads). Inset in i shows loss of the brush border. For details, see text. Scale bars are 50 µm in i for HE-stained images (a, c, e, g, i) and in j for images showing PAS reactions (b, d, f, h, j)
Renal function
NGAL and cystatin C were measured to detect minor reductions of the glomerular filtration rate (GFR) and the early onset of ARF. Cystatin C, a 13-kD endogenous cysteine proteinase inhibitor, is produced by all nucleated cells at a constant rate, freely filtered by the glomerulus and reabsorbed, and catabolized but not secreted by the proximal tubule [16]. The serum concentration of cystatin C directly correlates with the GFR [17]. NGAL is one of the earliest and most robustly induced proteins in the kidney (distal nephron) after ischemic or nephrotoxic ARF in animal models [18] and in human adults with established ARF [19].
The parameters of kidney function revealed the following (Fig. 5): Crea and urea increased significantly in Gel-infused rats (crea: 0.53 ± 0.17 mg/dl sham vs. 0.69 ± 0.16 mg/dl Gel; urea: 48.8 ± 5.15 mg/dl sham vs. 69.9 ± 16.16 mg/dl Gel), whereas administration of NaCl, SteroIso and HES did not influence these parameters. NGAL was significantly increased in the colloidal groups (15,290 ± 8,560 U/ml sham vs. 82,854 ± 8,951 U/ml Gel, 40,736 ± 15,160 U/ml HES). Furthermore, Gel-treated animals had a significantly increased level of NGAL compared to the HES group. The NGAL level was elevated in animals treated with crystalloids, but did not reach significance. The cystatin C levels showed no significant changes among the different groups.
Discussion
Patients with severe sepsis often require large amounts of volume substitution to reach hemodynamic stability. The optimization of the volume status reduces mortality and morbidity—but how much of which fluid solution should be administered to critically ill patients [20, 21]? In the present study only one solution per group (except the basal fluid requirement) was used to examine the maximum influence of the volume solution. There were no significant changes in MAP, SVRI, HR, SaO2, PaO2, pH, HCO3 − and BE compared to shams, which could be interpreted as sufficient macrocirculation and oxygenation. CI was significantly increased in the HES group because of an increased SV-I caused by the expected higher volume expansion effect of HES. Colloid- and crystalloid-treated septic animals received the same amount of volume solution (1.0 ml/100 g BW/h). In preliminary studies to this survey, we revealed that the application of 1.5 ml crystalloids/100 g BW/h (on top of the basal fluid rate of 0.5 ml NaCl/100 g BW/h) in septic animals resulted in general edema formation (especially pulmonary edema) with no significant improvement of the hemodynamic variables (e.g., CI, MAP and SVI) when compared with septic animals treated with 1.0 ml crystalloids/100 g BW. Therefore, septic animals treated with colloids and crystalloids received the same amount of volume solution. Regarding MAP, cardiac index and DO2, no significant differences among crystalloid-, gelatin- and sham-treated animals were detectable. A lower Hb level in the Gel group can be explained by hematothoracis and bloody ascites secretion in the abdominal cavity probably caused by coagulopathy. Hydroxyethyl starches are polydisperse solutions with molecules of various weights and therefore with different elimination kinetics. Six percent HES 130/0.4 has an average molecular weight (MW) of 130 kD, in contrast to the monodisperse gelatin, where all molecules have a MW of 30 kD. HES metabolism in rats differs from humans because of an increased level of serum amylase in rodents [22, 23]. The expected average MW after 24 h of HES 130/0.4 in serum of healthy rats after a single bolus over 3 h is 63 kD [22]. In histopathological investigations, the HES group showed significantly more larger vesicles compared to Gel. It can be speculated that the different dispersal MW of HES and Gel may have caused the different sizes of the vesicles. However, it still remains unclear if the size and/or quantity of the vesicles is responsible for the deterioration in renal function [24].
There is still an ongoing controversy about the impact of hydroxylethyl starch solutions on the development of renal dysfunction, especially in septic patients [2, 5, 10, 25, 26]. We used the modern third generation 6% HES 130/0.4, which should have fewer side effects [9, 27]. The results of this study showed severe histological renal derangements with 6% HES 130/0.4. The HES group showed more cell death in tubulus cells compared to crystalloids and the sham group. We have been able to show that the modern HES also induced osmotic nephrosis-like lesions (ONL). The HES-treated group had significantly more vesicles compared to the sham and crystalloid groups [28, 29]. Comparing the histological results with functional parameters, only NGAL showed a significantly increased serum level in HES-treated animals [18]. Because we had no increased levels of urea and crea, we hypothesize that we detected the early onset of ARF in the HES group. The later onset of ARF in the HES group may be due to a better DO2-I compared to Gel, which may result in a longer sufficient oxygen supply for the tubulus cells. This hypothesis is in contrast to the previous findings that the impaired kidney function in a rodent LPS sepsis model is not due to oxygen deficiency [30].
