Abstract
Aims/hypothesis
The purpose of the study was to test prospectively whether healthy individuals with a family history of type 2 diabetes are more susceptible to adverse metabolic effects during experimental overfeeding.
Methods
We studied the effects of 3 and 28 days of overfeeding by 5,200 kJ/day in 41 sedentary individuals with and without a family history of type 2 diabetes (FH+ and FH− respectively). Measures included body weight, fat distribution (computed tomography) and insulin sensitivity (hyperinsulinaemic–euglycaemic clamp).
Results
Body weight was increased compared with baseline at 3 and 28 days in both groups (p < 0.001), FH+ individuals having gained significantly more weight than FH− individuals at 28 days (3.4 ± 1.6 vs 2.2 ± 1.4 kg, p < 0.05). Fasting serum insulin and C-peptide were increased at 3 and 28 days compared with baseline in both groups, with greater increases in FH+ than in FH− for insulin at +3 and +28 days (p < 0.01) and C-peptide at +28 days (p < 0.05). Fasting glucose also increased at both time points, but without a significant group effect (p = 0.1). Peripheral insulin sensitivity decreased in the whole cohort at +28 days (54.8 ± 17.7 to 50.3 ± 15.6 µmol min−1 [kg fat-free mass]−1, p = 0.03), and insulin sensitivity by HOMA-IR decreased at both time points (p < 0.001) and to a greater extent in FH+ than in FH− (p = 0.008). Liver fat, subcutaneous and visceral fat increased similarly in the two groups (p < 0.001).
Conclusions
Overfeeding induced weight and fat gain, insulin resistance and hepatic fat deposition in healthy individuals. However, individuals with a family history of type 2 diabetes gained more weight and greater insulin resistance by HOMA-IR. The results of this study suggest that healthy individuals with a family history of type 2 diabetes are predisposed to adverse effects of overfeeding.
Trial registration:
ClinicalTrials.gov NCT00562393
Funding:
The study was funded by the National Health and Medical Research Council (NHMRC), Australia (no. #427639).
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Overnutrition and a sedentary lifestyle are major causes of the obesity epidemic, which is associated with increased risk of related metabolic disorders, including hypertension, coronary artery disease, insulin resistance and type 2 diabetes. First-degree relatives of individuals with a family history of type 2 diabetes (FH+) are at increased risk of developing type 2 diabetes [1, 2]. The mechanisms leading to this are not entirely clear, although defects already identified in this population include a greater tendency towards insulin resistance [2, 3], pancreatic beta cell impairment [4, 5], central adiposity [6], increased inflammation [7], increased intramyocellular lipid [8] and reduced mitochondrial function [8, 9]. We and others have also reported that these individuals have an impaired ability to respond to dietary challenge, including impaired fatty acid oxidation in response to a single high-fat meal [10] or 3 days of isoenergetic high-fat feeding [11].
Short-term experimental overfeeding is a model often used in animal studies to induce insulin resistance and associated metabolic defects. In humans, this model has previously been applied in lean healthy individuals. The observed outcomes from these studies include increases in fasting insulin and glucose [12], increases in energy expenditure [13] and intramyocellular triacylglycerol content [14] and decreases in peripheral [15] and hepatic [12] insulin sensitivity. The aim of the present study was to examine prospectively the effects of 3 and 28 days of overfeeding on body weight, fat distribution and insulin sensitivity and the relationships between these factors in healthy individuals with and without a family history of type 2 diabetes. We hypothesised that overfeeding will induce a greater adverse effect in FH+ individuals than in those without a history of type 2 diabetes (FH−).
Methods
Subjects
Sedentary, non-smoking, non-diabetic men and women who reported either no family history of type 2 diabetes (FH−) or at least one first-degree relative with type 2 diabetes (FH+) were recruited by advertising in local newspapers. Subjects were excluded if their weight had changed by >2 kg in the preceding 6 months, if they exercised more than 60 min per week, if they were taking medications known to affect insulin sensitivity or blood pressure, or if they had a personal history of type 2 diabetes or cardiovascular disease. Forty-one individuals were recruited; one male FH− participant did not complete the study due to a viral infection. The study protocol was approved by the Human Research and Ethics Committee at St Vincent’s Hospital, Sydney. Subjects provided informed written consent before commencement of the study.
