Abstract
Objective
To assess the relationship between blood glucose concentrations (BSL) and intolerance to gastric feeding in critically ill patients.
Design
Prospective, case-controlled study.
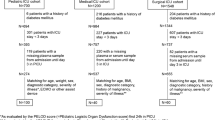
Patients and participants
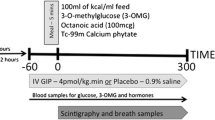
Two-hourly BSL and insulin requirements over the first 10 days after admission were assessed in 95 consecutive feed-intolerant (NG aspirate > 250 ml during feed) critically ill patients and 50 age-matched, feed-tolerant patients who received feeds for at least 3 days. Patients with diabetes mellitus were excluded. A standard insulin protocol was used to maintain BSL at 5.0–7.9 mmol.
Measurements and results
The peak BSLs were significantly higher before and during enteral feeding in feed-intolerant patients. The mean and trough BSLs were, however, similar between the two groups on admission, 24 h prior to feeding and for the first 4 days of feeding. The variations in BSLs over 24 h before and during enteral feeding were significantly greater in feed-intolerant patients. A BSL greater than 10 mmol/l was more prevalent in patients with feed intolerance during enteral feeding. The time taken to develop feed intolerance was inversely related to the admission BSL (r = –0.40). The amount of insulin administered before and during enteral feeding was similar between the two groups.
Conclusions
Feed intolerance in critically ill patients is associated with a greater degree of glycaemic variation, with a greater number of patients with transient hyperglycaemia. These data suggest more intensive insulin therapy may be required to minimize feed intolerance, an issue that warrants further study.






Similar content being viewed by others
References
Rayner CK, Samsom M, Jones KL, Horowitz M (2001) Relationships between upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care 24:371–381
Schvarcz E, Palmer M, Aman J, Horowitz M, Stridsberg M, Berne C (1997) Physiological hyperglycaemia slows gastric emptying in normal subjects and patients with insulin-dependent DM. Gastroenterology 113:60–66
Andrews JM, Rayner CK, Doran S, Hebbard G, Horowitz M (1998) Physiological changes in blood glucose affect appetite and pyloric motility during antroduodenal lipid infusion. Am J Physiol 275:G797–G804
Jones KL, Kong MF, Berry MK, Samson M, Horowitz M (1999) The effect of erythromycin on gastric emptying is modified by physiological changes in the blood glucose concentration. Am J Gastroenterol 94:2074–2079
MacGregor IL, Gueller R, Watts HD, Meyer J (1976) The effect of acute hyperglycemia on gastric emptying in man. Gastroenterology 70:190–196
Oster-Jorgensen E, Pedersen SA, Larsen ML (1990) The influence of induced hyperglycemia on gastric emptying in healthy humans. Scand J Lab Clin Invest 50:831–836
Fraser R, Horowitz M, Maddox A, Harding P, Chatterton B, Dent J (1990) Hyperglycaemia slows gastric emptying in type 1 DM. Diabetologia 30:675–680
Hebbard GS, Sun WM, Dent J, Horowitz M (1996) Hyperglycaemia affects proximal gastric motor and sensory function in normal subjects. Eur J Gastroenterol Hepatol 8:211–217
Schvarcz E, Palmer M, Aman J, Lindkvist B, Backman K (1995) Hypoglycemia increases the gastric emptying rate in healthy subjects. Diabetes Care 18:674–676
Horowitz M, Wishart JM, Jones KL, Hebbard G (1996) Gastric emptying in diabetes: an overview. Diabet Med 13:S16–S22
Heyland D, Cook DJ, Winder B, Brylowski L, Van demark H, Guyatt G (1995) Enteral nutrition in the critically ill patient: a prospective survey. Crit Care Med 23:1055–1060
Mentec H, Dupont H, Bocchetti M, Cani P, Ponche F, Bleichner G (2001) Upper digestive intolerance during enteral nutrition in critically ill patients: frequency, risk factors, and complications. Crit Care Med 29:1955–1961
Multu G, Multu E, Factor P (2001) Gastrointestinal complications in patients receiving mechanical ventilation. Chest 119:1222–1241
Nguyen N, Fraser R, Chapman M, Bryant L, Holloway RH, Vozzo R, Feinle-Bisset C (2006) Impaired proximal gastric relaxation in response to small intestinal nutrients in critically ill patients. World J Gastroenterol 21:4383–4388
Chapman M, Fraser R, Vozzo R, Bryant L, Tam W, Nguyen NQ, Zacharakis B, Butler R, Davidson G, Horowitz M (2005) Antro-pyloro-duodenal motor responses to gastric and duodenal nutrient in critically ill patients. Gut 54:1384–1390
Dive A, Moulart M, Jonard P, Jamart J, Mahieu P (1994) Gastroduodenal motility in mechanically ventilated critically ill patients: a manometric study. Crit Care Med 22:441–447
Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P (2003) Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr 27:355
Mullen JL, Buzby GP, Matthews D, Smale B, Rosato E (1980) Reduction of operative morbidity and mortality by combined preoperative and postoperative nutritional support. Ann Surg 192:604–609
