Abstract
Objective
To document the prevalence of anemia among patients admitted to intensive care (ICU) and, among survivors, at ICU discharge when restrictive transfusion practice was used.
Design
This was an observational cohort study.
Setting
Ten of the 26 general ICUs in Scotland.
Patients and participants
One thousand twenty-three sequential ICU admissions over 100 days, representing 44% of all ICU admissions in Scotland during the study period, studied daily from admission to discharge or death in the ICU.
Interventions
None.
Measurements and results
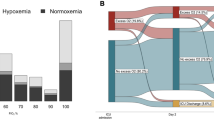
The median transfusion trigger used, in the absence of bleeding, was 78 g/l (interquartile range 73–84); <2% of transfusion triggers were above the upper limit of the national transfusion trigger guideline (100 g/l). Overall, 25% of admissions had a hemoglobin concentration <90 g/l at ICU admission. Seven hundred sixty-six patients admitted survived to ICU discharge. Among these, the prevalence of anemia (male <130 g/l; female <115 g/l) at ICU discharge was 87.0 (95% CI: 83.6 to 89.9)% for males and 79.6 (74.8 to 83.7)% for females. Of the male survivors 24.1 (20.3 to 28.3)% and of the female 27.9 (23.4 to 33.2)% had a hemoglobin <90 g/l at ICU discharge. The prevalence was similar for patients with and without pre-existing ischemic heart disease. Logistic regression found independent associations between having a hemoglobin concentration <90 g/l at ICU discharge and the first measured hemoglobin in ICU, the presence of acute renal failure and thrombocytopenia during ICU stay.
Conclusions
Anemia is highly prevalent in ICUs that use restrictive transfusion triggers. The impact of anemia on functional recovery after intensive care requires investigation.


Similar content being viewed by others
References
Hebert PC, Fergusson DA (2002) Red blood cell transfusions in critically ill patients. JAMA 288:1525–1526
Ho J, Sibbald WJ, Chin-Yee IH (2003) Effects of storage on efficacy of red cell transfusion: when is it not safe? Crit Care Med 31:S687–S697
McLellan SA, Walsh TS, McClelland DB (2002) Should we demand fresh red blood cells for perioperative and critically ill patients? Br J Anaesth 89:537–540
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion requirements in critical care investigators, Canadian Critical Care Trials Group. N Engl J Med 340:409–417
Hill SR, Carless PA, Henry DA, Carson JL, Hebert PC, McClleland DBL, Henderson KM (2002) Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion (Cochrane Review). In: The Cochrane Library, Issue 2. Oxford: Update Software. 2002
Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, Meier-Hellmann A, Nollet G, Peres-Bota D (2002) Anemia and blood transfusion in critically ill patients. JAMA 288:1499–1507
Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Abraham E, MacIntyre NR, Shabot MM, Duh MS, Shapiro MJ (2004) The CRIT Study: Anemia and blood transfusion in the critically ill—current clinical practice in the United States. Crit Care Med 32:39–52
Walsh TS, Garrioch M, Maciver C, Lee RJ, MacKirdy F, McClelland DB, Kinsella J, Wallis C for the ATICS study group (2004) Red cell requirements for intensive care units adhering to evidence-based transfusion guidelines. Transfusion 44:1405–1411
(2001) Perioperative blood transfusion for elective surgery: a national clinical guideline. www.sign.ac.uk
Walsh TS, McClelland DBL, Lee RJ, Garrioch M, Maciver CR, McArdle F, Crofts SL, Mellor I, for the ATICS Study Group (2005) Does documented ischaemic heart disease influence the observed threshold haemoglobin concentration for red cell transfusions in intensive care units? Brit J Anaesth 94:445–452
Walsh TS, Lee RJ Maciver M, McClelland DB (2003) Prevalence of anaemia at discharge from the intensive care unit (ICU): multicentre study in Scottish ICUs. Brit J Anaesth 90:569P
