Abstract
Despite enormous progress in managing blood glucose levels, pregnancy in women with type 1 diabetes still carries risks for the growing fetus. While, previously, fetal undergrowth was not uncommon in these women, with improved maternal glycaemic control we now see an increased prevalence of fetal overgrowth. Besides short-term implications, offspring of women with type 1 diabetes are more likely to become obese and to develop diabetes and features of the metabolic syndrome. Here, we argue that the increase in birthweight is paradoxically related to improved glycaemic control in the pre- and periconceptional periods. Good glycaemic control reduces the prevalence of microangiopathy and improves placentation in early pregnancy, which may lead to unimpeded fetal nutrition. Even mild maternal hyperglycaemia may then later result in fetal overnutrition. This notion is supported by circumstantial evidence that lower HbA1c levels as well as increases in markers of placental size and function in early pregnancy are associated with large-for-gestational age neonates. We also emphasise that neonates with normal birthweight can have excessive fat deposition. This may occur when poor placentation leads to initial fetal undergrowth, followed by fetal overnutrition due to maternal hyperglycaemia. Thus, the complex interaction of glucose levels during different periods of pregnancy ultimately determines the risk of adiposity, which can occur in fetuses with both normal and elevated birthweight. Prevention of fetal adiposity calls for revised goal setting to enable pregnant women to maintain blood glucose levels that are closer to normal. This could be supported by continuous glucose monitoring throughout pregnancy and appropriate maternal gestational weight gain. Future research should consider the measurement of adiposity in neonates.
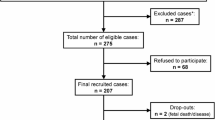
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
The incidence of type 1 diabetes is rising worldwide, in particular in younger adults [1]. This implies that there is an increasing number of pregnant women with type 1 diabetes. Indeed, in Canada and Scotland, the incidence of pregnancies complicated by diabetes has reportedly increased during the past 15 years [2, 3]. Up to the 1970s, medical attention focused on reducing the rate of congenital malformations and stillbirths. Despite enormous progress in maternal glycaemic control over the past few decades, pregnancies in women with type 1 diabetes still carry manifold maternal and fetal risks. While reduced in frequency, complications in both early pregnancy (e.g. congenital malformations) and late pregnancy (e.g. preeclampsia, preterm labour and stillbirth) are still more prevalent in women with type 1 diabetes than in those without diabetes [4].
In addition, fetal growth is affected in pregnancies with type 1 diabetes. Up to the 1970s the majority of fetuses showed overgrowth, with signs of excessive fat accumulation, but some fetuses grew at a lower rate and showed signs of growth restriction [5]. In more recent decades a paradoxical trend has been observed: neonates born to women with type 1 diabetes increasingly show overgrowth despite improved maternal glycaemic control [6]. A continuous increase in the proportion of large-for-gestational-age (LGA) neonates was found between 1992 and 2013 in Scotland [3] and between 1982 and 2007 in Sweden [7, 8]. The proportion of small-for-gestational-age (SGA) neonates born to women with type 1 diabetes remained stable at around 3–4% up to 2010 in Denmark [9, 10], with a small increase to 6–7% in the last 10 years [11]. In a recent large multicentre trial, rates of LGA offspring were 62–65% and of SGA offspring were 1–2%, depending which growth chart was used [12].
The shift to a higher incidence of fetal overgrowth has short-term implications, such as increased risks of shoulder dystocia, birth trauma and operative delivery [13]. Fetal overgrowth is often based on birthweight and can be defined as a neonate being LGA. However, in diabetes, overgrowth in fetuses actually relates mostly to excessive fat deposition at various anatomical locations [14, 15]. Therefore, fetal overgrowth manifests not only in neonates with increased birthweight, but also in those with normal birthweight [16]. In addition, the concentrations of leptin in the cord blood, presumably derived from fetal adipose tissue, are higher in neonates with overgrowth [17]. In the long-term, offspring of women with type 1 diabetes are more likely to become obese and have increased risks of developing type 2 diabetes, cardiovascular disease and other features of the metabolic syndrome, suggesting a programming role of the adverse intrauterine environment for these health problems [18,19,20]. Hence, it is important to avoid overgrowth of the fetus throughout pregnancy.
Poor glycaemic control over a longer period may lead to microangiopathy, expressed clinically as diabetic retinopathy and diabetic nephropathy. The presence of diabetic nephropathy in pregnancy is associated with a higher prevalence of SGA infants [9, 21]. Presumably, the presence of microangiopathy is likely to impair placental development and growth, which might be the underlying cause of restricted fetal growth. Reports indicate that the prevalence of nephropathy in pregnant women with type 1 diabetes has decreased in recent decades [9, 11].
In this review, we argue that the increase in birthweight is paradoxically related to the improvement in glycaemic control in the pre- and periconceptional periods over the past few decades. This argument is based on the concept that it is less common for women to experience severe hyperglycaemia and so subsequent processes in early pregnancy around placentation have become less and less affected and microangiopathy lesions of maternal vessels occur less frequently. The improved placentation leads to unimpeded fetal overnutrition as a result of the still present, but milder, maternal hyperglycaemia.
Determinants of birthweight
Birthweight is determined by the interplay of the genetic makeup of the fetus with macro- and micronutrients supplied by the mother and transferred through the placenta. Thus, the placenta plays an important role throughout pregnancy. In addition to providing nutrients to the fetus, it anchors the fetoplacental unit in maternal uterine tissues, mostly the decidua [22].
In pregnancy, decidual arteries supply the embryo and fetoplacental unit with oxygen and nutrients. In order to accomplish this task, the spiral arteries, that is, vessels that branch from the radial arteries in the myometrium, extending into the decidua, change their lumen to become high-capacity, low-resistance vessels (Fig. 1). This process of spiral artery transformation, or ‘remodelling’ of the spiral arteries, begins early in the first trimester of pregnancy and is critical for adequate oxygen and nutrient supply throughout pregnancy [23, 24].
