Abstract
Aims/hypothesis
The aims of this work were to assess glycaemic control in metformin users receiving their first add-on glucose-lowering therapy and to examine the real-life effectiveness of different add-on drugs.
Methods
We carried out a population-based cohort study using healthcare databases in northern Denmark during 2000–2012. We included 4,734 persons who initiated metformin monotherapy and added another glucose-lowering drug within 3 years. Attainment of recommended HbA1c goals within 6 months of add-on was investigated, using Poisson regression analysis adjusted for age, sex, baseline HbA1c, diabetes duration, complications and Charlson Comorbidity Index.
Results
Median metformin treatment duration at intensification was 12 months (interquartile range [IQR] 4–23 months) and pre-intensification HbA1c was 8.0% (IQR 7.2–9.2%) (64 [IQR 55–77] mmol/mol). Median HbA1c dropped 1.2% (13 mmol/mol) with a sulfonylurea (SU) add-on, 0.8% (9 mmol/mol) with a dipeptidyl peptidase-4 (DPP-4) inhibitor, 1.3% (14 mmol/mol) with a glucagon-like peptide-1 (GLP-1) receptor agonist, 0.9% (10 mmol/mol) with other non-insulin drugs and 2.4% (26 mmol/mol) with insulin. Compared with SU add-on, attainment of HbA1c <7% (<53 mmol/mol) was higher with GLP-1 receptor agonists (adjusted RR [aRR] 1.10; 95% CI 1.01, 1.19) and lower with DPP-4 inhibitors (aRR 0.94; 95% CI 0.89, 0.99), other drugs (aRR 0.86; 95% CI 0.77, 0.96) and insulin (aRR 0.88; 95% CI 0.77, 0.99). The proportion of metformin add-on users who attained HbA1c <7% (<53 mmol/mol) increased from 46% in 2000–2003 to 59% in 2010–2012, whereas attainment of HbA1c <6.5% (<48 mmol/mol) remained 30% among patients aged <65 years without comorbidities.
Conclusions/interpretation
Among early type 2 diabetes patients receiving their first metformin add-on treatment, HbA1c reduction with different non-insulin drugs is similar to, and comparable with, that observed in randomised trials, yet 41% do not achieve HbA1c <7% (<53 mmol/mol) within 6 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metformin monotherapy is currently the recommended initial glucose-lowering drug (GLD) for most patients with type 2 diabetes, with addition of a second GLD if HbA1c targets are not achieved. Glucose-lowering treatment options have expanded considerably [1] yet the number of head-to-head trials comparing GLDs is limited and there is little evidence to guide clinicians’ choice of add-on therapy [2]. Adding a non-insulin second-line GLD to metformin was found to reduce HbA1c levels by approximately 1% in clinical trials [3] and an individualised treatment approach following metformin initiation is currently recommended [4]. In real-world type 2 diabetes populations, who may differ from clinical trial participants in some characteristics (e.g. age, comorbidities and compliance with medications [5]), little is known about success rates when older and newer GLDs are used to intensify metformin therapy.
We aimed to assess the quality of glycaemic control in a large population-based cohort of incident metformin users receiving their first add-on glucose-lowering therapy. We examined the association of calendar time with achieved glycaemic control and compared the reduction of HbA1c for different add-on GLDs.
Methods
Setting and study population
We conducted this cohort study in northern Denmark during 2000–2012. We used linkage of existing population-based medical databases covering 1.8 million inhabitants or 30% of Denmark’s population, as described in more detail elsewhere [6]. The cohort included individuals who redeemed a first-time GLD prescription (codes A10A, A10B) of metformin monotherapy (no GLD prescription other than metformin within the first 14 days) between 1 January 2000 and 31 December 2012 and who had at least 12 months of baseline data. Metformin exposure time was estimated as the quantity filled at each prescription collection, divided by the minimum daily dose used in clinical practice (500 mg), plus another 100 days to avoid falsely assumed termination of treatment due to non-compliance [7].
