Abstract
Aims/hypothesis
Diabetic retinopathy is the result of increased oxidative and nitrosative stress induced by chronic hyperglycaemia, and affects the vasculature and the neuroglia. Erythropoietin is a neuroprotective and an endothelial survival factor. We assessed the effect of suberythropoietic epoetin delta doses on variables of oxidative stress in target tissues of diabetic complications and on pericyte loss in the diabetic retina.
Methods
We administered epoetin delta to streptozotocin-induced diabetic Wistar rats at doses of 384 IU/kg body weight once weekly or 128 IU/kg body weight three times a week. The treatment lasted for 3 months. Oxidative stress and formation of AGEs were assessed by immunoblotting, expression of Ang-2 (also known as Angpt2) by RT-PCR, activation of protein kinase B (AKT) and heat shock protein (HSP)-27 levels by immunofluorescence, and incipient retinal vascular changes by quantitative morphometry of retinal digest preparations.
Results
Diabetes increased variables of oxidative stress and nitrosative stress (N ε-carboxymethyl-lysine, nitrotyrosine and methylglyoxal-type AGEs) in retina, kidney and heart of diabetic rats. Epoetin delta reduced oxidative and nitrosative stress in all tissues, and AGEs in the retina. It also reduced increased retinal Ang-2 expression and pericyte loss, and ameliorated p-AKT and HSP-27 levels.
Conclusions/interpretation
Epoetin delta has antioxidative properties in organs affected by diabetes and may prevent incipient microvascular damage in the diabetic retina.
Similar content being viewed by others
Introduction
Chronic hyperglycaemia increases oxidative stress in target organs of diabetic late complications [1]. The increase in oxidative stress can result from diverse hyperglycaemia-induced abnormalities, where glucose-driven mitochondrial overproduction of reactive oxygen species (ROS) plays a central role [2]. Mitochondrial ROS activate the nuclear protection system, poly-ADP-ribose polymerase (PARP), which interferes with the glycolytic pathway, inducing a reduction of glyceraldehyde-3-phosphate dehydrogenase (GAPDH) activity and a consecutive overflow of metabolites into biochemical pathways such as the hexosamine pathway or the formation of AGEs. With persistent hyperglycaemia and the resulting activation of the AGE pathway, tissue oxidative stress involving cytoplasmic ROS-overproduction and progressive exhaustion of endogenous antioxidants persists [3–5].
Apart from accelerated AGE formation, the combination of increased glycation and oxidation gives rise to glycoxidation products, which are also considered to be AGEs and represent tissue markers of cumulative oxidative stress. N ε-(Carboxymethyl) lysine (CML) is one well characterised glycoxidation product, which serves as a biomarker of general oxidative stress, accumulates in tissues with age and whose rate of accumulation is accelerated in diabetes [6–8]. ROS, in particular superoxide anions, interact with nitric oxide, forming the strong cytotoxin, peroxynitrite, which attacks various biomolecules, leading to the production of a modified amino acid nitrotyrosine [9]. Nitrotyrosine measurements have been established as a biomarker of nitrosative stress, which is implicated as a key mechanism in diabetic pathologies, affecting enzyme activities, antioxidant capacities, signal transduction and DNA integrity [10]. Target tissues of microvascular damage in diabetes differ substantially in substrates susceptible to oxidative damage, such as that caused by polyunsaturated fatty acids, and in their predisposition to inflammatory cell infiltration [11–13].
Vasoregression in the diabetic retina starts with pericyte loss, which is likely to involve the angiopoietin (ANG) Tie system [14]. Angiopoietin-1 as the activating ligand for the endothelial receptor tyrosine kinase TIE-2 promotes endothelial survival and tightness of the blood retinal barrier. The endogenous antagonist ANG-2 promotes angiogenesis in cooperation with vascular endothelial growth factor (VEGF) and induces vasoregression in conditions where VEGF is low [15]. ANG-2 upregulation precedes pericyte dropout in the diabetic retina. ANG-2 deficiency prevents diabetic pericyte loss. In mice with excess levels of retinal ANG-2, pericyte dropout is exaggerated.
