Abstract
Aims/hypothesis
This study aimed to investigate whether the effects of sleep duration interacted with the presence of diabetes. We specifically sought to examine the relationship between sleep duration and all-cause and cause-specific mortality in people with type 2 diabetes across sex, age at diagnosis, duration of diabetes and treatment type.
Methods
The sample consisted of 273,029 adults, including 248,817 without diabetes and 24,212 with type 2 diabetes, who participated in the National Health Interview Survey from 2004 to 2013 and whose data were linked to a mortality database up to 31 December 2015. Sleep duration was measured using self-report, whereby participants were asked ‘on average how long do you sleep each day (≤5, 6, 7, 8, 9 or ≥10 h/day)?’ The relationship between sleep duration and mortality risk was investigated using Cox proportional hazards regression model, with adjustments for demographics, BMI, lifestyle behaviours and clinical variables.
Results
Absolute mortality rate was higher in adults with diabetes and extremes of sleep duration (≤5 h/day, 215.0 per 10,000 person-years; ≥10 h/day, 363.5 per 10,000 person-years). There was a non-significant interaction between sleep duration and the presence of diabetes (p for interaction = 0.08). A J-shaped relationship existed between sleep duration and all-cause mortality risk in people with type 2 diabetes. Compared with the reference group (7 h/day), both shorter and longer sleep durations were associated with increased risk of all-cause mortality (≤5 h/day, HR 1.24 [95% CI 1.09, 1.40]; 6 h/day, HR 1.13 [1.01, 1.28]; 8 h/day, HR 1.17 [1.06, 1.30]; ≥10 h/day, HR 1.83 [1.61, 2.08]). Similar associations were also observed for mortality risk from CVD, cancer, kidney disease, Alzheimer’s disease and chronic lower respiratory diseases. Longer sleep duration in those with a younger age at diabetes onset was associated with greater risks of all-cause and CVD mortality. Shorter sleep duration in individuals treated with both insulin and oral glucose-lowering medication was also associated with higher risks of all-cause and CVD mortality.
Conclusions/interpretation
The associations between sleep duration and mortality risk may be different between diabetic and non-diabetic individuals. In people with type 2 diabetes, sleeping less or more than 7 h/day was associated with increased risk of all-cause and condition-specific mortality. The association was more prominent in those with a younger age at diabetes onset and receiving treatment with both oral glucose-lowering medication and insulin. This population may benefit from targeted sleep-related interventions to reduce the risks of adverse health outcomes.

Graphical abstract
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.

Introduction
Diabetes is a worldwide public health crisis. Globally, the prevalence of diabetes was 8.8% in 2017, affecting an estimated 424.9 million people [1]. This number is predicted to increase to 628.6 million by 2045 [1]. Diabetes was the seventh highest cause of premature death in 2016 [1] and is associated with an increased risk of all-cause mortality as well as condition-specific morbidity and mortality including CVD, cancer and kidney disease [2,3,4,5,6,7]. CVD is among the foremost diabetes-related causes of death [1, 8].
A recent study showed that death rates have obvious differences between people with diabetes and those without [9]. In addition, an earlier study found that there are weaker relative educational disparities in mortality among adults with vs those without diabetes [10]. The benefit from physical activity in individuals with CVD was shown to be greater than that in healthy individuals without CVD [11]. Mounting epidemiological evidence suggests that sleep duration is related to increased risks of CVD events and higher mortality risk in the general population [12,13,14,15,16]. However, no previous studies have compared the effect of sleep duration on mortality risk among participants with and without diabetes.
In addition, both insulin treatment and metformin therapy are associated with sleep duration and quality in individuals with type 2 diabetes [17, 18]. It is well established that individuals who experience short sleep duration and poor sleep quality have a higher risk of obesity, glucose intolerance, insulin resistance and poor glycaemic control, which would directly and indirectly affect outcomes among those with diabetes [19]. Moreover, studies have suggested that sex difference in the mortality rate associated with diabetes and age at onset of type 2 diabetes is a prognostically important determinant for survival outcomes [20, 21]. The role of sleep in this association remains unclear; although, it is biologically plausible that too little or too much sleep in people with type 2 diabetes would lead to poorer survival outcomes. Therefore, it is necessary to investigate the association of sleep duration with all-cause and disease-specific mortality in people with type 2 diabetes across the above subgroups.
