Abstract
Aims/hypothesis
We aimed to examine whether individuals with initial omission of glucose-lowering drug treatment (GLDT), including those achieving initial remission of type 2 diabetes, may experience a higher risk of major adverse cardiovascular events (MACE) compared with well-controlled individuals on GLDT after a new type 2 diabetes diagnosis in real-world clinical practice. Furthermore, we examined whether a higher risk could be related to lower initiation of statins and renin–angiotensin system inhibitors (RASi).
Methods
In this cohort study, we used Danish registers to identify individuals with a first measured HbA1c between 48 and 57 mmol/mol (6.5–7.4%) from 2014 to 2020. Six months later, we divided participants into four groups according to GLDT and achieved HbA1c (<48 vs ≥48 mmol/mol [6.5%]): well-controlled and poorly controlled on GLDT; remission and persistent type 2 diabetes not on GLDT. We reported how much the standardised 5 year risk of MACE could be reduced for each group if initiation of statins and RASi was the same as in the well-controlled group on GLDT.
Results
We included 14,221 individuals. Compared with well-controlled participants on GLDT, the 5 year standardised risk of MACE was higher in the three other exposure groups: by 3.3% (95% CI 1.6, 5.1) in the persistent type 2 diabetes group not on GLDT; 2.0% (95% CI 0.4, 3.7) in the remission group not on GLDT; and 3.5% (95% CI 1.3, 5.7) in the poorly controlled group on GLDT. Fewer individuals not on GLDT initiated statins and RASi compared with individuals on GLDT. If initiation of statins and RASi had been the same as in the well-controlled group on GLDT, participants not on GLDT could have reduced their risk of MACE by 2.1% (95% CI 1.2, 2.9) in the persistent type 2 diabetes group and by 1.1% (95% CI 0.4, 1.9) in the remission group.
Conclusions/interpretation
Compared with well-controlled individuals on GLDT, individuals not on initial GLDT had a higher 5 year risk of MACE, even among those achieving remission of type 2 diabetes. This may be related to lower use of statins and RASi.
Graphical Abstract

Similar content being viewed by others

Avoid common mistakes on your manuscript.

Introduction
Type 2 diabetes is a progressive disease with an increased risk of cardiovascular morbidity [1]. Yet, little is known about the relationship between remission of type 2 diabetes and risk of cardiovascular events in real-world clinical practice. One English observational study found that remission was associated with a reduction of cardiovascular events among individuals with prevalent type 2 diabetes registered by primary care codes [2]. However, the likelihood of initial remission of type 2 diabetes and the associated risk of cardiovascular events remains to be examined among newly diagnosed individuals identified from routine HbA1c measurements (≥48 mmol/mol [6.5%]). In accordance with guidelines presented by the ADA and the EASD [3], Danish guidelines allow a 6 month trial period of lifestyle modifications (diet and physical activity) prior to initiation of glucose-lowering drug treatment (GLDT) for individuals with an initial HbA1c level below 58 mmol/mol (<7.5%) [4, 5]. These recommendations combined with the access to routine HbA1c measurements from Danish registers provide a unique setting to investigate the influence of a possible initial conservative lifestyle strategy without GLDT.
A diagnosis of type 2 diabetes gives rise to new treatment targets of LDL-cholesterol and blood pressure, preferably with renin–angiotensin system inhibitors (RASi) [4,5,6]. Nonetheless, an initial conservative trial period of lifestyle modifications to achieve glycaemic control could lead to less aggressive risk factor management with statins and RASi. Thus, in a real-world usual care setting, individuals with remission or GLDT delay could have a higher risk of cardiovascular events compared with individuals initiating early effective GLDT. To reflect Danish guidelines, we examined the extent of GLDT delay and type 2 diabetes remission 6 months after a first measured HbA1c between 48 and 57 mmol/mol (6.5–7.4%). Further, we examined whether these individuals may experience a higher risk of first-time cardiovascular events. As a secondary objective, we aimed to examine whether a higher risk could be mediated by lower initiation of statins and RASi. Hence, we aimed to test whether a reduction in risk of major adverse cardiovascular events (MACE) could be expected among individuals omitting initial GLDT if they had been as likely to receive initial treatment with statins and RASi as well-controlled individuals on GLDT (i.e. an indirect interventional effect).
Methods
Setting
In Denmark, the majority of patients with type 2 diabetes are managed in primary care. Since the WHO endorsed HbA1c in the diagnostic criteria of diabetes (≥48 mmol/mol [6.5%]) in 2011 [7], HbA1c measurements have been the main diagnostic method in Denmark [8].
Data sources
All Danish residents are assigned a unique personal civil registration number, which allows cross-linkage of routinely collected individual-level data from the Danish nationwide administrative registers. In this cohort study, we obtained data from the following registers: (1) the Danish Civil Registration System, which holds data on date of birth, sex, ethnicity, migration, vital status and cohabitation status for all individuals residing in Denmark [9]; (2) the Danish National Patient Register [10]; (3) the Danish National Prescription Register, which holds data on redeemed prescriptions [11]; (4) the Danish Income Statistics Register [12]; (5) the Danish Population Education Register [13]. All these registers have previously been described [14]. Further, we also obtained information from the Danish Nationwide Register of Laboratory Results for Research, which holds systematic laboratory measurements from general practitioners, outpatient clinics and hospitalised patients in four out of five administrative regions in Denmark from 2014 onwards, coded according to the Nomenclature for Properties and Units (NPU) codes and local analysis numbers [15].