In line with the VISEP study, many ICUs have replaced HES by Gel as the first-line volume solution [6]. For Gel, no dose limitation is recommended, even in cases of renal impairment [11]. The results of this study contradict the hypothesis that gelatin 4% has no influence on the kidneys. To our knowledge, we have demonstrated for the first time that septic rats treated with gelatin also exhibited incorporated vesicles in the proximal tubulus cells as well as significantly increased levels of renal functional parameters. These results show a severe harmful impact of gelatin on the kidneys in septic rats. Gel impaired renal function in our septic model probably earlier and more severely, resulting in increased NGAL, urea and crea. The significant loss of the brush border in the proximal tubules cells may explain this reduced function of the kidney treated by gelatin 4%. The smaller MW of Gel suggests an earlier contact to tubulus cells by passing the glomerular basement membrane at the beginning of infusion. This may lead to an earlier onset of ARF compared to HES and explain the increased level of crea and urea. Our results agree with data from a clinical trial of elderly patients undergoing cardiac surgery and gelatin treatment that demonstrated significantly increased crea and NGAL levels after surgery [26].
In our study crystalloid-treated animals showed less renal impairment when compared with colloid-treated animals. These results support the interpretation that crystalloids should be preferred in cases of sepsis regarding to ARF. Additionally, there is no evidence for an improvement in survival by using colloids in critically ill patients [31]. The use of a combination with balanced starch and crystalloid solution in elderly patients who had undergone cardiac surgery had a beneficial effect on kidney integrity, which is in line with our data [32]. However, in our experimental setup, animals treated with NaCl had the highest and SteroIso the lowest mortality rate. The improved outcome in SteroIso-treated rats may be due to its balanced solution pattern [33]. Swollen tubular cells may cause the onset of ARF by direct tubular obstruction as seen in SteroIso-treated animals (Fig. 4c) [34]. This hypothesis was already challenged more than 30 years ago, which is now substantiated by our present data [34].
In summary, none of the examined volume solutions in our experiment was inert to the kidney. In a CLP rodent sepsis model, SteroIso-infused animals exhibited the least effects on kidney function. Both colloids derogated the kidney, whereas the Gel group was more harmful compared to HES. More investigations are needed to determine the metabolic pathway of colloid and crystalloid solutions to prevent renal failure, especially in critical situations like sepsis.
References
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150
Sakr Y, Payen D, Reinhart K, Sipmann FS, Zavala E, Bewley J, Marx G, Vincent JL (2007) Effects of hydroxyethyl starch administration on renal function in critically ill patients. Br J Anaesth 98:216–224
Trof RJ, Di Maggio F, Leemreis J, Groeneveld AB (2006) Biomarkers of acute renal injury and renal failure. Shock 26:245–253
Bagshaw SM, Lapinsky S, Dial S, Arabi Y, Dodek P, Wood G, Ellis P, Guzman J, Marshall J, Parrillo JE, Skrobik Y, Kumar A (2009) Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med 35:871–881
Schortgen F, Lacherade JC, Bruneel F, Cattaneo I, Hemery F, Lemaire F, Brochard L (2001) Effects of hydroxyethylstarch and gelatin on renal function in severe sepsis: a multicentre randomised study. Lancet 357:911–916
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139
Cittanova ML, Leblanc I, Legendre C, Mouquet C, Riou B, Coriat P (1996) Effect of hydroxyethylstarch in brain-dead kidney donors on renal function in kidney-transplant recipients. Lancet 348:1620–1622
Su F, Wang Z, Cai Y, Rogiers P, Vincent JL (2007) Fluid resuscitation in severe sepsis and septic shock: albumin, hydroxyethyl starch, gelatin or ringer’s lactate-does it really make a difference? Shock 27:520–526
Jungheinrich C, Scharpf R, Wargenau M, Bepperling F, Baron JF (2002) The pharmacokinetics and tolerability of an intravenous infusion of the new hydroxyethyl starch 130/0.4 (6%, 500 mL) in mild-to-severe renal impairment. Anesth Analg 95:544–551 (table of contents)
Wiedermann CJ (2008) Systematic review of randomized clinical trials on the use of hydroxyethyl starch for fluid management in sepsis. BMC Emerg Med 8:1
Ragaller MJ, Theilen H, Koch T (2001) Volume replacement in critically ill patients with acute renal failure. J Am Soc Nephrol 12 Suppl 17:S33–S39
Boldt J, Wolf M (2008) Identification of renal injury in cardiac surgery: the role of kidney-specific proteins. J Cardiothorac Vasc Anesth 22:122–132