Using data from the National Health Interview Survey (NHIS) in the USA, the aim of this study was to investigate whether the effect of sleep duration interacted with the presence of diabetes. We specifically sought to examine the relationship between sleep duration and all-cause and cause-specific mortality in people with type 2 diabetes across sex, age at diagnosis, duration of diabetes and treatment.
Methods
Participants
The NHIS is a nationally representative and multistage stratified survey of non-institutionalised individuals in the USA. In the survey, one adult and one child are selected randomly from each household for a detailed interview on health status and lifestyle behaviours. Details of the survey design and methods are displayed at the website of NHIS from National Center for Health Statistics (NCHS) (www.cdc.gov/nchs/nhis/about_nhis.htm; accessed 7 January 2018). NHIS was approved by the NCHS ethics review board. We could not influence the design of the prior studies upon which this work is based and cannot comment on individual ethics approval or consent. The data we used are publicly available and considered as exempt under the ethical board review of the corresponding author’s institution.
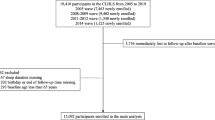
A total of 289,187 adults who participated in the NHIS from 2004 to 2013 were eligible to be linked to a mortality database over the follow-up period (up to 31 December 2015). After excluding missing data about sleep duration (n = 14,382), diabetes (n = 148), age at diagnosis of diabetes (n = 497) or use of oral glucose-lowering medication (n = 18) or insulin (n = 4), 274,138 remained. Among those with diabetes, we excluded individuals with possible type 1 diabetes (n = 1109), defined by use of insulin and age at diabetes onset <30 years (validated as accurate in 97% of cases [9]); the remaining 24,212 individuals were defined as having type 2 diabetes. The total study population of 273,029 adults also included 248,817 without diabetes. NHIS were reviewed and approved by the NCHS Research Ethics Review Board, and Institutional Review Board approval was not required because this study was based on secondary analyses of publicly available, de-identified data.
Study outcomes: mortality
Mortality outcomes were determined by the National Death Index (NDI) records. Accuracy of the all-cause and cause-specific death information and consistency of the matching algorithm in the NDI records were verified [22]. The underlying causes of death were collected and classified according to the International Classification of Diseases (ICD-10) guidelines (http://apps.who.int/classifications/icd10/browse/2016/en). In addition to all-cause mortality, we were interested in the following cause-specific mortality outcomes as they are the eight leading causes of death in the general population: CVD, including heart disease and stroke; cancer; chronic lower respiratory disease (CLRD); Alzheimer’s disease; diabetes mellitus; influenza and pneumonia; and kidney disease. Electronic supplementary material (ESM) Table 1 shows specific codes for causes of death.
Study exposure: sleep duration
Sleep duration data were obtained from the following self-reported interview question: ‘On average, how many hours of sleep do you get in a 24 h period?’. The smallest unit of increments was 1 h, and sleep duration was subsequently categorised into six groups (≤5, 6, 7, 8, 9 and ≥10 h/day). Extreme sleep duration was defined as sleep duration ≤5 h/day or ≥10 h/day.
Covariates
The following covariates were included as adjustment variables: age; sex; race (Hispanic, non-Hispanic White, non-Hispanic black, and others); education level (less than high school degree, high school degree, and more than high school degree); household income; lifestyle variables of BMI (normal weight or underweight [<25 kg/m2], pre-obese [25 kg/m2 to ≤30 kg/m2], obese [>30 kg/m2]), physical activity (meeting or not the 2008 Physical Activity Guidelines for Americans that recommend at least 75 min of vigorous physical activity or 150 min of moderate physical activity in 1 week), smoking status (non-smoker, former smoker, current smoker), alcohol drinking status (lifetime abstainer, former drinker, current drinker); clinical variables with self-reported diagnoses of hypertension (e.g. BP), CHD, stroke and cancer; and calendar year. We also collected and categorised the duration of diabetes into four groups of 0–5, 6 to ≤10, 11 to ≤20 and >20 years. Age at diagnosis of diabetes was classified into two groups (≤45 or >45 years of age [young and old, respectively]) [23].