Study population
We identified Danish residents who had a first-time HbA1c measurement ≥48 mmol/mol (6.5%), from 1 January 2014 to 31 December 2020. We included individuals aged 40 to 80 years at the date of first measurement of HbA1c≥48 mmol/mol. Of these individuals, we included only those presenting with an HbA1c level of 48–57 mmol/mol (6.5–7.4%). We excluded individuals with a prior redeemed prescription of any glucose-lowering drug (Anatomical Therapeutic Chemical [ATC] code: A10; https://www.whocc.no/atc_ddd_index/) or a prior primary discharge code of diabetes (ICD-8 codes: 249–250; ICD-10 codes: E10–E14, O24.0–O24.3, O24.5–O24.9 or H36.0; http://apps.who.int/classifications/icd10/browse/2016/en). Further, we excluded individuals with conditions in which HbA1c is not appropriate for diagnosis of diabetes, including eGFR <30 ml/min per 1.73 m2 and moderate anaemia (haemoglobin <6.83 mmol/l) (see Fig. 1 for other criteria and electronic supplementary material [ESM] Tables 1, 2 for definitions). Moreover, we excluded individuals already on statins or RASi within 180 days prior to first measured HbA1c≥48 mmol/mol (6.5%).
Flow chart of the study population. aEnd-stage renal disease or eGFR<30 ml/min per 1.73 m2: n=1035; severe liver disease or splenomegaly: n=296; haemolytic anaemia, haemoglobinopathies, moderate anaemia, iron deficiency or B12 deficiency: n=3671; alcoholism: n=1362; severe hypertriglyceridaemia or severe hyperbilirubinaemia: n=49; and intake of specific drugs: n=643. CABG, coronary artery bypass graft surgery; IHD, ischaemic heart disease; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; T2D, type 2 diabetes
In order to reflect the Danish recommendation of a possible 6 month trial period of lifestyle modifications [4, 5], we started the follow-up time for cardiovascular events 180 days after date of first measured HbA1c≥48 mmol/mol (6.5%) (i.e. the index date). As we aimed to investigate primary prevention outcomes, we included only individuals without prior registered ischaemic heart disease, stroke or peripheral artery disease at the index date. Individuals who did not initiate GLDT prior to the index date were included only if they had a second HbA1c measurement recorded prior to index, while individuals who initiated GLDT prior to the index date were included only if they had a post-GLDT HbA1c measurement recorded prior to index.
Exposure
Initiation of GLDT was defined as at least one redeemed prescription (ATC code: A10). At index (180 days after first measured HbA1c≥48 mmol/mol [6.5%]), we divided participants into four exposure groups according to initiation of GLDT and most recently measured HbA1c level: (1) well-controlled (HbA1c<48 mmol/mol) on GLDT; (2) poorly controlled (HbA1c≥48 mmol/mol) on GLDT; (3) remission (HbA1c<48 mmol/mol) not on GLDT; (4) persistent type 2 diabetes (HbA1c≥48 mmol/mol) not on GLDT. For individuals initiating GLDT, we only used HbA1c measurements obtained after initiation of GLDT.
Outcomes
The primary outcome was first-time MACE, defined as the first occurrence of myocardial infarction, stroke or all-cause death (see ESM Table 1 for ICD-10 codes). The diagnoses for myocardial infarction and stroke have a high validity (positive predictive values: myocardial infarction, 92.4–100%; stroke, 80.5–97.0%) [10, 16]. We examined initiation of statins and RASi in relation to exposure and MACE as described in the Statistical analyses section. Initiation of statins and RASi was defined as at least one redeemed prescription within the exposure window between the first measured HbA1c≥48 mmol/mol (6.5%) and the index date.
Characteristics of the study population
Baseline medication was defined as a redeemed prescription within the period of 180 days prior to index date (see ESM Table 2 for ATC codes). Comorbidities were defined from discharge codes within the 10 years prior to index and/or by use of condition-specific medications (ESM Table 1). We obtained the most recent measurements of haemoglobin, LDL-cholesterol and creatinine within a 180 day period prior to date of first measured HbA1c≥48 mmol/mol (6.5%). eGFR was calculated from the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (see ESM Table 3 for NPU codes) [17].
Statistical analyses
Patient characteristics at index date were summarised according to the four exposure groups, where continuous variables were presented as medians with IQRs and categorical variables as counts with percentages. We described the time-dynamic distribution of the individuals across exposure groups every 30 days during the 180 day period between the date of first measured HbA1c≥48 mmol/mol (6.5%) and the index date. We reported the proportions of the exposure groups who initiated statins and RASi treatment, respectively, before the index date. In addition, we reported the achieved post-index 1 year level of LDL-cholesterol according to the four exposure groups.