The placenta is made up of a villous tree covered by a continuous cell layer (syncytiotrophoblast). Some villi (anchoring villi) attach to the decidua in the uterus of the pregnant woman (black rectangle in upper part of figure). At the tip of these villi, cytotrophoblasts are amassed. They invade the decidua to physically anchor the placenta in the uterine wall. They also invade uteroplacental (‘spiral’) arteries, where they aggregate to initially form cellular plugs, clogging the vessels. Up to about 8 weeks of pregnancy, only a filtrate of maternal blood with physically dissolved oxygen reaches the intervillous space. Thereafter, the cytotrophoblasts in the spiral arteries contribute to continuously remodel these arteries into high-capacity, low-resistance vessels. Loss of vascular smooth muscle cells leads to widening (opening) of the spiral arteries. As a result, cytotrophoblast plugs are removed, enabling fully oxygenated maternal blood to enter the intervillous space. This is paralleled by a rise in oxygen tension to which the fetoplacental unit is exposed. Each of the spiral arteries contributes to the overall oxygen supply of the fetoplacental unit. Inadequate or absent opening of the 100–150 spiral arteries reduces or inhibits blood flow. Depending on how many arteries are affected, and to what extent, the resulting reduced oxygen supply can ultimately reduce fetal growth. This figure is available as part of a downloadable slideset
Up to the 1970s, growth restriction, resulting in SGA neonates, was not an uncommon outcome of pregnancies in women with type 1 diabetes [5]. Chronic fetal hypoxia was often the underlying reason for the growth restriction [25]. Several processes contributed to the increased risk of fetal hypoxia in women with type 1 diabetes.
Type 1 diabetes was often accompanied by diabetic microangiopathy, mostly in individuals with longstanding and poorly controlled type 1 diabetes. When women became pregnant, these vasculopathies affected the uterine arteries, impairing remodelling of the uterine spiral arteries and, thus, reducing blood flow through these supply vessels [26]. This could cause problems with oxygen delivery to the fetoplacental unit and, in extreme cases, result in chronic fetal hypoxia and SGA neonates. In addition, decidual arteries often showed pathological changes, such as decidual vasculopathy in late pregnancy. Lesions in the decidual arteries, such as intramural fibrosis or signs of atherosis, were not uncommon in normotensive women with type 1 diabetes [27, 28], especially in women with diabetic microangiopathy [29]. Furthermore, atheromas in decidual arteries, with resultant elevated vascular resistance [30, 31], may have compounded the problem of diminished blood flow and oxygen supply.
The role of the pre- and periconceptional periods
Major advances in diabetes management in women with type 1 diabetes [32, 33] have resulted in pre- and periconceptional mean HbA1c levels decreasing from ≥59 mmol/mol (≥7.5%) in 1996–1999 [9] to 52 mmol/mol (6.9%) in 2012–2016 [33]. In addition, blood pressure control has been intensified over the same period. This may have resulted in reductions in the occurrence of decidual vasculopathy and spiral artery lesions. The prevalence of smoking, a well-known risk factor for SGA neonates, has also decreased in the past few decades in Europe and the USA [34]. This may also have contributed to better placentation in early pregnancy. Thus, through overall improved diabetes management and a reduction in smoking, the process of placentation has become near normal. This facilitates adequate oxygen delivery to the placental intervillous space, which reduces the risk of neonates being born growth restricted or SGA.
Measurements of first trimester concentrations of proteins related to placental size and function support the notion of improved placentation leading to LGA neonates in women with type 1 diabetes [35] (Fig. 2). Proteins used as markers of placentation include placental growth factor, A disintegrin and metalloproteinase 12, placental protein 13, placental growth hormone and pregnancy-associated plasma protein A. Their concentrations in the first trimester of pregnancy in women with diabetes were lower than in women without diabetes, suggesting poor placentation in diabetes. However, combined with the effect of hyperglycaemia, the neonates were born with appropriate for gestational age (AGA) birthweights. Women with diabetes, who had concentrations similar to those in women without diabetes, suggesting that they had ‘healthy’ placentas, gave birth to LGA neonates, again reflecting the contributing effect of hyperglycaemia [35]. Thus, improved placentation and placental function may be associated with a shift in birthweight distribution to higher birthweights and a reduced incidence of SGA neonates born to women with type 1 diabetes.
The effect of hyperglycaemia on birthweight category depends on early placental size and function, which can be monitored by biomarkers. An improvement in placentation and early placental function that interacts with hyperglycaemia throughout pregnancy can lead to increased birthweight of neonates born to women with type 1 diabetes. =, unaltered, in the normal range; AGA, appropriate for gestational age. This figure is available as part of a downloadable slideset
Why are more LGA babies born currently?
Early pregnancy events that may impair placentation and fetal oxygenation are not the only determinants of birthweight in pregnancies of women with type 1 diabetes. Despite improvements in glycaemic control in type 1 diabetes, maternal and fetal glucose levels are still elevated in both early and late pregnancy [36, 37] and not fully normalised to reflect the physiology of a healthy pregnancy. This is clearly seen in the elevated levels of insulin and C-peptide in cord blood in pregnancies of women with type 1 diabetes [38, 39]. Fetal hyperinsulinaemia stimulates fetal growth, which may result in LGA neonates (Fig. 3).