Walsh TS, Lee RJ, Maciver CR, Garrioch M, MacKirdy F, Scott SA, Binning AR, McClelland DBL (2004) An analysis of factors associated with a haemoglobin concentration of <90 g/l at ICU discharge. Br J Anaesth 92:617P
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A., Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Int Care Med 22:707–710
French CJ, Bellomo R, Finfer SR, Lipman J, Chapman M, Boyce NW (2002) Appropriateness of red blood cell transfusion in Australasian intensive care practice. Med J Aust 177:548–551
Rao MP, Boralessa H, Morgan C, Soni N, Goldhill DR, Brett SJ, Boralessa H, Contreras M (2002) Blood component use in critically ill patients. Anaesthesia 57:530–534
Engelfriet CP, Reesink HW, McCullough J, Hebert PC, McIntyre LA, Carson JL, Ferreira G, Thurer RL, Brock H, Boyce N, Jones J, Wulf H, Lukasewitz P, Kretschmer V, Walsh TS, McClelland B (2002) Perioperative triggers for red cell transfusions. Vox Sang 82:215–226
Walsh TS, McClelland DB (2003) When should we transfuse critically ill and perioperative patients with known coronary artery disease? Br J Anaesth 90:719–722
Hebert PCM (2000) The anemic patient in the intensive care unit: how much does the heart tolerate? Curr Opin Crit Care 6:372–380
Hebert PC, Yetisir E, Martin C, Blajchman MA, Wells G, Marshall J, Tweeddale M, Pagliarello G, Schweitzer I (2001) Is a low transfusion threshold safe in critically ill patients with cardiovascular diseases? Crit Care Med 29:227–234
Wu WC, Rathore SS, Wang Y, Radford MJ, Krumholz HM (2001) Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med 345:1230–1236
Rao SV, Jollis JG, Harrington RA, Granger CB, Newby LK, Armstrong PW, Moliterano DJ, Lindblad L, Pieper K, Topol EJ, Stamler JS, Califf RM (2004) Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 292:1555–1562
Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J (2002) Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol 39:1780–1786
Ezekowitz JA, McAlister FA, Armstrong PW (2003) Anemia is common in heart failure and is associated with poor outcomes: insights from a cohort of 12,065 patients with new-onset heart failure. Circulation 107:223–225
Nguyen BV, Bota DP, Melot C, Vincent JL (2003) Time course of hemoglobin concentrations in nonbleeding intensive care unit patients. Crit Care Med 31:406–410
von Ahsen NM, Muller CP, Serke SM, Frei UM, Eckardt K-UM (2001) Important role of nondiagnostic blood loss and blunted erythropoietic response in the anemia of medical intensive care patients. Crit Care Med [Suppl] 29:S150
Andrews T, Waterman H, Hillier V (1999) Blood gas analysis: a study of blood loss in intensive care. J Adv.Nurs 30:851–857
Corwin HL, Parsonnet KC, Gettinger A (1995) RBC transfusion in the ICU. Is there a reason? Chest 108:767–771
Rogiers P, Zhang H, Leeman M, Nagler J, Neels H, Melot C, Vincent JL (1997) Erythropoietin response is blunted in critically ill patients. Int Care Med 23:159–162
Krafte-Jacobs B (1997) Anemia of critical illness and erythropoietin deficiency. Int Care Med 23:137–138
van Iperen CE, Gaillard CA, Kraaijenhagen RJ, Braam BG, Marx JJ, van de WA (2000) Response of erythropoiesis and iron metabolism to recombinant human erythropoietin in intensive care unit patients. Crit Care Med 28:2773–2778
Rodriguez RM, Corwin HL, Gettinger A, Corwin MJ, Gubler D, Pearl RG (2001) Nutritional deficiencies and blunted erythropoietin response as causes of the anemia of critical illness. J Crit Care 16:36–41
Krafte-Jacobs B, Levetown ML, Bray GL, Ruttimann UE, Pollack MM (1994) Erythropoietin response to critical illness. Crit Care Med 22:821–826
Saleh E, McArdle F, Lee RJ, McClleland DBL, Walsh TS (2003) Prevalence of anaemia among survivors of critical illness managed with conservative transfusion triggers: a single centre cohort study. Br J Anaesth 90:819P
Obrador GT, Pereira BJ (2002) Anaemia of chronic kidney disease: an under-recognized and under-treated problem. Nephrol Dial Transplant 17 [Suppl 11]:44–46