All participants were followed from the index date until date of MACE, emigration or end of study (31 January 2022), whichever came first. We used the Aalen–Johansen method to estimate the proportions of participants who had initiated statins and RASi, respectively, within 1 year after index, while accounting for MACE as a competing risk [18]. We used the stratified Kaplan–Meier method to estimate the crude 5 year absolute risks of MACE in the four exposure groups.
First, we aimed to examine the standardised absolute 5 year risk of MACE according to the four exposure groups using the observed within-group propensity of initiation of statins and RASi (total effect) [19]. Second, we aimed to estimate the indirect stochastic interventional effect (mediation effect) through initiation of statins and RASi in the three other exposure groups by setting the use of statins and RASi according to the observed propensity in the well-controlled group on GLDT. This method is similar to the methods suggested by Vanderweele et al and Rudolph et al [20, 21]. A minor variation is that we standardised to the whole population, in order to obtain estimates with a clinically relevant interpretation. We used logistic regression to model the propensity of initiation of statins and RASi, respectively, until the index date, separately in each exposure group. We used Cox regression to model the hazard rate of MACE in all participants according to exposure groups. In the Cox regression model, to avoid generalising the effects from other exposure groups, we allowed the effects of statins and RASi to vary between exposure groups by including an exposure × mediator interaction term. We further assumed consistency, positivity, conditional exchangeability (no uncontrolled exposure–outcome confounding, mediator–outcome confounding, or exposure–mediator confounding) and no intermediate confounders [19]. All regression models were adjusted for: age (5 year categories), sex, cohabitation status, income, ethnicity (Danish or immigrants/descendants); type of requester of first HbA1c measurement (general practitioner or other); value of first measured HbA1c (48–52 mmol/mol [6.5–6.9%] or 53–57 mmol/mol [7.0–7.4%]); eGFR prior to first HbA1c≥48 mmol/mol (6.5%); and history of comorbidities (heart failure, atrial fibrillation, chronic pulmonary obstructive disease and cancer).
Based on the Cox regression model and the observed characteristics of each participant, by setting the exposure level to each of the four given exposure levels by turn for each participant and by random assignment of treatment values of statins and RASi according to the modelled propensities, we predicted the absolute 5 year risks of MACE according to each exposure level for all participants [22]. We repeated the random treatment assignment 200 times and averaged the predicted risk estimates, in order to report the standardised absolute 5 year risk of MACE. First, we estimated the standardised absolute 5 year risk of MACE according to exposure and the observed propensity of statins and RASi in each of the four exposure groups. Second, for each of the three other exposure groups than the well-controlled group on GLDT, we estimated the indirect interventional effect of initiation of statins and RASi as the average standardised absolute 5 year MACE risk differences between setting treatment of statins and RASi according to the observed within-group propensity and the propensity in the well-controlled group on GLDT. The 95% CIs were obtained as quantiles of 1000 bootstrap samples obtained by resampling from the population of all included individuals.
Further, we report the separate indirect interventional effects (mediation effects) of statins and RASi. We also repeated the analysis of indirect interventional effects of the combined use of statins and RASi after excluding individuals with hypertension prior to first measured HbA1c≥48 mmol/mol. We also repeated the analyses in subgroups of sex and age (40–64, 65–80 years) and for the total population, replacing 180 days as index with 365 days. We defined the level of statistical significance as 5%, conducted all analyses in R, version 4.0.3, and used the riskRegression R package [23, 24].
Ethics
In Denmark, register-based studies do not require ethical approval or informed consent by law. Permission to use data has been granted by the Knowledge Centre on Data Protection Compliance–the Capital Region of Denmark (approval number: P-2019-191).
Results
Characteristics of the study population
The final study population comprised 14,221 individuals with a first measured HbA1c of 48–57 mmol/mol (6.5–7.4%) (Fig. 1). The distribution of GLDT and most recent HbA1c level every 30 days during the first 180 days after first HbA1c≥48 mmol/mol (6.5%) are shown in ESM Fig. 1. The proportion of individuals receiving GLDT stabilised after 120 days, while the proportion of individuals with a follow-up HbA1c measurement increased steadily over time. Hence, the distribution of exposure groups was as follows after 180 days (date of index): well-controlled on GLDT: 22.3%; poorly controlled on GLDT: 14.7%; remission not on GLDT: 38.3%; and persistent type 2 diabetes not on GLDT: 24.7%. Baseline characteristics differed according to initial GLDT and initial glycaemic control (Table 1). Regardless of initial glycaemic control, individuals on GLDT were slightly younger and had higher levels of first measured HbA1c and eGFR than individuals not on GLDT. Regardless of GLDT, well-controlled/remitted individuals were more likely to be female, had higher income and educational level, and were less likely to live alone compared with the respective poorly controlled/persistent type 2 diabetes group on/not on GLDT. Compared with other groups, the well-controlled group on GLDT had fewer comorbidities. The majority of individuals on GLDT received metformin. No differences in LDL-cholesterol were observed between exposure groups. A similar pattern of baseline characteristics was observed according to exposure groups defined after 365 days (ESM Table 4).