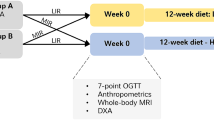
Diets
Estimated energy requirements were calculated for each participant based on fat-free mass (FFM) and fat mass (FM) using equations previously generated by doubly labelled water and intake balance techniques [16–18]. A trained dietitian then planned individual menus for participants. Study timeline and food consumption regimen are outlined in Fig. 1. Briefly, from day −3 to day 0 all foods were provided at baseline energy requirements with a nutrient composition of 30% of energy as fat, 15% as protein and 55% as carbohydrate. From days 0–3 and 25–28, all foods were provided at baseline energy requirements plus 5,200 kJ/day with a nutrient composition of 45% fat, 15% protein and 40% carbohydrate. During the overfeeding phase we aimed to double the amount of fat intake by providing three high energy-high fat snacks per day, each providing ∼1,000 kJ (e.g. potato crisps, chocolate bars, cheesecake) and a liquid oil-based supplement (Benecalorie; Novartis, Basel, Switzerland; ∼1,400 kJ) mixed in a dairy dessert (∼800 kJ). On days 3–25 of overfeeding, participants were instructed to consume their regular diets and were provided with the above snacks and supplement to achieve an intake of 5,200 kJ/day above the baseline energy requirement. They were required to complete a checklist every day, reporting which snacks were consumed, complete a 3 day diet diary once before study commencement and twice during the overfeeding phase, and to meet the study dietitian weekly. The checklists were reviewed during weekly weighings by the study dietitian so that any deviations from protocol were quickly identified and alternative options could be provided, in order to improve adherence to the diet plan. Diets were analysed for macronutrients and fatty acid composition using FoodWorks 2007 based on the Australian foods database (Xyris Software, QLD, Australia). Thirty-two participants returned the diet diaries of both study phases (Table 1).
Study timeline and food consumption regimen. From day −3 to the baseline study, all foods were provided to participants at calculated baseline energy requirements (a; 30% of energy as fat, 15% as protein and 55% as carbohydrate). During the overfeeding phase (shaded), on days 0–3 and 25–28, all foods were provided to participants at calculated baseline energy requirements +5,200 kJ/day (b; 45% of energy as fat, 15% as protein and 40% as carbohydrate). On days 3–25, participants were instructed to consume their regular diet and were provided with high-fat snacks to provide an additional 5,200 kJ/day (c)
Metabolic testing
Subjects attended the clinical research facility at 08:00 hours after a 12 h overnight fast at baseline and on days 3 and 28 of overfeeding (Fig. 1). The baseline and 28 day visits were identical: weight, height and blood pressure were measured in a hospital gown after voiding and fasting blood samples were drawn. After 30 min of supine rest, resting metabolic rate (RMR) and respiratory quotient (RQ) were determined for 30 min (ParvoMedics, UT, USA). A peri-umbilical subcutaneous fat biopsy was performed as described previously [19]. Insulin sensitivity was then measured using a 2 h hyperinsulinaemic–euglycaemic clamp (60 mU m−2 min−1), as described previously [10]. Glucose was infused at a variable rate to maintain glucose at 5.0 mmol/l and the steady-state glucose infusion rate was calculated between 90 and 120 min. Indirect calorimetry was repeated in conjunction with the steady-state measurement. Stanford 7 day activity recalls were administered at baseline and after 28 days of overfeeding according to previously published guidelines [20]. At 3 days of overfeeding, weight and blood pressure were measured, fasting blood samples were obtained and indirect calorimetry was performed. Participants attended the clinical research facility weekly for weight follow-up, snack collection and consultation with the study dietitian.
Body composition
Fat mass, fat-free mass and central abdominal fat were assessed at baseline and day 28 of overfeeding by dual energy x-ray absorptiometry (DXA; Lunar DPX-Lunar Radiation, Madison, WI, USA), as described previously [21]. Three cross-sectional computed tomography (CT) scans (Gemini GXL; Philips, the Netherlands), 1 cm wide, centred on the L2–L3, L4–L5 and the T12–L1 disc spaces were also performed to assess abdominal adipose tissue distribution and hepatic fat content. Abdominal areas of adipose tissue were defined by attenuation values of −50 to 150 Hounsfield units, as described previously [19]. CT images were analysed using Gemini (GXL Host System; Philips, the Netherlands). Two participants did not undergo CT scans. L4–L5 superficial and deep subcutaneous adipose tissues were not able to be analysed in four participants and the spleen was not visualised in two participants.