Medication status was stratified into four categories: insulin only, oral glucose-lowering medication only, both and no medication.
Statistical analysis
Descriptive statistics were used to report the distribution of participants’ baseline characteristics by sleep duration. Continuous variables were displayed as mean ± SE, and categorical variables were displayed as percentage (%). Continuous data were compared with analysis of t test and variance, while Pearson’s χ2 tests were used to compare differences in baseline characteristics (including the exposure and covariates). Mortality rates were age-standardised to the overall NHIS using the age groups of 18–44 years, 45–64 years and 65 years or older. The graphical assessment of log–log plots was used to assess the proportional hazards assumption and the assumption was met in each of the models [24]. We used a multivariate Cox proportional hazards regression model to estimate HRs with corresponding 95% CIs to test the association between sleep duration categories and all-cause and cause-specific mortality. The reference group was 7 h/day. In multivariate models, we adjusted for age (as a timescale), sex, race, education level, household income, duration of diabetes (years), BMI, physical activity, smoking status, alcohol drinking status, hypertension, CHD, stroke, cancer and calendar year. Moreover, we also conducted subgroup analyses for all-cause and CVD-related mortality stratified by sex, duration of diabetes and age at diagnosis. Adjusted Wald test accounting for complex multistage sampling design was used to test for interaction term. To examine the robustness of the results, we performed sensitivity analyses excluding individuals with a history of CHD and stroke or cancer. Sampling weights were used to account for the unequal probabilities of selection. SEs were calculated by Taylor series linearisation. A p value <0.05 was considered statistically significant (two-tailed). All data analyses were performed using STATA version 12.0 (Stata Corp, College Station, TX, USA).
Results
Participant characteristics
Among the 248,817 adults without diabetes, there were 17,060 deaths during the mean 6.70 years of follow-up (1.62 million person-years). A total of 4593 deaths (2331 for women, 2262 for men) were recorded during a mean follow-up of 5.96 years (0.14 million person-years) among the 24,212 participants with diabetes. Baseline characteristics of participants with or without diabetes by sleep duration are presented in Table 1 and ESM Table 2, respectively.
Impact of sleep duration on mortality
Figure 1 shows age-standardised mortality rate per 10,000 person-years stratified by the presence of diabetes and sleep duration. Mortality rate was highest with extreme sleep duration (≤5 h/day and ≥10 h/day) and lowest with sleep duration of 7 h/day, regardless of the presence of type 2 diabetes (Table 2).
Extremes of sleep duration were associated with increased risk in mortality among adults with and without diabetes (Fig. 2). Individuals with type 2 diabetes who reported the shortest and longest sleep duration had higher all-cause mortality risk than the non-diabetic group who slept for 7 h/day (≤5 h/day, HR 1.63 [95% CI 1.24, 2.13]); ≥10 h/day, HR 2.17 [1.72, 2.73]) (Table 2). There was a non-significant interaction between sleep duration and the presence of diabetes (p for interaction = 0.08).
Among individuals with type 2 diabetes, compared with the reference group (7 h/day sleep), both shorter and longer sleep duration were associated with increased mortality risk (≤5 h/day, HR 1.24 [1.09, 1.40]; ≥10 h/day, HR 1.83 [1.61, 2.08]) (Table 3 and Fig. 3). A subgroup analysis showed a similar J-shaped curve among women and men, respectively (Table 3 and Fig. 4a).
Sleep duration and cause-specific mortality
People with type 2 diabetes who slept for ≤5 h/day, 8 h/day and ≥10 h/day had 41%, 26% and 59% greater risk of cancer mortality, respectively, compared with those who slept for 7 h/day (Table 3 and Fig. 4b). The association between sleep duration and CVD mortality risk in individuals with type 2 diabetes was only statistically significant for people who slept for ≥10 h/day (HR 1.74 [1.33, 2.28]) (Table 3 and Fig. 4c). For heart disease mortality specifically, the excess risk was only statistically significant for ≥10 h/day sleep duration (HR 1.51 [1.11, 2.07]). Of all the CVD types, the most prominent sleep–mortality association was observed for stroke mortality (sleep duration ≥10 h/day, HR 2.95 [1.63, 5.34]). For other causes of death, we observed a statistically significant association between sleep duration and mortality risk from kidney disease, Alzheimer’s disease and CLRD (Table 3). Although the subgroup analysis by sex showed higher HRs among men, the test for interaction term was not statistically significant due to wider CIs (Table 3).