Various scenarios during pregnancy in women with type 1 diabetes showing how the interplay between early placentation and fetal overnutrition in the wake of elevated concentrations of maternal macronutrients can affect birthweight. Only extreme situations are depicted; more graded modifications are possible. The timing of fetal overnutrition in pregnancy (mostly glucose), as well as the genetic background of the fetus, may also play a role. The left side of the figure shows that long-term elevated blood glucose levels in the pre- and periconceptional periods, entailing microangiopathy, and at the time of placentation in early pregnancy may lead to impaired remodelling of spiral arteries, reduced placental blood flow and oxygen transfer. This poor placentation results in the birth of SGA neonates. If this is counteracted by maternal factors such as elevated glucose levels it may result in overnutrition of the fetus through the placenta, leading to fetal overgrowth. This will remain unrecognised if birthweight is the only outcome measure, as these neonates are born with a normal weight. The right side of the figure shows that, with near-normal blood glucose glycaemic levels in the pre- and periconceptional periods, placentation in early pregnancy will be almost normal, that is, with unimpaired or slightly impaired placental blood flow and oxygenation. In this situation, maternal factors such as normal glucose levels may result in normal fetal growth, leading to the birth of AGA neonates, whereas elevated glucose levels may result in overnutrition of the fetus through the placenta, leading to fetal overgrowth. This can manifest in the birth of LGA neonates. Thus, overnutrition can result in two phenotypes of overgrowth independent of birthweight (size of babies): in the presence of microangiopathy or poor placentation, birthweight will be low or normal; in their absence, birthweight will be normal or neonates will be LGA. In both instances, elevated maternal glucose concentrations lead to fetal hyperinsulinaemia and excessive fat deposition as characteristic features of overgrowth in these pregnancies. This figure is available as part of a downloadable slideset
However, fetal overnutrition may occur even in the case of AGA neonates. In cases of poor placentation with initially reduced fetal growth, hyperglycaemia later in pregnancy may result in neonates being born with an inconspicuous birthweight, that is, being AGA, which then also represents a phenotype of overgrowth with excessive fat deposition. This resembles the thin–fat phenotype in Asian populations, in which neonates are born with a ‘normal’ birthweight but with a disproportionately high body fat percentage compared with neonates from a white population [40] (Fig. 3). If placentation had been adequate, then later hyperglycaemia—even subtle—may have led to an LGA neonate. This distinction between overgrowth in AGA and LGA birthweight categories is important, because it helps explain the results seen for early placental markers and birthweight category [35].
The near-normalisation of decidual vascular health and placentation through improved glycaemic control in the pre-and periconceptional periods may have unmasked the potential for overgrowth in the wake of a still not fully normalised maternal metabolism. Hence, the effects of fetal ‘overnutrition’ as a result of elevated concentrations of maternal macronutrients, particularly glucose, become prominent, leading to more LGA neonates than in previous decades.
In the CONCEPTT trial, a large multicentre RCT of continuous glucose monitoring (CGM) in women with type 1 diabetes [37], women had a mean HbA1c level of 52 mmol/mol (6.9%) at baseline (around 10–11 gestational weeks). The LGA rate was 53% in women randomised to CGM and 69% in those randomised to routine capillary glucose monitoring. These LGA rates were higher than the LGA rate reported in the National Pregnancy in Diabetes UK audit, which was 46%, but early mean HbA1c was higher (60 mmol/mol [7.6%]) than in the CONCEPTT trial [41]. While these studies cannot be directly compared, they provide support for the relevance of early pregnancy blood glucose levels in determining birthweight. However, elevated blood glucose levels in the pre-and periconceptional period are not the only key factor. Rather, early blood glucose levels interact with the influence of glucose levels later in pregnancy to ultimately determine birthweight. The early and late pregnancy periods cannot be separated by a specific date in pregnancy, because the transition varies between pregnancies, depending on a variety of individual factors. Moreover, metabolically induced hyperinsulinaemia in the fetus is an important driver for increasing fetal fat deposition and, hence, contributes to increased birthweight and the overgrowth phenotype [42, 43]. Its onset may vary between individuals and can happen as early as the 14th gestational week [44].
The advance in knowledge over the last decade has enabled us to support earlier concepts about the complex interaction of early and later blood glucose levels and their effects on birthweight, biologically mediated by the quality of placentation in early pregnancy [35, 45]. The role of placental development is highlighted by analyses of a subcohort of the CONCEPTT trial that found higher birthweights in women with type 1 diabetes and suboptimal glucose control when placentas were ‘healthy’, as determined by placental growth factor, than when placentas were ‘unhealthy’ [46].
Insulin may play a contributing role, as seen in the association between the first trimester insulin dose in women with type 1 diabetes and birthweight, which is independent of glycaemic control. The higher the daily insulin dose needed to control glucose levels in the first trimester, the higher the birthweight [47]. Insulin doses in the second or third trimester were not associated with birthweight [47]. One hypothesis is that there is maternal insulin stimulation of early placental growth [48], which is associated with LGA offspring [49]. It remains to be studied whether these LGA neonates have more lean mass and fat mass or whether they represent the classical phenotype of overgrowth with increased fat mass but not lean mass accumulation.
The obesity pandemic has led to more women with type 1 diabetes entering their pregnancy with a pre-pregnancy BMI in the overweight or obese range [50, 51]. This can further exacerbate the risk of having an LGA infant [52]. The specific pathophysiological underpinnings are unclear but may involve maternal hyperglycaemia, because of obesity-associated insulin resistance, with subsequent early fetal hyperglycaemia and hyperinsulinaemia pulling more glucose to the fetus, the so-called glucose steal phenomenon [42]. Although the fetal glucose steal phenomenon has not yet been demonstrated in pregnancies with type 1 diabetes, it is mainly driven by fetal hyperinsulinaemia, which is also present in these pregnancies [38, 39]. However, multiple other pathways affecting birthweight have been proposed [53]. Although the daily insulin dose per unit body weight has not changed profoundly over the last few decades, the increase in body weight of pregnant women may have led to increases in absolute insulin doses, which in turn may have stimulated early placental growth with potential sequelae (see above).
Why should we avoid fetal overgrowth?