Measurement of fat cell size
Subcutaneous adipose biopsies were fixed in Bouin’s fluid, dehydrated, paraffin-embedded and then sectioned (4 µm). Sections were stained with haematoxylin and eosin. Digital images were captured using a camera (TriCCD; Sony, Paris, France) and diameters measured using Perfect Image software (Claravision, Orsay, France). Fat cell size was measured in 33 participants who had histological samples available before and after intervention. Adipocyte diameter was measured blindly and for at least two fields of view. The mean diameter was calculated from an average of 400 cells per sample.
Biochemical analysis
Glucose was analysed using a glucose oxidase electrode (YSI Life Sciences, OH, USA). Fasting serum insulin, C-peptide and leptin were assayed by radioimmunoassay (Linco Research, St Charles, MO, USA). HOMA-IR was calculated as described previously [22]. HDL-cholesterol and triacylglycerol were evaluated by enzymatic colorimetry (Roche, IN, USA). LDL was calculated by the Friedewald equation. NEFA was measured by an enzymatic colorimetry assay (Wako, Osaka, Japan).
Statistical analysis
Data are presented as mean ± SD unless otherwise stated. Statistics were analysed with SPSS 15 (SPSS, Chicago, IL, USA). Leptin and insulin data were not normally distributed and were log-transformed for analysis. Baseline differences between groups were analysed by one-way ANOVA. All other data were analysed using repeated measures with respect to group and time, and an intention-to-treat approach without carrying forward data on the one dropout. Bonferroni post hoc analysis was performed and further analysis was performed by independent t test. Linear regression at baseline (n = 41) was used to generate equations for predicting RMR with FFM and FM in the model as described previously [16]. Correlations were calculated using Pearson’s correlation coefficient. Significance was set at p < 0.05.
Results
Baseline characteristics
Baseline characteristics by group are shown in Table 2. There were no detectable differences between groups at baseline with respect to age, weight, BMI, blood pressure, fasting glucose, insulin, C-peptide, leptin, lipid profile or peripheral insulin sensitivity. The only difference was in carbohydrate oxidation in response to insulin infusion during the hyperinsulinaemic–euglycaemic clamp (∆RQ), which was lower in FH+ than in FH− individuals. At baseline, peripheral insulin sensitivity was related to liver/spleen ratio (r = 0.5, p = 0.001) and visceral adipose tissue (r = −0.4, p = 0.01). Fat cell size correlated with body fat percentage by DXA (r = 0.4, p = 0.04), subcutaneous adipose tissue (r = 0.4, p = 0.02), serum NEFA (r = 0.4, p = 0.02), triacylglycerol (r = 0.5, p = 0.006) and insulin resistance by HOMA-IR (r = 0.5, p = 0.007).
Diet diary and physical activity questionnaire analysis
Reported dietary intakes at baseline and during overfeeding by group are given in Table 1. Dietary fat (g) approximately doubled in the overfeeding phase. Carbohydrate and protein intakes also increased (p < 0.0001). There were no significant differences in energy, carbohydrate or protein intake between groups, although a tendency was noted for FH+ to consume more total energy (p = 0.15) and more fat during overfeeding (p = 0.07) compared with FH− participants. The average self-reported consumption of snacks during the overfeeding period was 92 ± 14% and 95 ± 9% in FH− and FH+ participants respectively (p = 0.4). Reported levels of physical activity were similar at baseline (230 ± 8 and 232 ± 12 metabolic equivalent of task (MET-h week−1 in FH− and FH+ respectively, p = 0.7) and did not change with overfeeding (229 ± 7 and 231 ± 7 MET-h week−1 in FH− and FH+ respectively; time p = 0.4, group p = 0.8).