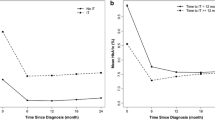
Five year risk of MACE according to initial GLDT and glycaemic control
During 52,006 person-years, 1351 individuals had a first-time MACE (stroke: 243, myocardial infarction: 161, all-cause death: 947). Well-controlled individuals on GLDT had the lowest unadjusted absolute 5 year risk of MACE compared with the three other exposure groups (Fig. 2a). After standardisation, the well-controlled group on GLDT remained with the lowest 5 year risk of MACE (Fig. 2b). Thus, compared with the well-controlled group on GLDT, the absolute standardised 5 year risk of MACE was 3.3% (95% CI 1.6, 5.1) higher in the group with persistent type 2 diabetes not on GLDT; 2.0% (95% CI 0.4, 3.7) higher in the remission group not on GLDT; and 3.5% (95% CI 1.3, 5.7) higher in the poorly controlled group on GLDT (Fig. 2b).
Crude (a) and standardised (b) absolute 5 year risk of first-time MACE according to initial GLDT and glycaemic control, 180 days after first measured HbA1c≥48 mmol/mol (6.5%). Time zero denotes 180 days after first measured HbA1c≥48 mmol/mol. Standardised to the distribution of all included individuals with respect to the distribution of age, sex, cohabitation status, ethnicity, income, type of requester (general practitioner or other), first measured HbA1c level, eGFR, comorbidities, and after setting the use of statins and RASi as observed for each exposure group for all individuals. T2D, type 2 diabetes
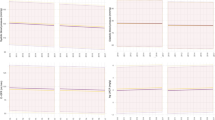
Differences in initiation of statins and RASi according to initial GLDT and glycaemic control
Both groups omitting initial GLDT had lower probabilities of treatment with statins and RASi compared with individual on GLDT (Fig. 3). These differences were consistent in subgroups of age and sex (ESM Figs 2, 3). Moreover, the treatment differences with statins and RASi remained 1 year after index (ESM Table 5, ESM Fig. 4). The proportion of individuals achieving a 1 year LDL-cholesterol level below 1.8 mmol/l was around 26% among both groups on GLDT and around 11–12% among both groups not on GLDT (ESM Table 6). The proportion of individuals with missing follow-up LDL-cholesterol measurements was higher among individuals not on initial GLDT.
Expected absolute reduction of 5 year risk of MACE if each exposure group had the same probability of receiving statins and RASi as the well-controlled group on GLDT
Figure 4 shows the absolute reduction of standardised risk of MACE that, hypothetically, could be expected for each exposure group if they had been as likely to receive initial treatment with statins and RASi as observed in the well-controlled group on GLDT. For both groups not on initial GLDT, this equalisation of initial treatment with statins and RASi could significantly reduce the standardised 5 year risk of MACE: by 2.1% (95% CI 1.2, 2.9) in the group with persistent type 2 diabetes and by 1.1% (95% CI 0.4, 1.9) in the remission group (Fig. 4). In separate analyses, equalising treatment with statins alone significantly changed the risk in both groups not on GLDT, whereas equalising treatment with RASi alone changed the risk significantly only in the group with persistent type 2 diabetes (Fig. 4). Of note, equalising treatment with both statins and RASi in the poorly controlled group on GLDT did not change the risk of MACE, as the observed probabilities of statins and RASi were almost identical as in the well-controlled group on GLDT (Fig. 4).
Expected absolute reduction of standardised 5 year risk of MACE if each exposure group had the same probability of receiving statins and/or RASi as the well-controlled group on GLDT. Depicted is the absolute reduction of standardised 5 year risk of MACE for each exposure group that could be expected if they, hypothetically, were as likely to receive treatment with statins and/or RASi as the well-controlled group on GLDT. The reduction of risk was calculated for each exposure group as the difference between the risk with the observed use of statins and/or RASi (observed risk) and the risk if treatment had been the same as the well-controlled group on GLDT (risk under intervention). The use of dashes for the well-controlled group on GLDT indicates that the observed risk and risk under intervention were identical for this specific group. T2D, type 2 diabetes
Sensitivity analyses
Exclusion of individuals with hypertension prior to first measured HbA1c≥48 mmol/mol (6.5%) did not change our results (data not shown). Our results according to exposure were consistent across sex and age groups, yet with broad 95% CI limits (ESM Figs 2, 3, 5, 6). In sensitivity analyses, in which we defined the four exposure groups after 365 days instead of 180 days, the results were consistent with the main findings from this study (ESM Figs 7–9). Thus, regardless of achieved glycaemic control, individuals not on GLDT had lower probabilities of initiation of statins and RASi compared with individuals on GLDT (ESM Fig. 8). If the probabilities of treatment with statins and RASi had been the same as in the well-controlled group on GLDT, the excess absolute risk of 5 year MACE could be reduced by 2.6% (95% CI 1.6, 3.5) in the group with persistent type 2 diabetes not on GLDT and by 1.4% (95% CI 0.6, 2.1) in the remission group not on GLDT (ESM Fig. 9).