Fetal overgrowth has the potential for short-term complications [4], and the metabolic derangements, leading to excessive fat deposition, pose long-term risks to the offspring [43]. In more than 4800 mother–offspring pairs in the global Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) study, neonatal fat was positively associated with obesity in offspring at age 11 years [54]. Neonatal adiposity was the mediator between the altered intrauterine metabolic milieu and childhood obesity. This finding is important because individuals with a higher number of adipocytes at 2 years and older will have more adipocytes throughout their lifespan [55]. The higher number of ‘hungry’ adipocytes, destined to be filled with triacylglycerols, will then facilitate excessive fat deposition, thereby contributing to the long-term obesity risk [56]. Thus, fetal overgrowth with excessive fat accumulation in pregnancies with type 1 diabetes may lead to similar long-term consequences as in offspring born to women with gestational diabetes or type 2 diabetes or with obesity [18,19,20].
What can we do to prevent fetal overgrowth?
Achieving strict glycaemic control throughout pregnancy is mandatory to prevent inappropriate fetal growth. The effect of the in utero environment on fetal growth may be lessened by implementing a diabetes management plan to achieve glucose levels closer to physiological levels and also by considering daily fluctuations of glucose. However, the actual level of glucose needed to maintain growth without increased adiposity is currently unknown. CGM may improve glycaemic control by dampening fluctuations of glucose concentrations, thereby reducing the proportion of LGA neonates [37]. CGM seems to be more effective than the use of insulin pumps at achieving good glycaemic control, which surprisingly has not resulted in fewer LGA infants than multiple daily injections [57, 58]. However, CGM is a costly intervention and may not be available in all resource settings. Diet plans and weight management are less costly alternatives [4].
Maternal pre-pregnancy BMI and gestational weight gain play a role in fetal growth. In normal pregnancy [52], as well as in pregnancy in women with type 1 diabetes [36], excessive gestational weight gain is associated with higher fetal growth, determined by birthweight SD score, which is independent of glycaemic control. Pre-pregnancy and antenatal caregivers could advise women with overweight and obesity on weight management before and during pregnancy. Counselling interventions to improve adherence to healthy eating may be effective in reducing fetal overgrowth in pregnant women with type 2 diabetes [59], but their effect in pregnant women with type 1 diabetes needs to be elucidated in future studies.
Over the last few decades, people’s lifestyles have generally become more obesogenic, including frequent snacking and fewer home-cooked meals. This became even more evident during the lockdown periods of the COVID-19 pandemic [60]. Excessive carbohydrate intake is related to poorer glycaemic control in pregnant women with type 1 diabetes [61] and is associated with adverse pregnancy outcomes. These problems are often related to low socioeconomic status [62]. In addition, the strict glycaemic control regimen and frequent use of CGM and insulin pumps may make pregnant women with type 1 diabetes feel safe and tempt them to eat more [61]. Despite the therapeutic and medical improvements, often resulting in near-normalised blood glucose levels, efforts to motivate women to strictly adhere to their diet plan throughout pregnancy is still of utmost importance [4]. The recommended diet plan should include a sufficient intake of macro- and micronutrients with a minimum daily intake of 175 g carbohydrates with a low glycaemic index [63] and limit gestational weight gain [61].
Future directions
Clinical directions
Currently, women with type 1 diabetes have been shown to have fairly good glycaemic control in the periconceptional period, as determined by their HbA1c levels [64]. HbA1c is an appropriate measure of average blood glucose levels, but its suitability as a pregnancy outcome predictor in type 1 diabetes has been questioned [65]. Recently, evidence has been accumulating about the importance of monitoring temporal glucose profiles throughout pregnancy and of glucose levels being in the desired glycaemic range for as much time as possible to improve birth outcomes [66, 67]. This calls for revised goal setting to achieve glucose levels in the physiological range throughout pregnancy (see text box: Summary of future directions). Although CGM holds promise for achieving glucose levels close to physiological levels over 24 h periods during pregnancy [68], euglycaemia may still be difficult to achieve in pregnant women with type 1 diabetes [50]. It is hoped that more and more healthcare systems globally will financially support the use of CGM, similar to the recent approval of these technologies by the UK government.
Lowering BMI before pregnancy and limiting gestational weight gain during pregnancy are mandatory for women with overweight or obesity with type 1 diabetes. However, both reducing pre-pregnancy BMI and preventing excessive gestational weight gain may be challenging and difficult to achieve, despite lifestyle counselling.
Research directions
The early growth period of the fetus and how it is influenced by the maternal environment is an underexplored area. Recently established, well-phenotyped early pregnancy cohorts [69] will help to gain insight into factors that modify early embryonic and fetal growth in a variety of maternal settings. It is well known that the maternal diet in the pre- and periconceptional periods can influence the early growth of the embryo, fetus and placenta [70], but the effect of metabolic changes in the mother on the embryo and fetus is less well studied. Some influences of maternal type 1 diabetes on early placental development and function have been found [22, 71,72,73], but their consequences for fetal growth remain elusive. Despite feasibility issues, we suggest that future research should focus on the early pregnancy period during which placental growth trajectories such as size/volume and vascularisation are largely determined [74, 75]. Moreover, fetal hyperinsulinaemia, the key driver of fetal growth and fat accumulation in pregnancies complicated by diabetes, has its roots in early pregnancy [42]. Thus, the early pregnancy period has a strong influence on later fetal growth.
To date, human studies, including intervention studies, have focused on the proportion of LGA neonates born to women with type 1 diabetes. However, neonates with an inconspicuous birthweight can also show overgrowth as a result of their overnutrition in utero against the background of impaired placentation. These offspring constitute an important group for future obesity prevention efforts and should be of major public health concern. The birthweight-centric classification system of AGA/LGA does not capture excessive adiposity, but no alternative classification system is currently available. In the future, it will be important to expand study outcomes to include the number of fetuses with overgrowth with increased adiposity despite having a normal birthweight (see text box: Summary of future directions). This will require measurement of neonatal body composition, although this might be difficult to implement in routine clinical practice. While sophisticated techniques such as air displacement plethysmography (e.g. PEA POD, COSMED) or dual-energy x-ray absorptiometry may be preferred for measurement of body composition, measurement of skinfold thickness using callipers or other techniques can give adequate results that can be converted into body fat and have been widely used in large-scale studies [76]. Furthermore, studies should include measurement of a proxy indicator for placentation (biomarkers, uterine artery blood flow) in the early pregnancy period combined with quantification of blood glucose levels in the pregnant women throughout pregnancy. These exposures could then be related to the outcome of neonatal adiposity.