According to recent data, Ang-2 transcription is modified by hyperglycaemia-induced biochemical alterations, resulting in increased Ang-2 expression [14]. When diminished pericyte protection of endothelial cells and cumulative damage from diabetic oxidative stress culminate in progressive vascular occlusion, either new vessels form or the progressive leakage through the defective blood–brain barrier results in macula oedema. Both of these late complications involve ischaemia-induced growth factors such as VEGF [15, 16]. Recently, erythropoietin has been identified as another important angiogenic factor, since vitreous levels of erythropoietin in patients with proliferative diabetic retinopathy were significantly higher than in non-diabetic patients. Furthermore, multivariate logistic regression analysis revealed that erythropoietin is more closely associated with proliferative diabetic retinopathy than is VEGF [17, 18]. Like VEGF, erythropoietin stimulates angiogenesis in vitro and in vivo, and promotes endothelial cell and neuronal cell survival. Erythropoietin inhibition reduces retinal neovascularisation in an animal model of proliferative retinopathy and inhibits endothelial cell proliferation in vitro [19]. Treatment with erythropoietin at a dose inducing erythropoiesis is beneficial not only for retinal vessels, but also for retinal neuron survival [20–23].
Traditionally viewed as a haemopoietic growth factor regulating proliferation, differentiation and survival of erythroid progenitor cells, erythropoietin has several other functions including prevention of apoptosis in ischaemia–reperfusion and facilitation of tissue regeneration [24, 25]. These protective effects were found in a variety of organs such as heart, kidney, liver, brain and bone [26]. Furthermore, erythropoietin signalling stimulates protein kinase B (AKT) phosphorylation, an activation step that is reversed by methylglyoxal modification, on which retinal vascular cells attach [27]. In addition to its dose-dependent increase in haematocrit, which may be detrimental for microcirculatory perfusion in ischaemic situations, erythropoietin facilitates functional recovery through stimulation of neurogenesis and angiogenesis [28]. However, high erythropoietin dosage may be inadequate in a diabetic model because of the erythropoietic effect. For long-term use of erythropoietin, it is critical to avoid erythropoietic doses. As demonstrated earlier, doses as low as 0.1 µg/kg body weight successfully prevented organ damage in a 5/6 nephrectomy model over 6 weeks [29].
In this study, we aimed to determine the potential beneficial effects of suberythropoietic dosage of erythropoietin on oxidative stress in target tissues of diabetic complications. We also aimed to define the feasibility of further long-term suberythropoietic application of epoetin delta, a human cell-derived erythropoiesis-stimulating agent, and its impact on early vascular changes in the diabetic retina.
Methods
The study was performed in accordance with the Association for Research in Vision and Ophthalmology (ARVO) statement for the use of animals in ophthalmic and vision research. All animal work was approved by the local ethics committee (Regierungspräsidium, Karlsruhe, Germany).
Animals, diabetes induction and epoetin delta treatment
Male 6-week-old Wistar rats (Harlan Winkelmann, Borchen, Germany) were rendered diabetic by i.v. injection of 55 mg/kg body weight streptozotocin (Roche Diagnostics GmbH, Mannheim, Germany). Glucose levels and body weight were monitored consecutively throughout the study. HbA1c was determined at the end of the study using an analyser (Micromat II; Bio-Rad Laboratories, Hercules, CA, USA). Rats with a blood glucose level above 14 mmol/l at 1 week after streptozotocin injection were considered diabetic. Once diabetes was established, rats were randomly assigned to epoetin delta treatment (CN655918.5; Shire Pharmaceutical Contracts, Basingstoke, UK). Based on unpublished pilot experiments, we administered a total weekly dose of 384 IU using two different i.p. injection frequencies over 3 months. The first, the low-frequency group, received 384 IU/kg body weight once weekly; the second, the high-frequency group, had three injections a week at 128 IU/kg body weight. Body weight was controlled every 2 weeks throughout the study. Blood glucose concentrations were measured weekly during the first month after diabetes induction using an analyser (ACCU Check Comfort, no. 63877; Roche Diagnostics GmbH, Mannheim, Germany). After 1 month of diabetes, blood glucose levels were assessed every 2 weeks. Age-matched rats that had not received streptozotocin served as non-diabetic controls. At the end of the experiments, 22 serum samples were collected for the antibody formation assay. Eyes, kidneys and hearts were removed from deeply anaesthetised animals, frozen in liquid nitrogen and stored at −80°C.