Discussion
In a real-world setting of individuals with a first-time HbA1c measurement above the diagnostic threshold of type 2 diabetes, we found a higher absolute 5 year risk of first-time MACE in individuals omitting initial GLDT as compared with well-controlled individuals on GLDT, regardless of having persistent type 2 diabetes or initial remission of type 2 diabetes. Further, individuals with initial omission of GLDT received markedly less treatment with statins and RASi. We showed that a significant part of the higher risk of MACE may be related to lower use of statins and RASi. These findings suggest that more attention could be given to risk-modifying treatment with statins and RASi among lifestyle-treated individuals without initial GLDT and underscore the disadvantages of a threshold-based, glucose-centred cardiovascular prevention strategy in real-world clinical practice.
One American and one English study found low rates of remission (2.8 and 9.7 per 1000 person-years) among individuals with prevalent type 2 diabetes [25, 26]. However, in support of our findings of type 2 diabetes remission as a common event after an initial type 2 diabetes diagnosis, they found relatively high remission rates among subgroups with low baseline HbA1c, no prior GLDT and short duration of type 2 diabetes [25, 26]. The evidence of a link between remission of type 2 diabetes and cardiovascular events is even more scarce. One study found an association between remission of type 2 diabetes and reduction of cardiovascular events [2]. These results were observed among individuals with prevalent type 2 diabetes identified from codes in primary care and are not generalisable to our study of new-onset type 2 diabetes identified from routine HbA1c measurements. Moreover, the beneficial effects could be attributable to more intensive underlying lifestyle modifications than in our study or their choice of using the entire spectrum of type 2 diabetes as a reference group. Contrary to their study, we also examined whether individuals achieving remission could have had a better prognosis if they had been treated with statins and RASi as for individuals on GLDT. Thus, assuming that participants on GLDT were a heterogeneous group with regard to health behaviour, we also divided participants on GLDT into groups according to achieved HbA1c and used the well-controlled group as a reference. Furthermore, we did not choose a very strict definition of remission, as we aimed to include spontaneous remission cases to reflect real-world decision making and the associated risk connected to undertreatment. This definition was almost in line with the recent consensus statement which defined remission as a single HbA1c measurement below 48 mmol/mol (6.5%) 6 months after initiation of lifestyle modifications [27].
Remission may occur either spontaneously (i.e. weight loss due to illness or emotional distress, or by chance) or through lifestyle interventions [27]. As we aimed to include both spontaneous and intentional cases to reflect real-world clinical practice, lifestyle intervention studies may yield more favourable results than ours. Yet, only one randomised trial, the Look Action for Health in Diabetes (Look AHEAD) trial, has evaluated the effects of intensive lifestyle interventions (physical activity and diet) on cardiovascular outcomes [28]. The researchers did not report cardiovascular efficacy in overweight or obese individuals [28], in spite of increased remission rates [29]. The Diabetes Remission Clinical Trial (DiRECT) was not designed to evaluate cardiovascular outcomes, but showed sustained remission at 24 months for more than a third undergoing a very-low-calorie/energy diet [30]. Both DiRECT and the Look AHEAD trial reported lower use of cardiovascular medication in the intervention group [28, 30]. Consequently, although levels of systolic blood pressure and triglycerides were lower in the intervention group in both trials, total cholesterol or LDL-cholesterol levels were elevated and may have contributed to the lack of cardiovascular effects in the Look AHEAD trial [28, 30,31,32]. These results are consistent with prior evidence suggesting that weight reduction programmes typically show greater reductions in triglyceride levels with more modest reductions in total cholesterol and LDL-cholesterol [33]. Lifestyle interventions with sufficient intensity to prevent cardiovascular outcomes may only be achievable in a subset of individuals.
Our findings suggest that individuals with initial remission shortly after diagnosis remain at high risk. Identification of individuals at high cardiovascular risk is the cornerstone in prevention efforts, since the higher the absolute cardiovascular risk, the higher the absolute benefit of risk factor treatment [34]. Strong evidence shows that lowering of LDL-cholesterol reduces cardiovascular risk in many different types of individuals, regardless of presenting cholesterol level [35, 36]. Further, based on a recent large individual participant-level data meta-analysis, it has been suggested that initiation of antihypertensive treatment may be based on an individual’s risk rather than relying on blood pressure values [37]. Moreover, guidelines recommend inclusion of RASi in treatment of hypertension in type 2 diabetes, with strong evidence in the presence of albuminuria or proteinuria and some evidence in the absence of kidney disease [4,5,6, 38].
Our results indicated that an absolute risk reduction of MACE could be expected in both groups not on initial GLDT if they had been as likely to receive statins and RASi therapy as the well-controlled individuals on GLDT. The most prominent absolute risk reductions after equalisation of treatment were observed in the group with persistent type 2 diabetes (with the highest cardiovascular risk). As we allowed for exposure × mediator interaction in our Cox model, the slightly more conservative findings in the remission group could also in part arise from confounding by indication, as treated individuals may have had a higher prevalence of undetected cardiovascular risk factors such as smoking and blood pressure.