Subgroup analyses
Age of diabetes onset
Comparing people with type 2 diabetes diagnosed before the age of 45 years vs those diagnosed after 45 years, the shortest and longest sleep durations were associated with greatest risk of all-cause mortality relative to those sleeping 7 h/day among people (Table 4). For CVD-specific mortality, significant increased risk was only observed in those diagnosed with type 2 diabetes at the age of >45 years and who slept for ≥10 h/day (HR 1.73 [1.28, 2.33]) (Table 4).
Duration of diabetes
Shorter sleep duration (≤5 h/day) was associated with the highest all-cause mortality risk in those living with type 2 diabetes for >20 years (HR 1.41 [1.08, 1.84]) (Table 4). For individuals who slept for ≥10 h/day, those living with type 2 diabetes for 11–20 years had an HR of 2.18 (95% CI 1.73, 2.74) and those living with type 2 diabetes for >20 years had an HR of 1.88 (95% CI 1.49, 2.37). Similar results were observed for CVD mortality when comparing against individuals who slept for 7 h/day. A more than 97% increased CVD mortality risk was detected in individuals living with type 2 diabetes for >20 years (sleep duration ≤5 h/day, HR 1.97 [1.08, 3.56]) and risk was increased in individuals who slept for ≥10 h/day (diabetes duration 11–20 years, HR 2.98 [1.80, 4.95]; diabetes duration >20 years, HR 1.98 [1.24, 3.17]).
Medication status
In individuals with type 2 diabetes treated with both oral glucose-lowering medication and insulin, higher HRs were observed for all-cause mortality in those who slept for shorter and longer durations (Table 5). People treated with both oral glucose-lowering medication and insulin also had greater HRs for CVD mortality risk according to sleep duration (≤5 h/day, HR 2.69 [1.35, 5.37]; ≥10 h/day, HR 2.80 [1.43, 5.47]) (Table 5).
Sensitivity analysis
Sensitivity analysis was performed to test the robustness of the main effects models. After eliminating participants with a history of CVD and/or cancer, results remained largely unchanged for all associations (ESM Table 3).
Discussion
In this population-based prospective cohort study, we observed that the absolute mortality rate was higher in adults with diabetes and extremes of sleep duration. There was a non-significant interaction between sleep duration and the presence of diabetes (p for interaction = 0.08). Extremes of sleep duration were associated with significant increases in all-cause and disease-specific mortality risk among people with type 2 diabetes. The risk was greatest for those who reported the longest mean sleep duration. The associations between sleep duration and mortality from all causes, cancer, CVD, heart disease, stroke, kidney disease and CLRD appeared to be J-shaped while the association between sleep duration and Alzheimer’s disease mortality risk appeared to be most pronounced at ≥10 h/day. Subgroup analysis showed that these associations were most pronounced for people who were diagnosed with diabetes at a younger age and for those who reported living with diabetes for a longer duration and used both oral glucose-lowering medication and insulin. Our findings suggest that excessive or insufficient amounts of sleep may be risk factors for all-cause and CVD mortality in people with type 2 diabetes.
Although the association between sleep duration and all-cause mortality has been investigated in several studies among the general population [25,26,27], few studies have explored this association in individuals with established diabetes. This study provides evidence that sleep duration is associated with higher mortality risk among people with type 2 diabetes and that the absolute mortality rate is higher in diabetic individuals with extreme sleep duration. Previous studies have demonstrated the significant gap in mortality risk between adults with and without diabetes [9, 28]. The magnitude of effects of risk factors such as socioeconomic and lifestyle factors on survival outcomes may differ between the diabetic and non-diabetic population. A recent study showed that the impact of higher leisure-time physical activity was even stronger in adults with CVD than in those without [11]. The effect of relative educational disparities on mortality risk was demonstrated to differ in adults with and without diabetes [10], but no difference in the obesity–mortality association was found between those with and without diabetes [29]. In our study, the p for interaction was 0.08, indicating that there may be a difference in the association between sleep duration and mortality when comparing diabetic and non-diabetic individuals, but this did not reach significance.