Changes in weight and fat distribution in response to overfeeding
As expected, overfeeding resulted in significant weight gain at 3 and 28 days compared with baseline (Fig. 2a). At 3 days, weight gain was not different between groups. At 28 days, FH+ individuals had gained 1.2 kg more than FH− individuals (p < 0.05). Weight gained as percentage of baseline weight was 0.7 ± 0.9% and 1.0 ± 0.7% in FH− and FH+ respectively at 3 days (p = 0.4) and 3.1 ± 2.0% and 4.4 ± 2.0% in FH− and FH+ respectively at 28 days of overfeeding (p < 0.05). Fat mass, fat-free mass, central fat by DXA and visceral and subcutaneous adipose tissue volume by CT increased similarly in the two groups (Table 3). Circulating leptin increased significantly with weight gain and to a greater extent in FH+ than in FH− participants at 28 days (Fig. 2b), consistent with the greater weight gain in the former group. The increases in circulating leptin concentration at days 3 and 28 correlated with weight gains at these time points (r = 0.3, p = 0.03 at 3 days and r = 0.5, p = 0.003 at 28 days). Preferential fat gain in the L2–L3 visceral depot was observed in the whole cohort, increasing from 33 ± 15% at baseline to 34 ± 14% at 28 days of overfeeding (p = 0.008). However, this was abolished when baseline visceral volume was included as a covariate (p = 0.1). Liver fat increased significantly in response to overfeeding similarly in the two groups (Table 3) and correlated with weight gain (R 2 = 0.17, p = 0.01). Abdominal fat cell size did not change (Table 3).
Body weight, circulating hormones and metabolites, HOMA-IR and respiratory quotient at baseline and in response to overfeeding. Body weight (a), serum leptin (b), glucose (c), insulin (d), C-peptide (e), HOMA-IR (f), NEFA (g) and RQ (h) at baseline and at +3 and +28 days of overfeeding in participants with (white squares) and without (black squares) a family history of type 2 diabetes. Difference from baseline: *p < 0.05, † p < 0.005. Difference between groups: ‡ p < 0.05, ‡‡ p < 0.01, § p = 0.06
Metabolic responses to overfeeding
Fasting glucose increased significantly at days 3 and 28 of overfeeding compared with baseline, but this response was not significantly different between groups (Fig. 2c). Fasting insulin and C-peptide increased at 3 and 28 days of overfeeding (Fig. 2d, e), with a greater increase in insulin in FH+ than in FH− individuals at both time points (p < 0.01, Fig. 2d) and in C-peptide at 28 days (p < 0.05; Fig. 2e). Accordingly, HOMA-IR (reflecting fasting insulin resistance) increased significantly in both groups (p < 0.005 for both time points; Fig. 2f), the increase being more pronounced in FH+ individuals (p < 0.01). Peripheral insulin sensitivity measured by the hyperinsulinaemic–euglycaemic clamp at 28 days decreased significantly in the whole cohort from 54.8 ± 17.7 to 50.3 ± 15.6 µmol min−1 [kg FFM]−1 at 28 days of overfeeding (p = 0.03), but was not different between groups. Total cholesterol and HDL-cholesterol increased significantly in response to overfeeding similarly in the two groups (4.6 ± 1.0 to 4.8 ± 1.0, p = 0.01 for total cholesterol and 1.3 ± 0.3 to 1.4 ± 0.4, p < 0.0001 for HDL-cholesterol). Blood pressure, LDL-cholesterol and triacylglycerol levels were unchanged (data not shown). Fasting NEFA levels were significantly suppressed at 3 days (p < 0.001) and returned to the basal level at 28 days of overfeeding, without a group effect (p = 0.4; Fig. 2g). Plasma NEFA was suppressed in the hyperinsulinaemic state (by clamp) at both baseline and 28 days of overfeeding (p < 0.0001), without a group difference at both time points (data not shown). Similarly, fasting RQ increased at 3 days (p < 0.0001) and returned to the basal level at 28 days, without a group effect (p = 0.8; Fig. 2h). The ∆RQ during the clamp was not altered by overfeeding (data not shown). Absolute RMR at baseline was not different between groups (Table 2) and increased after overfeeding at 3 and 28 days in both groups (p < 0.01). This increase was not different between FH− and FH+ groups at 3 days (290 ± 650 and 350 ± 550 kJ/day respectively, p = 0.8) or 28 days (330 ± 710 and 350 ± 550 kJ/day respectively, p = 0.9). Baseline RMR adjusted for FFM was not different between groups or in response to overfeeding (data not shown). We also calculated predicted RMR at 28 days based on equations derived at baseline (RMR = 158.8 + 19.91 × FFM + 10.37 × FM), as described previously [16], and found no difference between the predicted and measured RMR at 28 days of overfeeding (data not shown). We did not perform DXA measurements at day 3 but repeated this analysis using body weight at baseline (RMR = 344.9 + 14.0 × body weight). Similarly, we found no difference at 28 days. However, at day 3, measured RMR (6,100 ± 990 kJ/day) was significantly elevated above weight-predicted RMR (5,800 ± 640 kJ/day, p = 0.03). There was no difference between groups in this response (data not shown). The increase in thermogenesis in response to insulin infusion was 480 ± 690 kJ/day at baseline and 520 ± 620 kJ/day after overfeeding; neither value differed between groups (data not shown).