Summary and conclusion
The increase in birthweight over time reported in several populations of pregnant women with type 1 diabetes, despite improved glycaemic control, has been of concern. It has prompted the suggestion that, in addition to hyperglycaemia, other factors may account for this observation [51].
Our heuristic concept presented here provides an alternative explanation. We focus on improved placentation in early pregnancy in women with type 1 diabetes as the basis on which the growth-promoting effects of maternal hyperglycaemia later in pregnancy are superimposed. This concept posits that complex interactions of blood glucose levels at different stages of pregnancy ultimately determine birthweight or, more specifically, fetal overgrowth in pregnancies complicated by type 1 diabetes. This calls for more intensive efforts to bring glucose levels closer to the physiological range throughout pregnancy, and the use of modern diabetes technologies may help women to achieve this. Future research should focus on the placentation phase and onwards and include some form of neonatal adiposity measurement in addition to a birthweight-centred growth outcome.
Abbreviations
- AGA:
-
Appropriate for gestational age
- CGM:
-
Continuous glucose monitoring
- CONCEPTT:
-
Continuous Glucose Monitoring in Women with Type 1 Diabetes in Pregnancy Trial
- LGA:
-
Large for gestational age
- SGA:
-
Small for gestational age
References
Mobasseri M, Shirmohammadi M, Amiri T, Vahed N, Hosseini Fard H, Ghojazadeh M (2020) Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Health Promot Perspect 10(2):98–115. https://doi.org/10.34172/hpp.2020.18
Feig DS, Hwee J, Shah BR, Booth GL, Bierman AS, Lipscombe LL (2014) Trends in incidence of diabetes in pregnancy and serious perinatal outcomes: a large, population-based study in Ontario, Canada, 1996-2010. Diabetes Care 37(6):1590–1596. https://doi.org/10.2337/dc13-2717
Mackin ST, Nelson SM, Kerssens JJ et al (2018) Diabetes and pregnancy: national trends over a 15 year period. Diabetologia 61(5):1081–1088. https://doi.org/10.1007/s00125-017-4529-3
Ringholm L, Damm P, Mathiesen ER (2019) Improving pregnancy outcomes in women with diabetes mellitus: modern management. Nat Rev Endocrinol 15(7):406–416. https://doi.org/10.1038/s41574-019-0197-3
Pedersen JF, Molsted-Pedersen L (1979) Early growth retardation in diabetic pregnancy. Br Med J 1(6155):18–19. https://doi.org/10.1136/bmj.1.6155.18
Evers IM, de Valk HW, Mol BW, ter Braak EW, Visser GH (2002) Macrosomia despite good glycaemic control in Type I diabetic pregnancy; results of a nationwide study in The Netherlands. Diabetologia 45(11):1484–1489. https://doi.org/10.1007/s00125-002-0958-7
Persson M, Norman M, Hanson U (2009) Obstetric and perinatal outcomes in type 1 diabetic pregnancies: A large, population-based study. Diabetes Care 32(11):2005–2009. https://doi.org/10.2337/dc09-0656
Persson M, Pasupathy D, Hanson U, Norman M (2011) Birth size distribution in 3,705 infants born to mothers with type 1 diabetes: a population-based study. Diabetes Care 34(5):1145–1149. https://doi.org/10.2337/dc10-2406
Ekbom P, Damm P, Feldt-Rasmussen B, Feldt-Rasmussen U, Molvig J, Mathiesen ER (2001) Pregnancy outcome in type 1 diabetic women with microalbuminuria. Diabetes Care 24(10):1739–1744. https://doi.org/10.2337/diacare.24.10.1739
Nielsen LR, Damm P, Mathiesen ER (2009) Improved pregnancy outcome in type 1 diabetic women with microalbuminuria or diabetic nephropathy: effect of intensified antihypertensive therapy? Diabetes Care 32(1):38–44. https://doi.org/10.2337/dc08-1526
Do NC, Vestgaard M, Asbjornsdottir B et al (2021) Unchanged prevalence of preeclampsia after implementation of prophylactic aspirin for all pregnant women with preexisting diabetes: a prospective cohort study. Diabetes Care https://doi.org/10.2337/dc21-1182
Meek CL, Corcoy R, Asztalos E et al (2021) Which growth standards should be used to identify large- and small-for-gestational age infants of mothers with type 1 diabetes? A pre-specified analysis of the CONCEPTT trial. BMC Pregnancy Childbirth 21(1):96. https://doi.org/10.1186/s12884-021-03554-6
Secher AL, Bytoft B, Tabor A, Damm P, Mathiesen ER (2015) Fetal sonographic characteristics associated with shoulder dystocia in pregnancies of women with type 1 diabetes. Acta Obstet Gynecol Scand 94(10):1105–1111. https://doi.org/10.1111/aogs.12707
Logan KM, Gale C, Hyde MJ, Santhakumaran S, Modi N (2017) Diabetes in pregnancy and infant adiposity: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 102(1):F65–F72. https://doi.org/10.1136/archdischild-2015-309750
Greco P, Vimercati A, Hyett J et al (2003) The ultrasound assessment of adipose tissue deposition in fetuses of "well controlled" insulin-dependent diabetic pregnancies. Diabet Med 20(10):858–862. https://doi.org/10.1046/j.1464-5491.2003.01041.x
Catalano PM, Thomas A, Huston-Presley L, Amini SB (2003) Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol 189(6):1698–1704. https://doi.org/10.1016/s0002-9378(03)00828-7
Tapanainen P, Leinonen E, Ruokonen A, Knip M (2001) Leptin concentrations are elevated in newborn infants of diabetic mothers. Horm Res 55(4):185–190. https://doi.org/10.1159/000049993