Laboratory studies conducted in healthy adults have revealed that insufficient sleep is associated with 40% slower glucose clearance rate and higher sympathetic nervous system activity compared with a sleep recovery condition (mean sympathovagal balance 0.77 vs 0.66) [30]. Sympathetic activation may aggravate the status of insulin resistance, obesity and hypertension [31,32,33]. Therefore, sleep deprivation in people with type 2 diabetes is likely to exacerbate complications and affect the control and management of blood glucose, which drive excess mortality risk. It is acknowledged, however, that sleep is a complex phenomenon and extreme sleep duration may reflect poorer health status and reduced functioning (e.g. our finding that people with type 2 diabetes who sleep longer have greater mortality risk; such people may experience more severe diabetes-related complications that require more rest or long-term bed rest). Another possible explanation of these findings is that longer sleep duration has been associated with chronic inflammatory responses, which increase mortality risk. Indeed, IL-6 and C-reactive protein, indicators of infection, are elevated in individuals who report long sleep duration [34]. Chronic inflammation may accelerate the progressive condition of diabetes and its complications [35]. Recently, shorter sleep duration was shown to predict arterial stiffness in young to middle-aged adults [36].
Our findings further suggest that extremes of sleep duration (shorter or longer than 7 h/day) increase all-cause and CVD mortality in people with type 2 diabetes, particularly those with diabetes of a longer duration and who are diagnosed at an earlier age. Findings from other studies corroborate this. One recent study conducted among 3724 individuals with type 2 diabetes indicated that disease duration ≥10 years (vs <5 years) was associated with 1.82 and 1.48 times higher risk of all-cause mortality and heart failure, respectively [37]. Individuals with longer diabetes duration may be susceptible to burden or fatigue associated with chronic disease management. Similarly, those diagnosed at an early age may have a poorer overall health profile for other chronic conditions as well as that pertaining to their diabetes. This may include higher BMI, disease-related complications, medication adherence and poorer blood glucose control when compared with individuals having a shorter diabetes duration and older age at onset of diabetes [38]. Diabetes-related distress often experienced by younger people with type 2 diabetes may exacerbate problems maintaining diabetes control and other areas of self-management including sleep hygiene. However, evidence for the effectiveness of sleep interventions for improving clinical outcomes in people with type 2 diabetes is complex. This is exemplified by interventions to relieve sleep apnoea, an established risk factor for CVD events and mortality. On one hand, continuous positive airway pressure (CPAP) over 6 months was shown to improve glycaemic control and insulin resistance in people with type 2 diabetes and obstructive sleep apnoea [39] but on the other, one earlier trial of CPAP over 3 months found no such benefits [40].
In our study, subgroup analysis based on medication status showed that diabetic individuals with shorter sleep duration have the highest risk for mortality when they are treated with both insulin and oral glucose-lowering medication. A previous study showed that insulin-treated individuals with type 2 diabetes had higher Pittsburgh Sleep Quality Index and poor sleep quality [38]. Another study found that metformin therapy was associated with longer sleep duration and better sleep efficiency than that in patients not treated with metformin [39]. Patients with type 2 diabetes using both insulin treatment and oral glucose-lowering medication may have poorer glucose metabolism and glycaemic control and poorer sleep quality than those not using these medications. In addition, for individuals who have type 2 diabetes and short sleep duration, those using both insulin treatment and oral glucose-lowering medication have poorer sleep quality, such as obstructive sleep apnoea [17]. This poor sleep quality may partly explain the results that sleep deprivation was associated with the highest mortality risk among individuals with type 2 diabetes using both insulin and oral glucose-lowering medication [41].
Our study provides quantitative estimates regarding the association between sleep duration and all-cause and cause-specific mortality in people with type 2 diabetes. For people with type 2 diabetes, as per the general population, 6–8 h of sleep is recommended for reducing mortality risk [13, 26]. Sleep interventions as an adjunct to standard diabetes treatment may warrant further attention. Monitoring of sleep duration may serve as a useful tool for identifying high-risk people with type 2 diabetes in clinical practice for possible intervention, especially for those being treated with both oral glucose-lowering drugs and insulin.