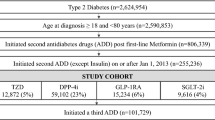
The treatment-intensification cohort consisted of metformin-exposed patients, who added another GLD within the first 3 years and had at least one HbA1c value recorded within 12 months before and within 3–6 months after the add-on prescription date in a regional laboratory information system research database [6] (for patient flow, see electronic supplementary material [ESM] Fig. 1).
Add-on drugs
Metformin add-on therapies examined were sulfonylurea (SU), dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, other non-insulin GLDs and insulin. The first intensification drug defined add-on exposure and subsequent changes were ignored, an approach similar to intention-to-treat analyses.
HbA1c outcomes
Baseline HbA1c was defined as the most recently measured HbA1c value within 12 months prior to the intensification date. We assessed the HbA1c level achieved between 2 and 6 months (60–180 days) following the intensification date. If there were several HbA1c measurements, the value closest to day 180 was used. HbA1c was analysed by either the HPLC method or immunoassays on automated equipment.
Patient characteristics
We obtained data from medical databases on 19 major disease categories included in the Charlson Comorbidity Index (CCI) based on patients’ entire hospital contact history within 5 years before the intensification date. We separately ascertained contacts and/or prescription history for mental disorders and alcoholism-related disorders (see ESM Table 1 for codes), and for any macrovascular or microvascular diabetes complication [6] including prior clinical biochemical indication of renal disease (2 days with estimated glomerular filtration rate [eGFR] ≤60 ml min−1 [1.73 m]−2 and/or 2 days with urinary albumin above the cut-off for microalbuminuria). The duration of healthcare-system-recorded diabetes was the time between the first-ever GLD prescription/hospital diagnosis of diabetes and the therapy intensification date.
Statistical analysis
For each metformin add-on therapy group, we computed absolute reduction in median HbA1c from baseline, as well as proportions of patients and RRs with 9%CIs of achieving HbA1c <6.5% (<48 mmol/mol) and <7.0% (<53 mmol/mol) with SU add-on as reference category. RRs were adjusted by Poisson regression for predefined factors (age [≤60 years, 61–70 years, >70 years], sex, diabetes duration [≤1 year, >1 year], macrovascular complications [yes/no], microvascular complications [yes/no], CCI level [0, ≥1] and baseline HbA1c [≤7.5%, 7.6–9.0%, >9.0%]). Analyses of HbA1c <6.5% (<48 mmol/mol) were restricted to a subgroup of ‘healthy’ intensification patients (i.e. aged <65 years, CCI = 0, no diabetes complications, no mental or alcoholism-related disorders), for whom providers might reasonably suggest a stringent HbA1c goal [4]. Pre-intensification HbA1c values and proportions attaining HbA1c <7% (<53 mmol/mol) and, among ‘healthy’ patients, <6.5% (<48 mmol/mol), were assessed by calendar year periods. The study was approved by the Danish Data Protection Agency (J. no. 2013-41-1924) and needed no further ethics approval according to Danish law.
Results
Patient characteristics
Among 4,734 metformin monotherapy initiators with add-on therapy and available HbA1c measurements (ESM Fig. 1), 52% (2,484) added an SU, 27% (1,262) a DPP-4 inhibitor, 7% (329) a GLP-1 receptor agonist (298 liraglutide, 31 exenatide), 6% (282) another non-insulin GLD and 8% (377) insulin. At the time of therapy intensification, the median age was 59 years (IQR 50–66 years), 20% had CCI comorbidities other than diabetes, duration of metformin use was 12 months (IQR 4–23 months) and median baseline HbA1c prior to add-on therapy was 8.0% (IQR 7.2–9.2%) (64 [IQR 55–77] mmol/mol) (Table 1).
Among patients who received SU add-on, median age was 59 years, median HbA1c was 8.0% (64 mmol/mol) and 20% had CCI comorbidities (Table 1). Corresponding figures appeared similar for patients who were intensified with DPP-4 inhibitors (60 years, 7.6% [60 mmol/mol] and 18%), GLP-1 receptor agonists, although younger (54 years, 8.0% [64 mmol/mol] and 19) and other GLDs (59 years, 7.9% [63 mmol/mol] and 20%). Patients who received insulin add-on were younger, had higher baseline HbA1c and more comorbidity (54 years, 9.6 (81 mmol/mol), and 27%).