Clausen TD, Mathiesen ER, Hansen T et al (2008) High prevalence of type 2 diabetes and pre-diabetes in adult offspring of women with gestational diabetes mellitus or type 1 diabetes: the role of intrauterine hyperglycemia. Diabetes Care 31(2):340–346. https://doi.org/10.2337/dc07-1596
Clausen TD, Mathiesen ER, Hansen T et al (2009) Overweight and the metabolic syndrome in adult offspring of women with diet-treated gestational diabetes mellitus or type 1 diabetes. J Clin Endocrinol Metab 94(7):2464–2470. https://doi.org/10.1210/jc.2009-0305
Vlachova Z, Bytoft B, Knorr S et al (2015) Increased metabolic risk in adolescent offspring of mothers with type 1 diabetes: the EPICOM study. Diabetologia 58(7):1454–1463. https://doi.org/10.1007/s00125-015-3589-5
Carr DB, Koontz GL, Gardella C et al (2006) Diabetic nephropathy in pregnancy: suboptimal hypertensive control associated with preterm delivery. Am J Hypertens 19(5):513–519. https://doi.org/10.1016/j.amjhyper.2005.12.010
Hoch D, Gauster M, Hauguel-de Mouzon S, Desoye G (2019) Diabesity-associated oxidative and inflammatory stress signalling in the early human placenta. Mol Aspects Med 66:21–30. https://doi.org/10.1016/j.mam.2018.11.002
Zhang P (2020) Decidual vasculopathy and spiral artery remodeling revisited II: relations to trophoblastic dependent and independent vascular transformation. J Matern Fetal Neonatal Med 35:395–401. https://doi.org/10.1080/14767058.2020.1718646
Burton GJ, Woods AW, Jauniaux E, Kingdom JC (2009) Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta 30(6):473–482. https://doi.org/10.1016/j.placenta.2009.02.009
Zur RL, Kingdom JC, Parks WT, Hobson SR (2020) The placental basis of fetal growth restriction. Obstet Gynecol Clin North Am 47(1):81–98. https://doi.org/10.1016/j.ogc.2019.10.008
Pietryga M, Brazert J, Wender-Ozegowska E, Biczysko R, Dubiel M, Gudmundsson S (2005) Abnormal uterine Doppler is related to vasculopathy in pregestational diabetes mellitus. Circulation 112(16):2496–2500. https://doi.org/10.1161/CIRCULATIONAHA.104.492843
Bjork O, Persson B, Stangenberg M, Vaclavinkova V (1984) Spiral artery lesions in relation to metabolic control in diabetes mellitus. Acta Obstet Gynecol Scand 63(2):123–127. https://doi.org/10.3109/00016348409154646
Kitzmiller JL, Watt N, Driscoll SG (1981) Decidual arteriopathy in hypertension and diabetes in pregnancy: immunofluorescent studies. Am J Obstet Gynecol 141(7):773–779. https://doi.org/10.1016/0002-9378(81)90703-1
Gutaj P, Wender-Ozegowska E (2016) Diagnosis and management of IUGR in pregnancy complicated by type 1 diabetes mellitus. Curr Diab Rep 16(5):39. https://doi.org/10.1007/s11892-016-0732-8
Barth WH Jr, Genest DR, Riley LE, Frigoletto FD Jr, Benacerraf BR, Greene MF (1996) Uterine arcuate artery Doppler and decidual microvascular pathology in pregnancies complicated by type I diabetes mellitus. Ultrasound Obstet Gynecol 8(2):98–103. https://doi.org/10.1046/j.1469-0705.1996.08020098.x
Alnaes-Katjavivi P, Lyall F, Roald B, Redman CW, Staff AC (2016) Acute atherosis in vacuum suction biopsies of decidua basalis: An evidence based research definition. Placenta 37:26–33. https://doi.org/10.1016/j.placenta.2015.10.020
Damm JA, Asbjornsdottir B, Callesen NF et al (2013) Diabetic nephropathy and microalbuminuria in pregnant women with type 1 and type 2 diabetes: prevalence, antihypertensive strategy, and pregnancy outcome. Diabetes Care 36(11):3489–3494. https://doi.org/10.2337/dc13-1031
Norgaard SK, Vestgaard MJ, Jorgensen IL et al (2018) Diastolic blood pressure is a potentially modifiable risk factor for preeclampsia in women with pre-existing diabetes. Diabetes Res Clin Pract 138:229–237. https://doi.org/10.1016/j.diabres.2018.02.014
Hansen AR, Akomolafe TO, McGalliard Z, Belle-Isle L, Zhang J (2018) Striving to meet healthy people 2020 objectives: trend analysis of maternal smoking. Public Health Rep 133(6):644–649. https://doi.org/10.1177/0033354918793120
Kuc S, Wortelboer EJ, Koster MP, de Valk HW, Schielen PC, Visser GH (2011) Prediction of macrosomia at birth in type-1 and 2 diabetic pregnancies with biomarkers of early placentation. BJOG 118(6):748–754. https://doi.org/10.1111/j.1471-0528.2011.02904.x
Secher AL, Parellada CB, Ringholm L, Asbjornsdottir B, Damm P, Mathiesen ER (2014) Higher gestational weight gain is associated with increasing offspring birth weight independent of maternal glycemic control in women with type 1 diabetes. Diabetes Care 37(10):2677–2684. https://doi.org/10.2337/dc14-0896
Feig DS, Donovan LE, Corcoy R et al (2017) Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet 390(10110):2347–2359. https://doi.org/10.1016/S0140-6736(17)32400-5
Sosenko IR, Kitzmiller JL, Loo SW, Blix P, Rubenstein AH, Gabbay KH (1979) The infant of the diabetic mother: correlation of increased cord C-peptide levels with macrosomia and hypoglycemia. N Engl J Med 301(16):859–862. https://doi.org/10.1056/NEJM197910183011603
Yamamoto JM, Corcoy R, Donovan LE et al (2019) Maternal glycaemic control and risk of neonatal hypoglycaemia in type 1 diabetes pregnancy: a secondary analysis of the CONCEPTT trial. Diabet Med 36(8):1046–1053. https://doi.org/10.1111/dme.13988