Our study has several strengths, including the relatively large sample size. In addition, we conducted subgroup and sensitivity analyses to ensure the robustness of the study findings. Several limitations should also be noted. First, sleep duration and diabetes history were determined from a self-reported questionnaire without using any objective measurements. However, any measurement errors in the assessment of sleep duration would most likely be non-differential and lead to underestimation of the observed associations because of the prospective design of the study [42]. Second, the present study did not include non-fatal events, which limited our ability to estimate risk of incident disease. Third, Stata have not provided the procedure of complex survey design data to account for competing risk, thus HR estimates may be overestimated due to estimation bias caused by ignoring competing risks. Fourth, due to the nature of observational studies, the current study cannot infer causality of the sleep–mortality association among people with type 2 diabetes. Finally, we lacked data on sleep quality and other factors that may be responsible for deterioration of sleep quality (e.g. number/age of young children, type of employment, medications, anxiety/depression, sleep apnoea and insomnia). This precludes in-depth analysis in relation to sleep problems and mortality among people with type 2 diabetes. Further studies in this area should concentrate on addressing such issues.
In summary, there is some preliminary evidence that the associations between sleep duration and mortality differ between diabetic and non-diabetic individuals. Diabetes patients sleeping for less than or in excess of 7 h conferred an increased risk of all-cause and cause-specific mortality. The association was more prominent in those with younger age at disease onset. These individuals may require greater medical attention that targets sleep and lifestyle to reduce the risks of adverse health outcomes.
Data availability
The NHIS data are available from www.cdc.gov/nchs/nhis/index.htm
Abbreviations
- CLRD:
-
Chronic lower respiratory disease
- CPAP:
-
Continuous positive airway pressure
- NCHS:
-
National Center for Health Statistics
- NDI:
-
National Death Index
- NHIS:
-
National Health Interview Survey
References
International Diabetes Federation (2017) IDF diabetes atlas, 8th edn. International Diabetes Federation, Brussels
Campbell PT, Newton CC, Patel AV, Jacobs EJ, Gapstur SM (2012) Diabetes and cause-specific mortality in a prospective cohort of one million US adults. Diabetes Care 35(9):1835–1844. https://doi.org/10.2337/dc12-0002
Ramezankhani A, Azizi F, Hadaegh F, Momenan AA (2018) Diabetes and number of years of life lost with and without cardiovascular disease: a multi-state homogeneous semi-Markov model. Acta Diabetol 55(3):253–262. https://doi.org/10.1007/s00592-017-1083-x
Bae JC, Cho NH, Suh S et al (2015) Cardiovascular disease incidence, mortality and case fatality related to diabetes and metabolic syndrome: a community-based prospective study (Ansung-Ansan cohort 2001–12). J Diabetes 7(6):791–799. https://doi.org/10.1111/1753-0407.12248
Aune D, Schlesinger S, Norat T, Riboli E (2018) Diabetes mellitus and the risk of sudden cardiac death: a systematic review and meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis 28(6):543–556. https://doi.org/10.1016/j.numecd.2018.02.011
Aune D, Schlesinger S, Neuenschwander M et al (2018) Diabetes mellitus, blood glucose and the risk of heart failure: a systematic review and meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis 28(11):1081–1091. https://doi.org/10.1016/j.numecd.2018.07.005
Aune D, Feng T, Schlesinger S, Janszky I, Norat T, Riboli E (2018) Diabetes mellitus, blood glucose and the risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Diabetes Complicat 32(5):501–511. https://doi.org/10.1016/j.jdiacomp.2018.02.004
Centers for Disease Control and Prevention (2017) National diabetes statistics report, 2017. Centers for Disease Control and Prevention, US Department of Health and Human Services, Atlanta