HbA1c reduction with add-on therapy
Overall, median HbA1c dropped from 8.0% (64 mmol/mol) at baseline to 6.8% (51 mmol/mol) within 2–6 months after commencement of add-on therapy, corresponding to a reduction of 1.2% (13 mmol/mol). Absolute reductions were 1.2% (13 mmol/mol) (from 8.0 to 6.8% [64 to 51 mmol/mol]) for SU add-on, 0.8% (9 mmol/mol) (from 7.6 to 6.8% [60 to 51 mmol/mol]) for DPP-4 inhibitors, 1.3% (14 mmol/mol) (from 8.0 to 6.7% [64 to 50 mmol/mol]) for GLP-1 receptor agonists including 1.3% (14 mmol/mol) (from 7.9 to 6.6% [63 to 49 mmol/mol]) for liraglutide, 0.9% (10 mmol/mol) (from 7.9 to 7.0% [63 to 53 mmol/mol]) for other non-insulin GLDs and 2.4% (26 mmol/mol) (from 9.6 to 7.2% [81 to 55 mmol/mol]) for insulin add-on (Fig. 1 and ESM Table 2). Overall, 2,704 (57%) of all 4,734 metformin users who received add-on therapy reached an HbA1c <7% within 2–6 months, while 466 (30%) of 1,558 patients <65 years without recorded complications or comorbidities attained an HbA1c <6.5% (ESM Table 2).
Absolute reduction in median HbA1c observed before and after add-on therapy. Large arrows show baseline HbA1c (%) and absolute reduction in HbA1c (%) from baseline to 2–6 months after treatment. The figure also shows the crude proportion of all patients (%) reaching glycaemic targets of HbA1c <7.0% (<53 mmol/mol) (black ellipses) and/or HbA1c <6.5% (<48 mmol/mol) in patients <65 years with no comorbidities (white ellipses). To convert values for HbA1c in % into mmol/mol, subtract 2.15 and multiply by 10.929
Compared with SU add-on, attainment of HbA1c <7% (<53 mmol/mol) was higher with GLP-1 receptor agonists (adjusted RR [aRR] 1.10; 95% CI 1.01, 1.19), including liraglutide (aRR 1.12; 95% CI 1.03, 1.22), and lower with DPP-4 inhibitors (aRR 0.94; 95% CI 0.89, 0.99), other non-insulin GLDs (aRR 0.86; 95% CI 0.77, 0.96) and insulin (aRR 0.88; 95% CI 0.77, 0.99) (Fig. 2 and ESM Table 2). Similar differences in attainment of an HbA1c target <6.5% (<48 mmol/mol) appeared among type 2 diabetes patients aged <65 years without complications or comorbidities (Fig. 2 and ESM Table 2), as well as in analyses restricted to the 2007–2012 period (n = 3,612 patients) (ESM Table 3), yet due to the smaller populations these estimates were statistically imprecise.
aRRs for attaining HbA1c targets of <7% (<53 mmol/mol) in all patients (a) and <6.5% (<48 mmol/mol) in patients <65 years with no comorbidities (b) 2–6 months after intensification. RR was adjusted for age, sex, diabetes duration, macrovascular type 2 diabetes complications, microvascular type 2 diabetes complications, CCI score and baseline HbA1c
HbA1c over calendar time
The proportion of all metformin users who attained HbA1c targets of <7% (<53 mmol/mol) and <6.5% (<48 mmol/mol), respectively, after add-on therapy increased from 46% and 26% in 2000–2003 to 59% and 29% in 2010–2012. This apparent time trend was associated with decreasing pre-intensification HbA1c values over time (ESM Fig. 2). Corresponding proportions for metformin users aged <65 years without comorbidities who attained HbA1c <6.5% (<48 mmol/mol) remained around 30% with a slightly decreasing tendency (ESM Fig. 3). The median HbA1c level achieved in 2010–2012 was 6.8% (IQR 6.4–7.4%) (51 [IQR 46–57] mmol/mol) in all metformin add-on users and was identical at 6.8% (IQR 6.4–7.4%) (51 [IQR 46–57] mmol/mol) in metformin add-on users aged <65 years without comorbidities.