Yajnik CS, Fall CH, Coyaji KJ et al (2003) Neonatal anthropometry: the thin-fat Indian baby. The pune maternal nutrition study. Int J Obes Relat Metab Disord 27(2):173–180. https://doi.org/10.1038/sj.ijo.802219
Murphy HR, Bell R, Cartwright C et al (2017) Improved pregnancy outcomes in women with type 1 and type 2 diabetes but substantial clinic-to-clinic variations: a prospective nationwide study. Diabetologia 60(9):1668–1677. https://doi.org/10.1007/s00125-017-4314-3
Desoye G, Nolan CJ (2016) The fetal glucose steal: an underappreciated phenomenon in diabetic pregnancy. Diabetologia 59(6):1089–1094. https://doi.org/10.1007/s00125-016-3931-6
Desoye G, Herrera E (2021) Adipose tissue development and lipid metabolism in the human fetus: The 2020 perspective focusing on maternal diabetes and obesity. Prog Lipid Res 81:101082. https://doi.org/10.1016/j.plipres.2020.101082
Carpenter MW, Canick JA, Hogan JW, Shellum C, Somers M, Star JA (2001) Amniotic fluid insulin at 14-20 weeks’ gestation: association with later maternal glucose intolerance and birth macrosomia. Diabetes Care 24(7):1259–1263. https://doi.org/10.2337/diacare.24.7.1259
Glinianaia SV, Tennant PW, Bilous RW, Rankin J, Bell R (2012) HbA(1c) and birthweight in women with pre-conception type 1 and type 2 diabetes: a population-based cohort study. Diabetologia 55(12):3193–3203. https://doi.org/10.1007/s00125-012-2721-z
Bacon S, Burger D, Tailor M et al (2021) Can placental growth factors explain birthweight variation in offspring of women with type 1 diabetes? Diabetologia 64(7):1527–1537. https://doi.org/10.1007/s00125-021-05438-y
Garcia-Patterson A, Ovejero D, Minambres I et al (2020) Both glycaemic control and insulin dose during pregnancy in women with type 1 diabetes are associated with neonatal anthropometric measures and placental weight. Diabetes Metab Res Rev 36(5):e3300. https://doi.org/10.1002/dmrr.3300
O'Tierney-Ginn P, Presley L, Myers S, Catalano P (2015) Placental growth response to maternal insulin in early pregnancy. J Clin Endocrinol Metab 100(1):159–165. https://doi.org/10.1210/jc.2014-3281
Plasencia W, Akolekar R, Dagklis T, Veduta A, Nicolaides KH (2011) Placental volume at 11-13 weeks’ gestation in the prediction of birth weight percentile. Fetal Diagn Ther 30(1):23–28. https://doi.org/10.1159/000324318
Murphy HR (2018) Intensive glycemic treatment during type 1 diabetes pregnancy: a story of (mostly) sweet success! Diabetes Care 41(8):1563–1571. https://doi.org/10.2337/dci18-0001
McGrath RT, Glastras SJ, Hocking SL, Fulcher GR (2018) Large-for-gestational-age neonates in type 1 diabetes and pregnancy: contribution of factors beyond hyperglycemia. Diabetes Care 41(8):1821–1828. https://doi.org/10.2337/dc18-0551
Persson M, Pasupathy D, Hanson U, Westgren M, Norman M (2012) Pre-pregnancy body mass index and the risk of adverse outcome in type 1 diabetic pregnancies: a population-based cohort study. BMJ Open 2(1):e000601. https://doi.org/10.1136/bmjopen-2011-000601
Barbour LA, Hernandez TL (2018) Maternal Non-glycemic contributors to fetal growth in obesity and gestational diabetes: spotlight on lipids. Curr Diab Rep 18(6):37. https://doi.org/10.1007/s11892-018-1008-2
Josefson JL, Scholtens DM, Kuang A et al (2021) Newborn adiposity and cord blood C-peptide as mediators of the maternal metabolic environment and childhood adiposity. Diabetes Care 44(5):1194–1202. https://doi.org/10.2337/dc20-2398
Spalding KL, Arner E, Westermark PO et al (2008) Dynamics of fat cell turnover in humans. Nature 453(7196):783–787. https://doi.org/10.1038/nature06902
Muhlhausler B, Smith SR (2009) Early-life origins of metabolic dysfunction: role of the adipocyte. Trends Endocrinol Metab 20(2):51–57. https://doi.org/10.1016/j.tem.2008.10.006
Feig DS, Corcoy R, Donovan LE et al (2018) Pumps or multiple daily injections in pregnancy involving type 1 diabetes: a prespecified analysis of the CONCEPTT Randomized Trial. Diabetes Care 41(12):2471–2479. https://doi.org/10.2337/dc18-1437
Rys PM, Ludwig-Slomczynska AH, Cyganek K, Malecki MT (2018) Continuous subcutaneous insulin infusion vs multiple daily injections in pregnant women with type 1 diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials and observational studies. Eur J Endocrinol 178(5):545–563. https://doi.org/10.1530/EJE-17-0804
Asbjornsdottir B, Vestgaard M, Ringholm L et al (2019) Effect of motivational interviewing on gestational weight gain and fetal growth in pregnant women with type 2 diabetes. BMJ Open Diabetes Res Care 7(1):e000733. https://doi.org/10.1136/bmjdrc-2019-000733
Ammar A, Brach M, Trabelsi K et al (2020) Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 International online survey. Nutrients 12(6):1583. https://doi.org/10.3390/nu12061583
Asbjornsdottir B, Akueson CE, Ronneby H et al (2017) The influence of carbohydrate consumption on glycemic control in pregnant women with type 1 diabetes. Diabetes Res Clin Pract 127:97–104. https://doi.org/10.1016/j.diabres.2016.12.012
Murphy HR, Howgate C, O'Keefe J et al (2021) Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: a 5-year national population-based cohort study. Lancet Diabetes Endocrinol 9(3):153–164. https://doi.org/10.1016/S2213-8587(20)30406-X