Discussion
High-fat overfeeding induces insulin resistance in rodent models in as little as 3 weeks [23, 24]. In this study we established that 28 days of overfeeding induced weight gain and peripheral insulin resistance in healthy non-diabetic individuals. We also showed that fat was deposited in the liver and we established that individuals who reported a family history of type 2 diabetes gained more weight and developed greater insulin resistance by HOMA-IR when provided with identical dietary instructions.
This is the first study to compare the effects of experimental overfeeding in individuals with and without a family history of type 2 diabetes, and we observed that weight gain was higher in FH+ than in FH− individuals. Moreover, since overconsumption by 44 kJ is required to gain 1 g of body weight [25, 26] and assuming no compensatory change in energy expenditure, we predicted a maximum weight gain of 3.3 kg with 28 days of overfeeding. We observed that FH+ individuals gained approximately the predicted weight whereas FH− individuals gained less weight than predicted. It should be emphasised that participants were free-living and self-selecting their foods for most of the study. Therefore, this difference may be explained by dietary compliance and may suggest that FH− individuals are less able to over-eat. Consistent with this, a trend towards greater fat and energy consumption was observed in FH+ individuals compared with FH− individuals. This outcome is of great interest as identical dietary instructions and food options were provided to both groups. Although FH+ had gained on average 1.2 kg more than FH− individuals at day 28, we did not detect significant group differences in compartmental gain by CT and DXA. This apparent inconsistency may stem from the lower reproducibility and higher variability of DXA [27] and CT estimates compared with a single scale weight. Interestingly, we have previously reported impaired peptide YY secretion in response to a meal in FH+ individuals [28], which may contribute to reduced satiety and facilitate weight gain. Even the classical experimental overfeeding studies [29–31], in which participants were incarcerated and all foods were provided, have shown wide variability in weight gain in response to controlled overfeeding. Furthermore, an experimental weight gain study in twins demonstrated a heritable component of weight gain, with much greater variability in weight gain between than within twin pairs [31]. In those studies, since energy intake was very carefully controlled, it is likely that differences in weight gain were due to variations in the thermogenic response to overfeeding and possibly non-exercise activity thermogenesis [32]. In the present study, we suggest that the weight gain differences between groups were not due to differences in compensatory changes in resting energy metabolism or physical activity levels by questionnaire, since more complex measures of activity were not used.
Overfeeding increased fasting insulin, glucose and peripheral insulin resistance in the whole cohort. This is consistent with previous studies of short-term (3 days) [15] and long-term (4.5 months) overfeeding [33] in healthy lean men. Our initial hypothesis was that metabolic defects associated with overfeeding would be greater in FH+ than in FH− individuals. Indeed, we observed that fasting serum insulin and C-peptide increased more in individuals with a family history of type 2 diabetes than in those without such a family history. Fasting blood glucose tended to increase more in FH+ than in FH− individuals at +3 days of overfeeding; this may account for the significant increase in insulin in the FH+ group. Notably, the insulin increase was maximal after just 3 days of overfeeding, which was during a time when all foods were provided to participants and prior to any detectable weight gain differences between groups. Consistently, in response to 5 days overfeeding, healthy lean men increased insulin secretion during an IVGTT [12]. In longer term overfeeding studies, reduced insulin clearance was observed after 4.5 months and significant weight gain in lean young men [33]. These findings are similar to those in dogs fed a diet with a moderately increased fat level, in which an increase in beta cell secretion was observed at 6 weeks but was no longer evident at 3 months, when hyperinsulinaemia was maintained by reduced insulin clearance by the liver [34].