Discussion
Among real-world metformin users with short diabetes duration (0 to ≤3 years) who receive first add-on treatment, reduction in median HbA1c was approximately 1% and comparable with that observed in randomised clinical trials [5]. Differences between add-on treatment regimens were modest, and HbA1c reductions with add-on of DPP-4 inhibitors (0.8%, 9 mmol/mol), SU (1.2%, 13 mmol/mol) and GLP-1 receptor agonists (1.3%, 14 mmol/mol) were similar. Nonetheless, 41% of patients in the most recent years did not achieve an HbA1c <7% (<53 mmol/mol) within 6 months.
The absolute HbA1c reduction with insulin add-on therapy may be overestimated as it is positively correlated with baseline HbA1c level, which was 1.5–2% (17–22 mmol/mol) higher [3]. In contrast, the absolute HbA1c reduction was similar for SU and GLP-1 receptor agonist add-on, although the aRR for reaching HbA1c <7% (<53 mmol/mol) was slightly higher with GLP-1 receptor agonists. Adjusted estimates for reaching HbA1c targets with insulin tended to be lower, possibly related to some of the challenges that patients experience with early insulin administration in real life [8]. Nonetheless, our finding of similar HbA1c levels achieved with insulin and other GLDs despite different HbA1c baseline levels suggest that physicians choose effective therapy for patients with poor baseline glycaemic control, in accordance with guidelines [4, 8].
Few, if any, comparable population-based studies have focused on early glycaemic control in metformin initiators after intensification. Across 11 US health systems, in 2005–2009, 48% achieved an HbA1c <7% (<53 mmol/mol) among a subgroup of 3,135 patients who initiated monotherapy and then added an oral agent within 12 months [9], which is comparable with the findings of the current study.
It is encouraging that an increasing share of patients reach HbA1c <7% (<53 mmol/mol) after therapy intensification. This may be related to decreasing pre-intensification HbA1c levels over time, likely reflecting closer follow-up and earlier treatment [6]. Nonetheless, it is of concern that more than 70% of early metformin users aged <65 years without recorded complications or comorbidities did not reach an HbA1c level of <6.5% (<48 mmol/mol) as recommended by treatment guidelines and 25% still had an HbA1c level of >7.4% (>57 mmol/mol) after intensification (upper quartile). One likely explanation is that half the patients in our cohort had HbA1c ≥8.0% (≥64 mmol/mol) (median) and 25% had HbA1c ≥9.2% (77 mmol/mol) (upper quartile) at the start of add-on therapy. Alternatively, the number, the dose or the efficacy of the drugs employed prior to intensification may not have fully matched the individual needs of each patient. As the greatest potential for prevention exists early in type 2 diabetes before complications have emerged [4], future observational studies should examine possible reasons why many patients do not attain recommended HbA1c targets following intensification.
Study strengths include a population-based design within the comprehensive Danish public healthcare system and, accordingly, our data reflect actual clinical practice in diabetes care. A limitation was that HbA1c measurements within the right time frame were available only for two-thirds of potentially eligible patients. Moreover, prescription redemption is only a marker of actual drug consumption. Finally, although a wide range of confounding factors were assessed, imperfectly measured, unmeasured (e.g. BMI, beta cell function, lifestyle and socioeconomic measures) or unknown factors still may have affected risk estimates.
In conclusion, the observed glucose-lowering effects in real life are similar for different add-on drug options and comparable with those observed in randomised trials. Still, a substantial proportion of patients with type 2 diabetes in the community setting who receive intensification of metformin monotherapy do not achieve currently recommended HbA1c targets.