Dempsey DT, Mullen JL, Buzby GP (1988) The link between nutritional status and clinical outcome: can nutritional intervention modify it? Am J Clin Nutr 47:352–356
Nguyen NQ, Ng MP, Chapman M, Fraser R, Holloway RH (2007) The impact of admission diagnosis on gastric emptying in critically ill patients. Crit Care 11:R16
Boord J, Graber A, Christman J (2001) Practical management of diabetes in critically ill patients. Am J Respir Crit Care Med 164:1763–1767
McCowan KC, Malhoota A, Bistrian BR (2001) Endocrine and metabolic dysfunction syndromes in the critically ill. Crit Care Clin 17:107–124
O'Neill PA, Davies, Fullerton KJ (1991) Stress hormone and blood glucose response following acute stroke in the elderly. Stroke 22:842–847
Van den Berghe G, Wouters P, Weekers F (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367
Van den Berghe G, Wouters PJ, Bouillon R (2003) Outcome benefit of intensive insulin therapy in the critically ill: insulin dose versus glycemic control. Crit Care Med 31:359–366
Krinsley JS (2004) Hyperglycemia is strongly associated with increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 79:992–1000
Nguyen NQ, Chapman M, Fraser R, Bryant L, Wishart J, Holloway RH, Horowitz M (2007) Feed intolerance in critical illness is associated with increased basal and nutrient-stimulated plasma cholecystokinin concentrations. Crit Care Med 35:82–88
Nguyen NQ, Chapman M, Fraser R, Ritz M, Bryant L, Butler R, Davidson G, Zacharakis B, Holloway RH (2006) Longstanding type II diabetes mellitus is not a risk factor for slow gastric emptying in critically ill patients. Intensive Care Med 32:1365–1370
Chapman MJ, Fraser RJ, Kluger MT, Buist M, De Nichilo D (2000) Erythromycin improves gastric emptying in critically ill patients intolerant of nasogastric feeding. Crit Care Med 28:2334–2337
McClave SA, Snider HL, Lowen CC, McLaughlin A, Greene L, McCombs R, Rodgers L, Wright R, Roy T, Schumer MP (1992) Use of residual volume as a marker for enteral feeding intolerance: prospective blinded comparison with physical examination and radiographic findings. JPEN J Parenter Enteral Nutr 16:99–105
De Beaux I, Chapman M, Fraser R, Finnis M, De Keulenaer B, Liberalli D, Satanek M (2001) Enteral nutrition in the critically ill: a prospective survey in an Australian intensive care unit. Anaesth Intensive Care 29:619–622
Boullata J, Williams J, Cottrell F, Hudson L, Compher C (2007) Accurate determination of energy needs in hospitalized patients. J Am Diet Assoc 107:393–401
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler L, Kitabchi A (2002) Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87:978–982
Glatzle J, Leutenegger CM, Mueller MH (2004) Mesenteric lymph collected during peritonitis or sepsis potently inhibits gastric motility in rats. J Gastrointest Surg 8:645–652
Yudkin JS, Stehouwer CD, Emeis JJ (1999) C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 19:972–978
Meier J, Weyhe D, Michaely M, Senkal M, Zumtolel V, Holst J, Nauck M, Schmidt W, Gallwitz B (2005) Intravenous glucagon-like peptide 1 normalizes blood glucose after major surgery in patients with type 2 diabetes. Crit Care Med 32:848–851
Mayer AP, Durward A, Turner C, Skellett S, Dalton N, Tibby SM, Murdoch I (2002) Amylin is associated with delayed gastric emptying in critically ill children. Intensive Care Med 28:336–340
Van den Berghe G (2004) How does blood glucose control with insulin save lives in intensive care? J Clin Invest 114:1187–1195
Langouche L, Vanhorebeek I, Vlasselaers D, Vander Perre S, Wouters PJ, Skogstrand K, Hansen TK, Van den Berghe G (2005) Intensive insulin therapy protects the endothelium of critically ill patients. J Clin Invest 115:2277–2286
Jeschke MG, Klein D, Bolder U, Herndon D (2004) Insulin attenuates the systemic inflammatory response in endotoxemic rats. Endocrinology 145:4084–4093
Bland D, Fankhanel Y, Langford, Lee M, Lee S, Maloney C, Rogers M, Zimmerman G (2005) Intensive versus modified conventional control of blood glucose level in medical intensive care patients: a pilot study. Am J Crit Care 14:370–376
McClave SA, Lukan JK, Stefater JA, Lowen C, Looney S, Matheson P, Gleeson K, Spain D (2005) Poor validity of residual volumes as a marker for risk of aspiration in critically ill patients. Crit Care Med 33:324–330
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the National Health and Medical Research Council of Australia.
Rights and permissions
About this article
Cite this article
Nguyen, N., Ching, K., Fraser, R. et al. The relationship between blood glucose control and intolerance to enteral feeding during critical illness. Intensive Care Med 33, 2085–2092 (2007). https://doi.org/10.1007/s00134-007-0869-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0869-7