Caro JJ, Salas M, Ward A, Goss G (2001) Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review. Cancer 91:2214–2221
Fallowfield L, Gagnon D, Zagari M, Cella D, Bresnahan B, Littlewood TJ, McNulty P, Gorzegno G, Freund M (2002) Multivariate regression analyses of data from a randomised, double-blind, placebo-controlled study confirm quality of life benefit of epoetin alfa in patients receiving non-platinum chemotherapy. Br J Cancer 87:1341–1353
Littlewood TJ, Bajetta E, Nortier JW, Vercammen E, Rapoport B (2001) Effects of epoetin alfa on hematologic parameters and quality of life in cancer patients receiving nonplatinum chemotherapy: results of a randomized, double-blind, placebo-controlled trial. J Clin Oncol 19:2865–2874
Barany P, Pettersson E, Konarski-Svensson JK (1993) Long-term effects on quality of life in haemodialysis patients of correction of anaemia with erythropoietin. Nephrol Dial Transplant 8:426–432
Seidenfeld J, Piper M, Aronson N (2002) Systematic review of controlled trials on erythropoietin to support evidence-based guidelines. Oncology (Huntingt) 16:171–188
Herridge MS (2002) Long-term outcomes after critical illness. Curr Opin Crit Care 8:331–336
Eddleston JM, White P, Guthrie E (2000) Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med 28:2293–2299
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Shapiro MJ, Corwin MJ, Colton T (2002) Efficacy of recombinant human erythropoietin in critically ill patients: a randomized controlled trial. JAMA 288:2827–2835
Acknowledgements
The ATICS study was supported by the Scottish Intensive Care Society and the Scottish National Blood Transfusion Service. The Scottish Intensive Care Society provided facilities for the collection and analysis of the ICU demographic and outcome data through the Scottish Intensive Care Society Audit Group. The Scottish National Blood Transfusion Service seconded a study coordinator to the study from the Effective Use of Blood Group. The study received unrestricted sponsorship from Ortho Biotech, which was managed through the Transfusion Medicine Education and Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors represent the Audit of Transfusion in Intensive Care in Scotland (ATICS) study group. The ATICS Study Group was made up of the organizing committee: T.S. Walsh (Chairman), M. Garrioch, C. Maciver (study coordinator), F. McArdle (study coordinator), J. Kinsella, R. Lee (statistician), G. Fletcher, D.B. McClelland, R. Green, A. Todd and F. MacKirdy and of the participating units: Aberdeen Royal Infirmary (S.A. Stott, J.L. Scott, M.G.K. Strachan); Borders General Hospital (T. Cripps, S. Hogg, D. Hedderly, L. Hume, J. Playfair, I. Gourlay); Glasgow Royal Infirmary (J. Kinsella, M.G. Booth, T. McMillan); Ninewells Hospital Dundee (S.L. Crofts, I. Mellor, S.J. Cole); Royal Alexandra Hospital Paisley (G. Fletcher, K. McIlravey); Royal Infirmary, Edinburgh (T.S. Walsh, F. McArdle, S.J. Dodds); Southern General Hospital, Glasgow (M. Garrioch, J. Sandbach, B. McMillan); St John’s Hospital, Livingston (M. Hughes, M. MacRury, L.M.M. Morrison); Western General Hospital, Edinburgh (C. Wallis, C.G. Battison, C. Hardcastle, E.D. Fox); Western Infirmary, Glasgow (A.R. Binning, M. Pollock, S. Kelly); Scottish National Blood Transfusion Service (D.B. McClelland, R.H.A. Green, A.M.M. Todd, I. McKechnie, C.R. Maciver); Scottish Intensive Care Society Audit Group (F. MacKirdy); Clinical Audit Resource Centre, Western General Hospital, Edinburgh (M.L. Hughes); Medical Statistics Unit, Edinburgh University (R.J. Lee).
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Walsh, T.S., Lee, R.J., Maciver, C.R. et al. Anemia during and at discharge from intensive care: the impact of restrictive blood transfusion practice. Intensive Care Med 32, 100–109 (2006). https://doi.org/10.1007/s00134-005-2855-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2855-2