Gregg EW, Cheng YJ, Srinivasan M et al (2018) Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet 391(10138):2430–2440. https://doi.org/10.1016/S0140-6736(18)30314-3
Dray-Spira R, Gary-Webb TL, Brancati FL (2010) Educational disparities in mortality among adults with diabetes in the U.S. Diabetes Care 33(6):1200–1205. https://doi.org/10.2337/dc09-2094
Jeong S-W, Kim S-H, Kang S-H et al (2019) Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur Heart J 40(43):3547–3555. https://doi.org/10.1093/eurheartj/ehz564
Yin J, Jin X, Shan Z et al (2017) Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc 6(9):e005947. https://doi.org/10.1161/JAHA.117.005947
Liu T-Z, Xu C, Rota M et al (2017) Sleep duration and risk of all-cause mortality: a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev 32:28–36. https://doi.org/10.1016/j.smrv.2016.02.005
Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y (2018) Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev 39:25–36. https://doi.org/10.1016/j.smrv.2017.06.011
Garcia-Perdomo HA, Zapata-Copete J, Rojas-Ceron CA (2018) Sleep duration and risk of all-cause mortality: a systematic review and meta-analysis. Epidemiol Psychiatr Sci 28(5):578–588. https://doi.org/10.1017/s2045796018000379
Itani O, Jike M, Watanabe N, Kaneita Y (2017) Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 32:246–256. https://doi.org/10.1016/j.sleep.2016.08.006
Song Y, Ye X, Ye L, Li B, Wang L, Hua Y (2013) Disturbed subjective sleep in Chinese females with T2DM on insulin therapy. PLoS One 8(1):e54951. https://doi.org/10.1371/journal.pone.0054951
Kajbaf F, Fendri S, Basille-Fantinato A et al (2014) The relationship between metformin therapy and sleep quantity and quality in patients with T2DM referred for potential sleep disorders. Diabet Med 31(5):577–580. https://doi.org/10.1111/dme.12362
Lee SWH, Ng KY, Chin WK (2017) The impact of sleep amount and sleep quality on glycemic control in T2DM: a systematic review and meta-analysis. Sleep Med Rev 31:91–101. https://doi.org/10.1016/j.smrv.2016.02.001
Wang Y, O’Neil A, Jiao Y et al (2019) Sex differences in the association between diabetes and risk of cardiovascular disease, cancer, and all-cause and cause-specific mortality: a systematic review and meta-analysis of 5,162,654 participants. BMC Med 12 17(1):136. https://doi.org/10.1186/s12916-019-1355-0
Sattar N, Rawshani A, Franzén S et al (2019) Age at diagnosis of type 2 diabetes mellitus and associations with cardiovascular and mortality risks: findings from the Swedish National Diabetes Registry. Circulation 139(19):2228–2237. https://doi.org/10.1161/CIRCULATIONAHA.118.037885
Centers for Disease Control and Prevention Statistics (2017) NHANES I Epidemiologic Follow-up Survey (NHEFS): calibration sample for NDI matching methodology. Centers for Disease Control and Prevention Statistics, Atlanta
Weeks K, Torner JC (2019) Ischemic stroke risk factor differences and their changes over time among young (45 years or less) persons in a rural state: 2012-2017. Circulation 139(Suppl 1):AP408 (Abstract). https://doi.org/10.1161/circ.139.suppl_1.P408
Garrett JM (1997) Graphical assessment of the Cox proportional hazards assumption. Available from www.stata.com/products/stb/journals/stb35.pdf. Accessed 15 Aug 2018
Gangwisch JE, Heymsfield SB, Boden-Albala B et al (2008) Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep 31(8):1087–1096. https://doi.org/10.5665/sleep/31.8.1087
Kronholm E, Laatikainen T, Peltonen M, Sippola R, Partonen T (2011) Self-reported sleep duration, all-cause mortality, cardiovascular mortality and morbidity in Finland. Sleep Med 12(3):215–221. https://doi.org/10.1016/j.sleep.2010.07.021
Tamakoshi A, Ohno Y, JACC Study Group (2004) Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep 27(1):51–54
Wang Z, Zhang H, Liu M (2017) Mortality in adults with and without diabetes: is the gap widening? Clin Epidemiol 3 9:537–544. https://doi.org/10.2147/CLEP.S148101
Zahir SF, Griffin A, Veerman JL et al (2019) Exploring the association between BMI and mortality in Australian women and men with and without diabetes: the AusDiab study. Diabetologia 62(5):754–758. https://doi.org/10.1007/s00125-019-4830-4