There is increasing evidence to suggest that the location of fat deposition may be more important than the total amount of fat stored in obese individuals [19]. For example, ectopic deposition of lipid within the liver is closely associated with traits of the metabolic syndrome [19, 35]. Consistent with this, we also observed a relationship between liver fat by CT and peripheral insulin resistance in this non-diabetic cohort at baseline. Gold standard measures of liver fat were not conducted in the present study; however, findings by magnetic resonance spectroscopy and CT measurement of liver fat content are closely correlated [36]. Interestingly, we observed that deposition of fat within the liver was increased in response to 28 days of overfeeding, and although we did not detect a difference between groups the increase in fat was closely aligned with the amount of weight gained. Deposition of fat in the liver in response to high fat overfeeding has been shown in rodents and dogs [37, 38] and in response to 3 days of a high fat overfeeding in healthy lean men by magnetic resonance spectroscopy [39]. Interestingly, moderate energy restriction for 2 days decreases liver fat in obese people [40]. Increased visceral fat is also closely associated with insulin resistance [41] and increased visceral adipose tissue is observed in BMI-matched insulin-resistant FH+ individuals [6]. In the present study, visceral adiposity was similar between groups at baseline and FH+ individuals were not more likely than FH− individuals to deposit fat in the visceral compartment in response to overfeeding. Increased fat cell size is also observed in insulin resistance and may represent failure of the adipose tissue mass to expand to accommodate increased energy intake [19]. We did not detect an increase in average fat cell size with the moderate weight gain achieved in this study. This result is in contrast to the results of a historical experimental overfeeding study [29], but that intervention was longer and weight gain was much greater.
There is some evidence to suggest that post-obese individuals do not appropriately oxidise dietary fat, which may predispose them to weight regain [42]. There is also marked variability between individuals in the capacity to switch appropriately between fat and carbohydrate oxidation [43]. This response has been termed metabolic flexibility [44] and has been associated with insulin resistance [11] and may also predispose to weight gain. In this study, we observed impaired metabolic flexibility in response to insulin infusion in FH+ individuals at baseline. However, this defect was not altered by overfeeding and there was no difference between groups in the fasting rates of fatty acid oxidation at baseline or during overfeeding, and thus is unlikely to have contributed to the increased weight gain observed in FH+ individuals. Overfeeding initially suppressed fatty acid oxidation. This may have been due to suppressed lipolysis of adipose tissue, as evidenced by reduced plasma NEFA and mediated by the increase in insulin. Interestingly, fasting levels of fat oxidation and plasma NEFA returned to basal by 28 days despite continuation of overfeeding, possibly as peripheral insulin resistance increased.
In conclusion, short-term overfeeding induced insulin resistance and deposition of fat in the liver in healthy men and women. Individuals with a family history of type 2 diabetes were more susceptible to weight gain and developed greater insulin resistance by HOMA-IR, which was evident even prior to any detectable difference in weight gain. The results of this study suggest that healthy individuals with a family history of type 2 diabetes are predisposed to adverse effects of overfeeding, which may help explain their susceptibility to the development of type 2 diabetes in an obesogenic environment.