Another large Danish register-based cohort study found that an HbA1c just below the diagnostic threshold (46–47 mmol/mol [6.4–6.5%]) predicts the highest risk of MACE in individuals with a first measured HbA1c of 40–51 mmol/mol (5.8–6.8%) [39]. Further, these individuals received much less treatment with statins and RASi compared with individuals just above the threshold. Our study elaborates on these findings by also reporting an increased cardiovascular risk for individuals with remission after an initial HbA1c measurement above the diagnostic threshold of type 2 diabetes. Moreover, our results suggest that the increased use of statins and RASi associated with the more aggressive treatment targets after a diagnosis of type 2 diabetes mostly seems to extend to individuals treated with GLDT [4,5,6]. Further, our findings that lower use of statins and RASi may be connected to a large part of the excess risk of MACE in individuals omitting initial GLDT are in line with previous findings in prediabetes, which have shown that elevated cardiovascular risk is mostly attributable to established risk factors other than dysglycaemia [40,41,42].
We sought to examine real-world initiation patterns and risk of cardiovascular outcomes with respect to guidelines for a possible 6 month lifestyle modification period without GLDT. Therefore, we aimed to report the risk of MACE according to whether individuals had received GLDT and their achieved HbA1c level at a single time point, 180 days following their first diagnostic routine measurement of type 2 diabetes. Further, we examined whether differences in risk could be attributed to differences in initiation of statins and RASi. Notably, we did not aim to determine the effects of GLDT and glycaemic control, including the time-varying effects. Thus, we considered possible relapse of type 2 diabetes after initial remission as part of the causal path between initial remission and MACE in real-world clinical practice. Moreover, our findings with regard to glycaemic control should be carefully interpreted. Although our findings suggest that poorly controlled type 2 diabetes predicts higher cardiovascular risk, this could be attributed to a more severe variant of type 2 diabetes and/or less toleration of intensive GLDT.
Clinical implications
We report potential mediation effects of statins and RASi on average group level and not treatment effects. Our findings are hypothesis generating and suggest that conservative strategies in relation to glycaemic control may halt risk-modifying treatment with statins and RASi after an initial diagnosis of type 2 diabetes. Given that the timing of pharmacologic treatment to achieve LDL-cholesterol (at least <2.6 mmol/l) and blood pressure (<130/<80 mmHg) targets has not been clearly specified in Danish and European diabetes guidelines, a discussion of timing seems relevant [4,5,6].
Strengths and limitations
The major strengths of this study arise from the large amount of unselected individual data on routine HbA1c measurements, prescriptions, sociodemographic variables and diagnosis codes with high validity. However, there are also limitations of which we need to be aware.
First, although we adjusted for initial levels of HbA1c and eGFR and baseline comorbidities, we cannot eliminate the possibility of unmeasured confounding because we lacked information on several clinically important variables, including smoking, weight, diet, physical activity, duration of type 2 diabetes and blood pressure. In the two groups not on GLDT, unmeasured confounding may have led to a slight overestimation when setting the use of statins and RASi as observed in the well-controlled group on GLDT. However, as unmeasured confounders may be more often present in individuals on initial GLDT, unmeasured confounding may have biased the absolute risk estimates of MACE towards the null in the two groups not on GLDT. Likewise, we would expect unmeasured confounding by indication to bias the mediation effects of statins and RASi towards the null.
Second, we focused on initial treatment differences with statins and RASi. Yet, the differences in use of statins and RASi were maintained throughout follow-up and the restriction of initial treatment most likely contributed with estimates towards the null. Third, we cannot exclude that initiation of statins and RASi may also be surrogates for higher levels of health literacy and a more favourable underlying health, which might be linked to more intensive non-pharmacological interventions such as self-management education and lifestyle. As we allowed for exposure × mediator interaction, this may be especially present in the persistent type 2 diabetes group and could bias our results away from the null. However, confounding by indication would bias the results towards the null and a ‘healthy adherer effect’ was previously shown to be minimal compared with pharmacological drug use [43]. Fourth, we cannot determine whether the observed treatment differences were attributable to doctors not prescribing or patients not redeeming prescriptions. In addition, although we considered redeemed prescriptions as a valid proxy of treatment utilisation, we cannot exclude the possibility of misclassification. Regarding statins and RASi use, this misclassification may have been most apparent in the two groups omitting initial GLDT, leading to a possible bias towards the null. Fifth, although we would expect our findings to be more pronounced with longer follow-up, our findings obtained from relatively short follow-up may not be generalisable to long-term outcomes. Last, given the observational study design, our findings represent associations, and no causal conclusions can be drawn.
Conclusionss
Following a first-time HbA1c measurement above the diagnostic threshold of type 2 diabetes, a large group of individuals omitting initial GLDT had a higher absolute 5 year risk of first-time MACE compared with well-controlled individuals on GLDT. This was observed even for individuals achieving initial remission of type 2 diabetes without GLDT. A significant part of the excess risk of MACE appeared to be related to lower use of statins and RASi. This study supports the importance of considering early pharmacological primary prevention with statins and RASi in addition to lifestyle changes.