Abbreviations
- aRR:
-
Adjusted relative risk
- CCI:
-
Charlson Comorbidity Index
- DPP-4:
-
Dipeptidyl peptidase-4
- eGFR:
-
Estimated GFR
- GLD:
-
Glucose-lowering drug
- GLP-1:
-
Glucagon-like peptide-1
- IQR:
-
Interquartile range
- SU:
-
Sulfonylurea
References
Lipska KJ, Krumholz HM (2014) Comparing diabetes medications: where do we set the bar? JAMA Intern Med 174:317–318
Roumie CL, Greevy RA, Grijalva CG et al (2014) Association between intensification of metformin treatment with insulin vs sulfonylureas and cardiovascular events and all-cause mortality among patients with diabetes. JAMA 311:2288–2296
Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC (2010) The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care 33:1859–1864
American Diabetes Association (2015) Standards of medical care in diabetes-2015: summary of revisions. Diabetes Care 38(suppl 1):S4
Agency for Healthcare Research and Quality (AHRQ) (2011) Medicines for type 2 diabetes: a review of the research for adults. Available from: http://www.effectivehealthcare.ahrq.gov/search-for-guides-reviews-and-reports/?pageaction=displayproduct&productID=721, accessed 15 April 2015
Thomsen RW, Baggesen LM, Svensson E et al (2015) Early glycaemic control among patients with type 2 diabetes and initial glucose-lowering treatment: a 13-year population-based cohort study. Diabetes Obes Metab 17:771–780
Pottegard A, Bjerregaard BK, Larsen MD et al (2014) Use of exenatide and liraglutide in Denmark: a drug utilization study. Eur J Clin Pharmacol 70:205–214
Wallia A, Molitch ME (2014) Insulin therapy for type 2 diabetes mellitus. JAMA 311:2315–2325
Raebel MA, Ellis JL, Schroeder EB et al (2014) Intensification of antihyperglycemic therapy among patients with incident diabetes: a Surveillance Prevention and Management of Diabetes Mellitus (SUPREME-DM) study. Pharmacoepidemiol Drug Saf 23:699–710
Acknowledgements
Preliminary data from this study were presented in poster form at the 50th EASD Annual Meeting in Vienna, September 2014.
Funding
This study was partly supported by a research grant from Novo Nordisk Scandinavia AB to Aarhus University.
Duality of interest
Two of the co-authors (ESB and CLH) are employees of Novo Nordisk Scandinavia AB. As co-authors, they contributed to the design and reporting of the study. By contract, however, the Department of Clinical Epidemiology at Aarhus University had control of the data and retained final authority over design, content and interpretation of the analyses. RWT, LMB, MS, LP, HN and SPJ have reported no personal duality of interest. The Department of Clinical Epidemiology is involved in studies with funding from various companies as research grants to (and administered by) Aarhus University, including the present study. Moreover, the Department of Clinical Epidemiology is a member of the Danish Centre for Strategic Research in Type 2 Diabetes (DD2), supported by the Danish Agency for Science (grant no. 09-067009 and 09-075724). DD2 also is supported by the Danish Health and Medicines Authority, the Danish Diabetes Association and an unrestricted donation from Novo Nordisk A/S. Partners in the DD2 project are listed on the project website at www.DD2.nu. The authors have no non-financial interests that may be relevant to the submitted work.
Contribution statement
RWT, LMB, ESB, CLH and SPJ conceived and designed the study. Funding was obtained by RWT, LP, ESB, CLH and SPJ. RWT, LP and SPJ supervised the study. Data was acquired by RWT, LMB, LP and SPJ and was analysed and interpreted by all authors. Statistical analysis was performed by LMB and LP. RWT, ESB, CLH and SPJ drafted the manuscript and LMB, MS, LP and HN critically revised it for important intellectual content. All authors gave final approval of the version to be published. RWT had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis and is the guarantor.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
(PDF 176 kb)
ESM Fig. 2
(PDF 172 kb)
ESM Fig. 3
(PDF 170 kb)
ESM Table 1
(PDF 276 kb)
ESM Table 2
(PDF 347 kb)
ESM Table 3
(PDF 272 kb)
Rights and permissions
About this article
Cite this article
Thomsen, R.W., Baggesen, L.M., Søgaard, M. et al. Early glycaemic control in metformin users receiving their first add-on therapy: a population-based study of 4,734 people with type 2 diabetes. Diabetologia 58, 2247–2253 (2015). https://doi.org/10.1007/s00125-015-3698-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3698-1