Roskjaer AB, Andersen JR, Ronneby H, Damm P, Mathiesen ER (2015) Dietary advices on carbohydrate intake for pregnant women with type 1 diabetes. J Matern Fetal Neonatal Med 28(2):229–233. https://doi.org/10.3109/14767058.2014.906577
Mathiesen ER, Ali N, Anastasiou E et al (2021) Characteristics of pregnant women with diabetes using injectable glucose-lowering drugs in the EVOLVE study. J Matern Fetal Neonatal Med 28:1–9. https://doi.org/10.1080/14767058.2021.1940132
Kerssen A, Evers IM, de Valk HW, Visser GH (2003) Poor glucose control in women with type 1 diabetes mellitus and ‘safe’ hemoglobin A1c values in the first trimester of pregnancy. J Matern Fetal Neonatal Med 13(5):309–313. https://doi.org/10.1080/jmf.13.5.309.313
Murphy HR, Rayman G, Lewis K et al (2008) Effectiveness of continuous glucose monitoring in pregnant women with diabetes: randomised clinical trial. BMJ 337:a1680. https://doi.org/10.1136/bmj.a1680
Scott EM, Feig DS, Murphy HR, Law GR, Group CC (2020) Continuous glucose monitoring in pregnancy: importance of analyzing temporal profiles to understand clinical outcomes. Diabetes Care 43(6):1178–1184. https://doi.org/10.2337/dc19-2527
Yamamoto JM, Murphy HR (2021) Benefits of real-time continuous glucose monitoring in pregnancy. Diabetes Technol Ther 23(S1):S8–S14. https://doi.org/10.1089/dia.2020.0667
Rousian M, Schoenmakers S, Eggink AJ et al (2021) Cohort profile update: the Rotterdam periconceptional cohort and embryonic and fetal measurements using 3D ultrasound and virtual reality techniques. Int J Epidemiol https://doi.org/10.1093/ije/dyab030
Reijnders IF, Mulders A, van der Windt M, Steegers EAP, Steegers-Theunissen RPM (2019) The impact of periconceptional maternal lifestyle on clinical features and biomarkers of placental development and function: a systematic review. Hum Reprod Update 25(1):72–94. https://doi.org/10.1093/humupd/dmy037
Desoye G (2018) The human placenta in diabetes and obesity: friend or foe? The 2017 Norbert Freinkel Award Lecture. Diabetes Care 41(7):1362–1369. https://doi.org/10.2337/dci17-0045
Gauster M, Majali-Martinez A, Maninger S et al (2017) Maternal type 1 diabetes activates stress response in early placenta. Placenta 50:110–116. https://doi.org/10.1016/j.placenta.2017.01.118
Majali-Martinez A, Weiss-Fuchs U, Miedl H et al (2021) Type 1 diabetes mellitus and the first trimester placenta: hyperglycemia-induced effects on trophoblast proliferation, cell cycle regulators, and invasion. Int J Mol Sci 22(20):10989. https://doi.org/10.3390/ijms222010989
Desoye G, Hauguel-de Mouzon S (2007) The human placenta in gestational diabetes mellitus. The insulin and cytokine network. Diabetes Care 30(Suppl 2):S120–S126. https://doi.org/10.2337/dc07-s203
Bjork O, Persson B (1982) Placental changes in relation to the degree of metabolic control in diabetes mellitus. Placenta 3(4):367–378. https://doi.org/10.1016/s0143-4004(82)80030-1
van Poppel MNM, Simmons D, Devlieger R et al (2019) A reduction in sedentary behaviour in obese women during pregnancy reduces neonatal adiposity: the DALI randomised controlled trial. Diabetologia 62(6):915–925. https://doi.org/10.1007/s00125-019-4842-0
Acknowledgements
The authors want to thank D. S. Feig (Department of Medicine, University of Toronto, Toronto, ON, Canada), H. R. Murphy (Norwich Medical School, University of East Anglia, Norwich, UK) and G. H. Visser (Department of Obstetrics, University Medical Center, Utrecht University, Utrecht, the Netherlands) for inspiring discussions that eventually motivated this review article, and L. A. Barbour (Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine, University of Colorado School of Medicine, Aurora, CO, USA) for valuable input.
Authors’ relationships and activities
GD and ERM are members of the editorial board of Diabetologia. All other authors declare that there are no relationships or activities that might bias, or be perceived as bias, their contribution to this manuscript.
Contribution statement
GD designed the concept of the manuscript, wrote parts of the manuscript and designed the figures. He serves as guarantor and accepts full responsibility for the work. LR, PD and ERM discussed the concept and content, wrote parts of the manuscript and edited the manuscript. MNMvP discussed the concept and content, wrote parts of the manuscript and edited the text and figures. All authors approved the version to be published.
Funding
Open access funding provided by Medical University of Graz. GD was supported by a visiting professorship grant from the Danish Diabetes Academy, which is funded by the Novo Nordisk Foundation (grant number NNF17SA0031406). Work in GD’s laboratory is supported by the Oesterreichische Nationalbank (Anniversary Fund, project number 17950). The funders were not involved in the writing of the manuscript and did not impose any restrictions regarding its publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Slideset of figures
(PPTX 386 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Desoye, G., Ringholm, L., Damm, P. et al. Secular trend for increasing birthweight in offspring of pregnant women with type 1 diabetes: is improved placentation the reason?. Diabetologia 66, 33–43 (2023). https://doi.org/10.1007/s00125-022-05820-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05820-4