Abstract
Background
In the last decades, many community-based studies have addressed predictors of nursing home placement (NHP) among the elderly. So far, predictors have not been analyzed separately for different age groups.
Methods
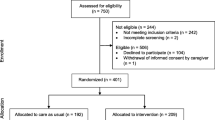
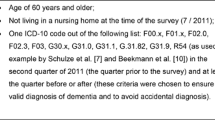
For a German GP-sample of 3,208 subjects aged 75 years and older, socio-demographic, clinical, and psychometric parameters were requested every 1.5 years over three waves. Logistic regression models determined predictors of NHP for total sample and for two different age groups. A CART analysis identified factors discriminating best between institutionalized and non-institutionalized individuals.
Results
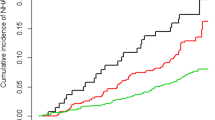
Of the overall sample, 4.7% of the sample (n = 150) was institutionalized during the study period. Baseline characteristics associated with a higher risk of NHP for the total sample were age, living without spouse, cognitive and functional impairment and depression. In the CART analysis, age was the major discriminator at the first level (at age 81). In subgroup regression analyses, for the younger elderly (age 75–81) being single as well as cognitive and functional impairment increased the risk of NHP; in the advanced elderly (age 82+) being widowed and subjective memory impairment were significant predictors for NHP, and cognitive and functional impairment became non-significant as predictors of NHP.
Conclusions
Predictors of NHP may differ in old age groups. The fact that many predictors show inconsistent results as predictors of NHP in the international literature may be attributed to the lack of differentiation in age groups.


Similar content being viewed by others
References
Kinsella K, Velkoff VA (2001) An aging world: 2001. International Population Reports. Washington DC: US Bureau of Census, US Government Printing Office
Channon A, Matthews Z, Van Lerberghe W (2006) Will there be enough people to care? Notes on the workforce implications of demographic change 2005–2050? Background paper prepared for The world health report 2006: working together for health. World Health Organization
Wancata J, Musalek M, Alexandrowicz R, Krautgartner M (2003) Number of dementia sufferers in Europe between the years 2000 and 2050. Eur Psychiatry 18:306–313
Federal Statistical Office (2007) Pflegestatistik 2005—Pflege im Rahmen der Pflegeversicherung—Deutschlandergebnisse. Statistisches Bundesamt, Wiesbaden
Gaugler JE, Duval S, Anderson KA, Kane RL (2007) Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr 7:13
Luppa M, Luck T, Brähler E, König H-H, Riedel-Heller SG (2008) Prediction of institutionalisation in dementia—a systematic review. Dement Geriatr Cogn Disord 26:65–78
Luppa M, Luck T, Weyerer S, König H-H, Brähler E, Riedel-Heller SG (2010) Prediction of institutionalisation in the elderly. A systematic review. Age Ageing 39:31–38
Wingard DL, Jones DW, Kaplan RM (1987) Institutional care utilization by the elderly: a critical review. Gerontologist 27:156–163
Chenier MC (1987) Review and analysis of caregiver burden and nursing home placement. Geriatr Nurs 18:121–126
Zaudig M, Hiller W (1996) SIDAM-Handbuch Strukturiertes Interview für die Diagnose einer Demenz vom Alzheimer Typ, der Multiinfarkt- (oder vaskulären) Demenz und Demenzen anderer Ätiologie nach DSM-III-R, DSM-IV, ICD-10. Verlag Hans Huber, Bern
Folstein MF, Folstein SE, McHugh PR (1965) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Luck T, Zaudig M, Wiese B, Riedel-Heller SG (2007) SIDAM: age- and education-specific reference values for the cognitive test section according to the new CASMIN Educational Classification. Z Gerontopsychol Psychiatr 20:31–38
Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, Mellits ED, Clark C (1989) The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 39:1159–1165
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Sheikh JI, Yesavage JA (1986) Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version. Clinical Gerontologist 5:165–173
Gauggel S, Birkner B (1999) Validity and reliability of a German version of the Geriatric Depression Scale (GDS). Z Klin Psychol Forschung Praxis 28:18–27
Breiman L, Friedman JH, Olshen RA, Stone CJ (1984) Classification and regression trees. Wadsworth, Belmont
Brauns H, Steinmann S (1999) Educational reform in France, West-Germany and the United Kingdom. ZUMA-Nachr 44:7–44
Harris Y (2007) Depression as a risk factor for nursing home admission among older individuals. J Am Med Dir Assoc 8:14–20
Aguero-Torres H, von Strauss E, Viitanen M, Winblad B, Fratiglioni L (2004) Institutionalization in the elderly: the role of chronic diseases and dementia. Cross-sectional and longitudinal data from a population-based study. J Clin Epidemiol 54:795–801
Woo J, Ho SC, Yu AL, Lau J (2000) An estimate of long-term care needs and identification of risk factors for institutionalization among Hong Kong Chinese aged 70 years and over. J Gerontol A Biol Sci Med Sci 55:M64–M69
Miller EA, Weissert WG (2000) Predicting elderly people’s risk for nursing home placement, hospitalization, functional impairment, and mortality: a synthesis. Med Care Res Rev 57:259–297
Gaugler JE, Yu F, Krichbaum K, Wyman JF (2009) Predictors of nursing home admission for persons with dementia. Medical Care 47:191–198
Riedel-Heller SG, Busse A, Aurich C, Matschinger H, Angermeyer MC (2001) Prevalence of dementia according to DSM-III-R and ICD-10: results of the Leipzig Longitudinal Study of the Aged (LEILA75+) Part 1. Br J Psychiatry 179:250–254
Jagger C, Gillies C, Moscone F, Cambois E, van Oyen H, Nusselder W, Robine JM (2008) Inequalities in healthy life years in the 25 countries of the European Union in 2005: a cross-national meta-regression analysis. Lancet 372:2124–2131
Acknowledgments
This publication is part of the German Research Network on Dementia (KND) and the German Research Network on Degenerative Dementia (KNDD) and was funded by the German Federal Ministry of Education and Research; Grant Number: 01GI0102, 01GI0420, 01GI0422, 01GI0423, 01GI0429, 01GI0431, 01GI0433, 01GI0434, O1GI0710, 01GI0711, 01GI0712, 01GI0713, 01GI0714, 01GI0715, 01GI0716.
Conflict of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Further members of the AgeCoDe group: Heinz-Harald Abholz, Matthias C. Angermeyer, Cadja Bachmann, Wolfgang Blank, Mirjam Colditz, Moritz Daerr, Sandra Eifflaender-Gorfer, Angela Fuchs, Frank Jessen, Sven Heinrich, Hanna Kaduszkiewicz, Teresa Kaufeler, Manfred Mayer, Julia Olbrich, Heinz-Peter Romberg, Anja Rudolph, Martina Schäufele, Sandra Schmitz, Britta Schürmann, Janine Stein, Michael Wagner.
Rights and permissions
About this article
Cite this article
Luppa, M., Riedel-Heller, S.G., Luck, T. et al. Age-related predictors of institutionalization: results of the German study on ageing, cognition and dementia in primary care patients (AgeCoDe). Soc Psychiatry Psychiatr Epidemiol 47, 263–270 (2012). https://doi.org/10.1007/s00127-010-0333-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0333-9