Spiegel K, Leproult R, Van Cauter E (1999) Impact of sleep debt on metabolic and endocrine function. Lancet 354(9188):1435–1439. https://doi.org/10.1016/S0140-6736(99)01376-8
Hall JE, Hildebrandt DA, Kuo J (2001) Obesity hypertension: role of leptin and sympathetic nervous system. Am J Hypertens 14(S3):103S–115S. https://doi.org/10.1016/S0895-7061(01)02077-5
Aucott L, Poobalan A, Smith W et al (2004) Weight loss in obese diabetic and non-diabetic individuals and long-term diabetes outcomes–a systematic review. Diabetes Obes Metab 6(2):85–94. https://doi.org/10.1111/j.1462-8902.2004.00315.x
Kalil GZ, Haynes WG (2012) Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hypertens Res 35(1):4. https://doi.org/10.1038/hr.2011.173
Patel SR, Zhu X, Storfer-Isser A et al (2009) Sleep duration and biomarkers of inflammation. Sleep 32(2):200–204. https://doi.org/10.5665/sleep/32.2.200
Dregan A, Charlton J, Chowienczyk P, Gulliford Martin C (2014) Chronic inflammatory disorders and risk of T2DM mellitus, coronary heart disease, and stroke. Circulation 130(10):837–844. https://doi.org/10.1161/CIRCULATIONAHA.114.009990
Kline CE, Taylor C, Kriska AM, Barinas-Mitchell E (2019) Short sleep duration is associated with greater arterial stiffness independent of sleep quality. Circulation 139(Suppl 1):AP277 (Abstract). https://doi.org/10.1161/circ.139.suppl_1.P277
Wannamethee SG, Shaper AG, Whincup PH, Lennon L, Sattar N (2011) Impact of diabetes on cardiovascular disease risk and all-cause mortality in older men: influence of age at onset, diabetes duration, and established and novel risk factors. JAMA Intern Med 171(5):404–410. https://doi.org/10.1001/archinternmed.2011.2
Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K (2010) Factors associated with poor glycemic control among patients with T2DM. J Diabetes Complicat 24(2):84–89. https://doi.org/10.1016/j.jdiacomp.2008.12.008
Martínez-Cerón E, Barquiel B, Bezos A-M et al (2016) Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and T2DM. A randomized clinical trial. Am J Respir Crit Care Med 194(4):476–485. https://doi.org/10.1164/rccm.201510-1942OC
West SD, Nicoll DJ, Wallace TM, Matthews DR, Stradling JR (2007) Effect of CPAP on insulin resistance and HbA1c in men with obstructive sleep apnoea and T2DM. Thorax 62(11):969–974. https://doi.org/10.1136/thx.2006.074351
Gamble JM, Chibrikov E, Twells LK et al (2017) Association of insulin dosage with mortality or major adverse cardiovascular events: a retrospective cohort study. Lancet Diabetes Endocrinol 5(1):43–52. https://doi.org/10.1016/s2213-8587(16)30316-3
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ (2008) Self-reported and measured sleep duration: how similar are they? Epidemiology 19(6):838–845. https://doi.org/10.1097/EDE.0b013e318187a7b
Acknowledgements
The authors thank the NCHS of the Centers for Disease Control and Prevention for sharing the NHIS data.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
This study is supported by funding from the National Natural Science Foundation of China (grant no. 81773552), the National Key Research and Development Program of China (no. 2018YFC1315302, 2017YFC1200502), the Natural Science Foundation of Zhejiang Province (LWY20H020001) and the Science and Technology Project of Wenzhou Science and Technology Bureau (Y20190125).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, and have given final approval of the version to be published. YW, CY and XC are guarantors of the work, accept full responsibility for the work and/or the conduct of the study, have access to the data and controlled the decision to publish.
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM Tables
(PDF 276 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Huang, W., O’Neil, A. et al. Association between sleep duration and mortality risk among adults with type 2 diabetes: a prospective cohort study. Diabetologia 63, 2292–2304 (2020). https://doi.org/10.1007/s00125-020-05214-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-020-05214-4