Abbreviations
- CT:
-
Computed tomography
- DXA:
-
Dual energy X-ray absorptiometry
- FFM:
-
Fat-free mass
- FH:
-
Family history
- FM:
-
Fat mass
- HOMA-IR:
-
HOMA–insulin resistance
- RMR:
-
Resting metabolic rate
- RQ:
-
Respiratory quotient
References
Meigs JB, Cupples LA, Wilson PW (2000) Parental transmission of type 2 diabetes: the Framingham Offspring Study. Diabetes 49:2201–2207
Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR (1990) Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann Intern Med 113:909–915
Rothman DL, Magnusson I, Cline G et al (1995) Decreased muscle glucose transport/phosphorylation is an early defect in the pathogenesis of non-insulin-dependent diabetes mellitus. Proc Natl Acad Sci U S A 92:983–987
Bonadonna RC, Stumvoll M, Fritsche A et al (2003) Altered homeostatic adaptation of first- and second-phase beta-cell secretion in the offspring of patients with type 2 diabetes: studies with a minimal model to assess beta-cell function. Diabetes 52:470–480
Thamer C, Stumvoll M, Niess A et al (2003) Reduced skeletal muscle oxygen uptake and reduced beta-cell function: two early abnormalities in normal glucose-tolerant offspring of patients with type 2 diabetes. Diabetes Care 26:2126–2132
Nyholm B, Nielsen MF, Kristensen K et al (2004) Evidence of increased visceral obesity and reduced physical fitness in healthy insulin-resistant first-degree relatives of type 2 diabetic patients. Eur J Endocrinol 150:207–214
Ruotsalainen E, Salmenniemi U, Vauhkonen I et al (2006) Changes in inflammatory cytokines are related to impaired glucose tolerance in offspring of type 2 diabetic subjects. Diabetes Care 29:2714–2720
Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI (2004) Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 350:664–671
Befroy DE, Petersen KF, Dufour S et al (2007) Impaired mitochondrial substrate oxidation in muscle of insulin-resistant offspring of type 2 diabetic patients. Diabetes 56:1376–1381
Heilbronn LK, Gregersen S, Shirkhedkar D, Hu D, Campbell LV (2007) Impaired fat oxidation after a single high-fat meal in insulin-sensitive nondiabetic individuals with a family history of type 2 diabetes. Diabetes 56:2046–2053
Ukropcova B, Sereda O, de Jonge L et al (2007) Family history of diabetes links impaired substrate switching and reduced mitochondrial content in skeletal muscle. Diabetes 56:720–727
Brons C, Jensen CB, Storgaard H et al (2009) Impact of short-term high-fat feeding on glucose and insulin metabolism in young healthy men. J Physiol 587:2387–2397
Leibel RL, Rosenbaum M, Hirsch J (1995) Changes in energy expenditure resulting from altered body weight. N Engl J Med 332:621–628
Schrauwen-Hinderling VB, Kooi ME, Hesselink MK et al (2005) Intramyocellular lipid content and molecular adaptations in response to a 1-week high-fat diet. Obes Res 13:2088–2094
Bachmann OP, Dahl DB, Brechtel K et al (2001) Effects of intravenous and dietary lipid challenge on intramyocellular lipid content and the relation with insulin sensitivity in humans. Diabetes 50:2579–2584
Heilbronn LK, de Jonge L, Frisard MI et al (2006) Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: a randomized controlled trial. JAMA 295:1539–1548
Redman LM, Heilbronn LK, Martin CK, Alfonso A, Smith SR, Ravussin E (2007) Effect of calorie restriction with or without exercise on body composition and fat distribution. J Clin Endocrinol Metab 92:865–872
Vinken AG, Bathalon GP, Sawaya AL, Dallal GE, Tucker KL, Roberts SB (1999) Equations for predicting the energy requirements of healthy adults aged 18–81 y. Am J Clin Nutr 69:920–926
Azuma K, Heilbronn LK, Albu JB, Smith SR, Ravussin E, Kelley DE (2007) Adipose tissue distribution in relation to insulin resistance in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 293:E435–E442
Washburn RA, Jacobsen DJ, Sonko BJ, Hill JO, Donnelly JE (2003) The validity of the Stanford Seven-Day Physical Activity Recall in young adults. Med Sci Sports Exerc 35:1374–1380
Carey DG, Jenkins AB, Campbell LV, Freund J, Chisholm DJ (1996) Abdominal fat and insulin resistance in normal and overweight women: direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes 45:633–638
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27:1487–1495
Kraegen EW, Storlien LH, Jenkins AB, James DE (1989) Chronic exercise compensates for insulin resistance induced by a high-fat diet in rats. Am J Physiol 256:E242–E249