Schabinski F, Oishi J, Tuche F, Luy A, Sakr Y, Bredle D, Hartog C, Reinhart K (2009) Effects of a predominantly hydroxyethyl starch (HES)-based and a predominantly non HES-based fluid therapy on renal function in surgical ICU patients. Intensive Care Med 35:1539–1547
Singleton KD, Wischmeyer PE (2003) Distance of cecum ligated influences mortality, tumor necrosis factor-alpha and interleukin-6 expression following cecal ligation and puncture in the rat. Eur Surg Res 35:486–491
Shinoda T, Smith CE, Khairallah PA, Fouad-Tarazi FM, Estafanous FG (1991) Effects of propranolol on myocardial performance during acute normovolemic hemodilution. J Cardiothorac Vasc Anesth 5:15–22
Herget-Rosenthal S, Bokenkamp A, Hofmann W (2007) How to estimate GFR-serum creatinine, serum cystatin C or equations? Clin Biochem 40:153–161
Tenstad O, Roald AB, Grubb A, Aukland K (1996) Renal handling of radiolabelled human cystatin C in the rat. Scand J Clin Lab Invest 56:409–414
Devarajan P (2008) Neutrophil gelatinase-associated lipocalin (NGAL): a new marker of kidney disease. Scand J Clin Lab Invest Suppl 241:89–94
Mori K, Lee HT, Rapoport D, Drexler IR, Foster K, Yang J, Schmidt-Ott KM, Chen X, Li JY, Weiss S, Mishra J, Cheema FH, Markowitz G, Suganami T, Sawai K, Mukoyama M, Kunis C, D’Agati V, Devarajan P, Barasch J (2005) Endocytic delivery of lipocalin–siderophore–iron complex rescues the kidney from ischemia–reperfusion injury. J Clin Invest 115:610–621
Rivers EP, Nguyen HB, Huang DT, Donnino M (2004) Early goal-directed therapy. Crit Care Med 32:314–315 (author reply 315)
Rivers EP, Coba V, Whitmill M (2008) Early goal-directed therapy in severe sepsis and septic shock: a contemporary review of the literature. Curr Opin Anaesthesiol 21:128–140
Wagenblast M (2004) Molmassenverteilung der in Milz und Leber gespeicherten hydroxyethylstärke (HES) bei Ratten nach intravenöser Applikation - polymeranalytische Untersuchungen mittels Kopplung der Ausschluss-Chromatographie und Mehrwinkel-Laser-Streulicht-Detektion. Deutsche Veterinärmedizinische Gesellschaft Service GmbH
Lenz K, Schimetta W, Polz W, Kroll W, Gruy-Kapral C, Magometschnigg D (2000) Intestinal elimination of hydroxyethyl starch? Intensive Care Med 26:733–739
Suttner S, Boldt J (2004) Volume replacement with hydroxyethyl starch: is there an influence on kidney function? Anasthesiol Intensivmed Notfallmed Schmerzther 39:71–77
Boldt J, Brosch C, Ducke M, Papsdorf M, Lehmann A (2007) Influence of volume therapy with a modern hydroxyethylstarch preparation on kidney function in cardiac surgery patients with compromised renal function: a comparison with human albumin. Crit Care Med 35:2740–2746
Boldt J, Brosch C, Rohm K, Papsdorf M, Mengistu A (2008) Comparison of the effects of gelatin and a modern hydroxyethyl starch solution on renal function and inflammatory response in elderly cardiac surgery patients. Br J Anaesth 100:457–464
Boldt J, Suttner S (2005) Plasma substitutes. Minerva Anestesiol 71:741–758
Ginz HF, Gottschall V, Schwarzkopf G, Walter K (1998) Excessive tissue storage of colloids in the reticuloendothelial system. Anaesthesist 47:330–334
Sirtl C, Laubenthal H, Zumtobel V, Kraft D, Jurecka W (1999) Tissue deposits of hydroxyethyl starch (HES): dose-dependent and time-related. Br J Anaesth 82:510–515
Johannes T, Mik EG, Nohe B, Raat NJ, Unertl KE, Ince C (2006) Influence of fluid resuscitation on renal microvascular PO2 in a normotensive rat model of endotoxemia. Crit Care 10:R88
Perel P, Roberts I (2007) Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev: CD000567
Boldt J, Suttner S, Brosch C, Lehmann A, Rohm K, Mengistu A (2009) The influence of a balanced volume replacement concept on inflammation, endothelial activation, and kidney integrity in elderly cardiac surgery patients. Intensive Care Med 35:462–470
Zander R (2002) Base excess and lactate concentration in infusion solutions and blood products. Anasthesiol Intensivmed Notfallmed Schmerzther 37:359–363
Dickenmann M, Oettl T, Mihatsch MJ (2008) Osmotic nephrosis: acute kidney injury with accumulation of proximal tubular lysosomes due to administration of exogenous solutes. Am J Kidney Dis 51:491–503
Acknowledgment
We appreciate the technical help and support of the histological work of Prof. Dr. H.J. Gröne, Deutsches Krebsforschungszentrum, Heidelberg, Germany. This work was supported by grants from the Interdisziplinäre Zentrum für klinische Forschung (IZKF) of the University of Wuerzburg.
Conflict of interest statement
No author has any conflict of interest to disclose with respect to this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. A. Schick and T. J. Isbary contributed equally to this work.
Rights and permissions
About this article
Cite this article
Schick, M.A., Isbary, T.J., Schlegel, N. et al. The impact of crystalloid and colloid infusion on the kidney in rodent sepsis. Intensive Care Med 36, 541–548 (2010). https://doi.org/10.1007/s00134-009-1704-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1704-0