Abstract
Objective
The transpulmonary thermodilution technique enables measurement of cardiac index (CI), intrathoracic blood volume (ITBV), global end-diastolic volume (GEDV), and extravascular lung water (EVLW). In this study, we analyzed the robustness of this technique during an acute increase in systemic vascular resistance (SVR).
Design
Prospective, clinical study.
Setting
Surgical intensive care unit in a university hospital.
Patients and methods
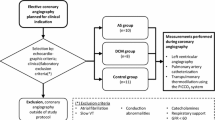
Twenty-four mechanically ventilated septic shock patients, who for clinical indications underwent extended hemodynamic monitoring by transpulmonary thermodilution and continuously received norepinephrine.
Interventions and main results
After baseline measurements, mean arterial pressure was increased briefly by increasing norepinephrine dosage and hemodynamic measurements were repeated before a control measurement was obtained. At each time point, 15 cc of 0.9% saline (< 8 °C) was administered by central venous injection in triplicate. Fluid status and respirator adjustments were kept constant. ANOVA with an all-pairwise comparison method was used for statistical analysis. Heart rate, central venous pressure, and EVLW remained constant throughout, while SVR significantly changed from 551 ± 106 to 746 ± 91 dyn*s*cm−5 and again to 566 ± 138 dyn*s*cm−5 (p < 0.05). However, CI and central blood volumes showed a reversible significant increase, i.e., ITBV went from 816 ± 203 to 867 ± 195 ml/m2 and then to 821 ± 205 ml/m2 and GEDV from 703 ± 178 to 747 ± 175 ml/m2 and finally to 704 ± 170 ml/m2, respectively. In eight patients, 2-D echocardiography was applied and revealed a reversible increase in left-ventricular end-diastolic area.
Conclusion
An acute increase in SVR by increasing norepinephrine dosage results in a reversible increase in central blood volumes (ITBV, GEDV) as measured by transpulmonary thermodilution and supported by echocardiography.

Similar content being viewed by others
References
Neumann P (1999) Extravascular lung water and intrathoracic blood volume: double versus single indicator dilution technique. Intensive Care Med 25:216–219
Sakka SG, Ruhl CC, Pfeiffer UJ, Beale R, McLuckie A, Reinhart K, Meier-Hellmann A (2000) of cardiac preload and extravascular lung water by single transpulmonary thermodilution. Intensive Care Med 26:180–187
Lichtwarck-Aschoff M, Zeravik J, Pfeiffer UJ (1992) Intrathoracic blood volume accurately reflects circulatory volume status in critically ill patients with mechanical ventilation. Intensive Care Med 18:142–147
Sakka SG, Bredle DL, Reinhart K, Meier-Hellmann A (1999) Comparison between intrathoracic blood volume and cardiac filling pressures in the early phase of hemodynamic instability of patients with sepsis or septic shock. J Crit Care 14:78–83
Godje O, Peyerl M, Seebauer T, Lamm P, Mair H, Reichart B (1998) Central venous pressure, pulmonary capillary wedge pressure and intrathoracic blood volumes as preload indicators in cardiac surgery patients. Eur J Cardiothorac Surg 13:533–539
Hoeft A, Schorn B, Weyland A, Scholz M, Buhre W, Stepanek E, Allen SJ, Sonntag H (1994) Bedside assessment of intravascular volume status in patients undergoing coronary bypass surgery. Anesthesiology 81:76–86
Mitchell JP, Schuller D, Calandrino FS, Schuster DP (1992) Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization. Am Rev Respir Dis 145:990–998
Eisenberg PR, Hansbrough JR, Anderson D, Schuster DP (1987) A prospective study of lung water measurement during patient management in an intensive care unit. Am Rev Respir Dis 136:662–668
Hinder F, Poelaert JI, Schmidt C, Hoeft A, Mollhoff T, Loick HM, Van Aken H (1998) Assessment of cardiovascular volume status by transoesophageal echocardiography and dye dilution during cardiac surgery. Eur J Anaesthesiol 15:633–640
Hofer CK, Furrer L, Matter-Ensner S, Maloigne M, Klaghofer R, Genoni M, Zollinger A (2005) Volumetric preload measurement by thermodilution: a comparison with transoesophageal echocardiography. Br J Anaesth 94:748–755
Buhre W, Kazmaier S, Sonntag H, Weyland A (2001) Changes in cardiac output and intrathoracic blood volume: a mathematical coupling of data? Acta Anaesthesiol Scand 45:863–867
McLuckie A, Bihari D (2000) Investigating the relationship between intrathoracic blood volume index and cardiac index. Intensive Care Med 26:1376–1378
Lichtwarck-Aschoff M, Beale R, Pfeiffer UJ (1996) Central venous pressure, pulmonary artery occlusion pressure, intrathoracic blood volume, and right ventricular end-diastolic volume as indicators of cardiac preload. J Crit Care 11:180–188
Buhre W, Weyland A, Schorn B, Scholz M, Kazmaier S, Hoeft A, Sonntag H (1999) Changes in central venous pressure and pulmonary capillary wedge pressure do not indicate changes in right and left heart volume in patients undergoing coronary artery bypass surgery. Eur J Anaesthesiol 16:11–17
Sakka SG, Bredle DL, Reinhart K, Meier-Hellmann A (1999) Comparison between intrathoracic blood volume and cardiac filling pressures in the early phase of hemodynamic instability of patients with sepsis or septic shock. J Crit Care 14:78–83
Lichtwarck-Aschoff M, Zeravik J, Pfeiffer UJ (1992) Intrathoracic blood volume accurately reflects circulatory volume status in critically ill patients with mechanical ventilation. Intensive Care Med 18:142–147
Combes A, Berneau JB, Luyt CE, Trouillet JL (2004) Estimation of left ventricular systolic function by single transpulmonary thermodilution. Intensive Care Med 30:1377–1383
Weissman C, Ornstein EJ, Young WL (1993) Arterial pulse contour analysis trending of cardiac output: hemodynamic manipulations during cerebral arteriovenous malformation resection. J Clin Monit 9:347–353
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented in part at the 19th annual meeting of the European Society of Intensive Care Medicine, 24–27 September 2006, Barcelona.
Samir Sakka has received fees from Pulsion Medical Systems AG, Munich, Germany, for giving lectures.
Rights and permissions
About this article
Cite this article
Kozieras, J., Thuemer, O. & Sakka, S.G. Influence of an acute increase in systemic vascular resistance on transpulmonary thermodilution-derived parameters in critically ill patients. Intensive Care Med 33, 1619–1623 (2007). https://doi.org/10.1007/s00134-007-0669-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0669-0