Abbreviations
- ATC:
-
Anatomical Therapeutic Chemical
- DiRECT:
-
Diabetes Remission Clinical Trial
- GLDT:
-
Glucose-lowering drug treatment
- Look AHEAD:
-
Look Action for Health in Diabetes
- MACE:
-
Major adverse cardiovascular events
- NPU:
-
Nomenclature for Properties and Units
- RASi:
-
Renin-angiotensin system inhibitors
References
Rawshani A, Rawshani A, Franzén S et al (2017) Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med 376:1407–1418. https://doi.org/10.1056/NEJMoa1608664
Hounkpatin H, Stuart B, Farmer A, Dambha-Miller H (2021) Association of type 2 diabetes remission and risk of cardiovascular disease in pre-defined subgroups. Endocrinol Diabetes Metab 4:e00280. https://doi.org/10.1002/edm2.280
Inzucchi SE, Bergenstal RM, Buse JB et al (2012) Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 55:1577–1596. https://doi.org/10.1007/s00125-012-2534-0
Danish Society for General Practice and Danish Endocrine Society (2014) Pharmacological treatment of type 2 diabetes - aims and algorithms 2014. Available from https://endocrinology.dk/PDF/FarmakologiskbehandlingDM2rev2014.pdf. Accessed 21 October 2022
Danish Society for General Practice and Danish Endocrine Society (2018) Pharmacological treatment of type 2 diabetes - aims and algorithms 2018. Available from https://vejledninger.dsam.dk/media/files/4/guidelines-2018-final.pdf. Accessed 21 October 2022
Cosentino F, Grant PJ, Aboyans V et al (2020) 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 41:255–323. https://doi.org/10.1093/eurheartj/ehz486
World Health Organization (2011) Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. Available from https://apps.who.int/iris/bitstream/handle/10665/70523/WHO_NMH_CHP_CPM_11.1_eng.pdf. Accessed 19 December 2022
Klinisk vejledning for almen praksis. Dansk selskab for Almen Medicin (2012) Type 2 diabetes - et metabolisk syndrom. Available from https://vejledninger.dsam.dk/media/files/4/type-2-diabetes-2012-med-links.pdf. Accessed 19 December 2022
Schmidt M, Pedersen L, Sørensen HT (2014) The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 29:541–549. https://doi.org/10.1007/s10654-014-9930-3
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/CLEP.S91125
Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M (2017) Data resource profile: the Danish national prescription registry. Int J Epidemiol 46:798–798f. https://doi.org/10.1093/ije/dyw213
Baadsgaard M, Quitzau J (2011) Danish registers on personal income and transfer payments. Scand J Public Health 39:103–105. https://doi.org/10.1177/1403494811405098
Jensen VM, Rasmussen AW (2011) Danish education registers. Scand J Public Health 39:91–94. https://doi.org/10.1177/1403494810394715
Falkentoft AC, Andersen J, Malik ME et al (2022) Impact of socioeconomic position on initiation of SGLT-2 inhibitors or GLP-1 receptor agonists in patients with type 2 diabetes - a Danish nationwide observational study. Lancet Reg Health Eur 14:100308. https://doi.org/10.1016/j.lanepe.2022.100308
Arendt JFH, Hansen AT, Ladefoged SA, Sørensen HT, Pedersen L, Adelborg K (2020) Existing data sources in clinical epidemiology: laboratory information system databases in Denmark. Clin Epidemiol 12:469–475. https://doi.org/10.2147/CLEP.S245060
Sundbøll J, Adelborg K, Munch T et al (2016) Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ open 6:e012832. https://doi.org/10.1136/bmjopen-2016-012832
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Int Med 150:604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Aalen OO, Johansen S (1978) An empirical transition matrix for nonhomogeneous Markov chains based on censored observations. Scand J Stat 5:141–150
Nguyen TQ, Schmid I, Stuart EA (2020) Clarifying causal mediation analysis for the applied researcher: defining effects based on what we want to learn. Psychol Methods 26(2):255–271. https://doi.org/10.1037/met0000299
Vanderweele TJ, Vansteelandt S, Robins JM (2014) Effect decomposition in the presence of an exposure-induced mediator-outcome confounder. Epidemiology 25:300–306. https://doi.org/10.1097/EDE.0000000000000034
Rudolph KE, Sofrygin O, Zheng W, van der Laan MJ (2018) Robust and flexible estimation of stochastic mediation effects: a proposed method and example in a randomized trial setting. Epidemiol Methods 7(1):20170007. https://doi.org/10.1515/em-2017-0007
Ozenne BMH, Scheike TH, Staerk L, Gerds TA (2020) On the estimation of average treatment effects with right-censored time to event outcome and competing risks. Biom J 62:751–763. https://doi.org/10.1002/bimj.201800298
R Core Team (2022) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available from https://www.R-project.org/. Accessed 21 December 2022
Gerds T, Ohlendorff J, Ozenne B (2023) riskRegression: risk regression models and prediction scores for survival analysis with competing risks. R package version 2023.03.22. Available from https://CRAN.R-project.org/package=riskRegression. Accessed 02 May 2023
Karter AJ, Nundy S, Parker MM, Moffet HH, Huang ES (2014) Incidence of remission in adults with type 2 diabetes: the diabetes & aging study. Diabetes Care 37:3188–3195. https://doi.org/10.2337/dc14-0874
Holman N, Wild SH, Khunti K et al (2022) Incidence and characteristics of remission of type 2 diabetes in England: a cohort study using the national diabetes audit. Diabetes Care 45:1151–1161. https://doi.org/10.2337/dc21-2136
Riddle MC, Cefalu WT, Evans PH et al (2021) Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetes Care 44:2438–2444. https://doi.org/10.2337/dci21-0034