Park SY, Cho YR, Kim HJ et al (2005) Unraveling the temporal pattern of diet-induced insulin resistance in individual organs and cardiac dysfunction in C57BL/6 mice. Diabetes 54:3530–3540
Pullar JD, Webster AJ (1977) The energy cost of fat and protein deposition in the rat. Br J Nutr 37:355–363
Schulz LO, Alger S, Harper I, Wilmore JH, Ravussin E (1992) Energy expenditure of elite female runners measured by respiratory chamber and doubly labeled water. J Appl Physiol 72:23–28
Pritchard JE, Nowson CA, Strauss BJ, Carlson JS, Kaymakci B, Wark JD (1993) Evaluation of dual energy X-ray absorptiometry as a method of measurement of body-fat. Eur J Clin Nutr 47:216–228
Viardot A, Heilbronn LK, Herzog H, Gregersen S, Campbell LV (2008) Abnormal postprandial PYY response in insulin sensitive nondiabetic subjects with a strong family history of type 2 diabetes. Int J Obes 32:943–948
Salans LB, Horton ES, Sims EA (1971) Experimental obesity in man: cellular character of the adipose tissue. J Clin Invest 50:1005–1011
Sims EA, Horton ES, Salans LB (1971) Inducible metabolic abnormalities during development of obesity. Annu Rev Med 22:235–250
Bouchard C, Tremblay A, Despres JP et al (1990) The response to long-term overfeeding in identical twins. N Engl J Med 322:1477–1482
Levine JA, Vander Weg MW, Hill JO, Klesges RC (2006) Non-exercise activity thermogenesis: the crouching tiger hidden dragon of societal weight gain. Arterioscler Thromb Vasc Biol 26:729–736
Erdmann J, Kallabis B, Oppel U, Sypchenko O, Wagenpfeil S, Schusdziarra V (2008) Development of hyperinsulinemia and insulin resistance during the early stage of weight gain. Am J Physiol Endocrinol Metab 294:E568–E575
Kim SP, Ellmerer M, Kirkman EL, Bergman RN (2007) Beta-cell “rest” accompanies reduced first-pass hepatic insulin extraction in the insulin-resistant, fat-fed canine model. Am J Physiol Endocrinol Metab 292:E1581–E1589
Kotronen A, Yki-Jarvinen H (2008) Fatty liver: a novel component of the metabolic syndrome. Arterioscler Thromb Vasc Biol 28:27–38
Zhong L, Chen JJ, Chen J et al (2009) Nonalcoholic fatty liver disease: quantitative assessment of liver fat content by computed tomography, magnetic resonance imaging and proton magnetic resonance spectroscopy. J Dig Dis 10:315–320
Kabir M, Catalano KJ, Ananthnarayan S et al (2005) Molecular evidence supporting the portal theory: a causative link between visceral adiposity and hepatic insulin resistance. Am J Physiol Endocrinol Metab 288:E454–E461
Turner N, Hariharan K, Tidang J et al (2009) Enhancement of muscle mitochondrial oxidative capacity and alterations in insulin action are lipid species-dependent: potent tissue-specific effects of medium chain fatty acids. Diabetes 58:2547–2554
van der Meer RW, Hammer S, Lamb HJ et al (2008) Effects of short-term high-fat, high-energy diet on hepatic and myocardial triglyceride content in healthy men. J Clin Endocrinol Metab 93:2702–2708
Kirk E, Reeds DN, Finck BN, Mayurranjan SM, Patterson BW, Klein S (2009) Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Gastroenterology 136:1552–1560
Jensen MD (2008) Role of body fat distribution and the metabolic complications of obesity. J Clin Endocrinol Metab 93:S57–S63
Larson DE, Ferraro RT, Robertson DS, Ravussin E (1995) Energy metabolism in weight-stable postobese individuals. Am J Clin Nutr 62:735–739
Smith SR, DE Jonge L, Zachwieja JJ et al (2000) Fat and carbohydrate balances during adaptation to a high-fat. Am J Clin Nutr 71:450–457
Kelley DE (2005) Skeletal muscle fat oxidation: timing and flexibility are everything. J Clin Invest 115:1699–1702
Acknowledgements
We would like to thank L. Schofield (the study co-ordinator) and A. Jenkins for statistical advice, and all the volunteers who participated in this demanding research study. The study was funded by the National Health and Medical Research Council (NHMRC), Australia. L. K. Heilbronn is supported by an NHMRC Career Development Award (No. 481354) and C. S. Tam by an NHMRC/NHF Postgraduate Biomedical Scholarship (No. 457224).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samocha-Bonet, D., Campbell, L.V., Viardot, A. et al. A family history of type 2 diabetes increases risk factors associated with overfeeding. Diabetologia 53, 1700–1708 (2010). https://doi.org/10.1007/s00125-010-1768-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1768-y
Keywords
Profiles
- L. K. Heilbronn View author profile