Wing RR, Bolin P, Brancati FL et al (2013) Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 369:145–154. https://doi.org/10.1056/NEJMoa1212914
Gregg EW, Chen H, Wagenknecht LE et al (2012) Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 308:2489–2496. https://doi.org/10.1001/jama.2012.67929
Lean MEJ, Leslie WS, Barnes AC et al (2019) Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol 7:344–355. https://doi.org/10.1016/S2213-8587(19)30068-3
Lean ME, Leslie WS, Barnes AC et al (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391:541–551. https://doi.org/10.1016/S0140-6736(17)33102-1
Redmon JB, Bertoni AG, Connelly S et al (2010) Effect of the look AHEAD study intervention on medication use and related cost to treat cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care 33:1153–1158. https://doi.org/10.2337/dc09-2090
Pi-Sunyer FX, Becker DM, Bouchard C et al (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr 68(4):899–917. https://doi.org/10.1093/ajcn/68.4.899
Visseren FLJ, Mach F, Smulders YM et al (2022) 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol 29:5–115. https://doi.org/10.1093/eurjpc/zwab154
Collins R, Reith C, Emberson J et al (2016) Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 388:2532–2561. https://doi.org/10.1016/S0140-6736(16)31357-5
Ference BA, Ginsberg HN, Graham I et al (2017) Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J 38:2459–2472. https://doi.org/10.1093/eurheartj/ehx144
(2021) Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 397:1625–1636. https://doi.org/10.1016/S0140-6736(21)00590-0
Thomopoulos C, Parati G, Zanchetti A (2017) Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10 - should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J Hypertens 35:922–944. https://doi.org/10.1097/HJH.0000000000001276
Yahyavi SK, Snorgaard O, Knop FK et al (2021) Prediabetes defined by first measured HbA1c predicts higher cardiovascular risk compared with HbA1c in the diabetes range: a cohort study of nationwide registries. Diabetes Care 44:2767–2774. https://doi.org/10.2337/dc21-1062
Preiss D, Thomas LE, Sun JL et al (2012) Predictors of cardiovascular events in a contemporary population with impaired glucose tolerance: an observational analysis of the Nateglinide and Valsartan in impaired glucose tolerance outcomes research (NAVIGATOR) trial. BMJ open 2:e001925. https://doi.org/10.1136/bmjopen-2012-001925
Vistisen D, Witte DR, Brunner EJ et al (2018) Risk of cardiovascular disease and death in individuals with prediabetes defined by different criteria: the Whitehall II study. Diabetes Care 41:899–906. https://doi.org/10.2337/dc17-2530
Welsh C, Welsh P, Celis-Morales CA et al (2020) Glycated hemoglobin, prediabetes, and the links to cardiovascular disease: data from UK biobank. Diabetes Care 43:440–445. https://doi.org/10.2337/dc19-1683
Rasmussen JN, Chong A, Alter DA (2007) Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 297:177–186. https://doi.org/10.1001/jama.297.2.177
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
Some of the data were presented as an abstract at the European Society of Cardiology (ESC) Congress 2022 in Barcelona.
Data availability
The highly protected servers of Statistics Denmark hold the data used for this study. Danish data protection laws do not allow sharing of these data.
Funding
Open access funding provided by Zealand Region. The lead investigator ACF has received funding by an unrestricted Research Grant from Steno Diabetes Center Sjaelland for the conduct of the current study. The funder had no role in the study design, data analyses, data interpretation or drafting of the manuscript.
Authors’ relationships and activities
FKK has served on scientific advisory panels and/or been part of speaker’s bureaus for, or served as a consultant to and/or received research support from 89bio, AstraZeneca, Bayer, Boehringer Ingelheim, Dawn Health, Eli Lilly, Gubra, Novo Nordisk, Pharmacosmos, Sanofi, Structure Therapeutics, Zealand Pharma and Zucara not related to the current study; and is a minority shareholder in Antag Therapeutics ApS and co-owner of Medicinsk Vægttab ApS. LK reports speaker’s fees from AstraZeneca, Bayer, Boehringer Ingelheim, Novartis and Novo Nordisk not related to the current study. CT-P has received grants for studies from Bayer and Novo Nordisk not related to the current study. MS reports speaker’s fees from Novo Nordisk, AstraZeneca, Novartis and Boehringer Ingelheim unrelated to the current work. NEB has received investigator-initiated grants from the Novo Nordisk Foundation, the Augustinus Foundation, the Kaj Hansen Foundation and Health Insurance Denmark unrelated to the current work. A-CR reports speaker’s fees from Novartis, AstraZeneca and BMS unrelated to the current study. The authors declare that there are no other relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
All authors have made substantial contributions to the conception or design of the current study, acquisition of data or analysis and interpretation of data. ACF drafted the manuscript. All authors critically revised the manuscript and approved the final version of the manuscript. ACF is the guarantor of this work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Falkentoft, A.C., Gerds, T.A., Zareini, B. et al. Risk of first-time major cardiovascular event among individuals with newly diagnosed type 2 diabetes: data from Danish registers. Diabetologia 66, 2017–2029 (2023). https://doi.org/10.1007/s00125-023-05977-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-05977-6