In a further set of experiments, streptozotocin-induced diabetic Wistar rats were treated with epoetin delta at a dose (i.p.) of 256 IU/kg body weight three times per week over 3 months. After 4 weeks, eyes were obtained to assess Ang-2 (also known as Angpt2) gene expression. After 3 months, the effect of epoetin delta on the following was determined in the retina: AGE formation, glial activation, heat shock protein (HSP)-27 levels, activation of AKT and pericyte loss.
Measurement of erythropoiesis
Blood cell count was performed automatically using a haematoanalyser (CellDyn 3500; Abbott GmbH & Co. KG, Wiesbaden, Germany). EDTA-anticoagulated blood (200 µl) was collected from tail veins and measured undiluted or in a 1:2-dilution with Dulbecco’s PBS (PAA Laboratories GmbH, Pasching, Germany).
Counting of erythrocytes and the determination of erythrocyte mean corpuscular volume (MCV) was performed by the impedance method in a single measurement chamber. Haematocrit was calculated automatically using the erythrocyte-counts and MCV values according to the following equation: haematocrit = (erythrocytes × MCV)/10. Haemoglobin values were measured photometrically at 540 nm in a flow cell by the modified cyanmethaemoglobin method.
Determination of antibody formation against epoetin delta
Serum samples were collected at the end of 3 months and were tested for the presence of antibodies against epoetin delta using an ELISA (MAB287; R&D Systems, Minneapolis, MN, USA). Human erythropoietin was used at a concentration of 0.5 mg/ml as positive control. Control samples were further diluted prior to analysis to give concentrations on the assay plate of 500 ng/ml and 10 ng/ml for the high and low positive controls. All study samples were analysed in 1:10 and 1:100 dilutions. A mean value below the relevant plate cut point was considered to be negative, meaning that no drug-specific immune response was detectable.
Biomarkers of oxidative stress and AGE formation
To identify formation of oxidative and nitrosative stress markers, CML and nitrotyrosine protein were extracted from retina, kidney and heart, and processed as previously described [30]. The isolated individual retinas were homogenised in 200 µl lysis buffer, containing 25 mmol/l HEPES (pH 7.3), 10 mmol/l EDTA (pH 8.0), 10 mmol/l NaPP (Na4P2O7⋅10H2O), 10 mmol/l NaF, 125 mmol/l NaCl, 0.1% (wt/vol.) SDS, 0.5% (wt/vol.) desoxycholat, 1% (vol./vol.) Triton X-100 and 1× protease inhibitor mixture (Complete Mini; Roche Diagnostics, USA). After centrifugation for 15 min at 10,000×g and 4°C, the supernatant fraction was collected and protein concentrations were determined using the Bradford method (Bio-Rad Laboratories, Munich, Germany). Before immunoblotting, samples were separated on 10 to 20% linear gradient Tris–HCl gels (Bio-Rad Laboratories), then the protein was electrotransferred on to polyvinylidene difluoride membranes using a semi-dry blotting system at ∼0.7 mA/cm2 for 1.5 h. Thereafter, unspecific binding was blocked by incubation with 5% (wt/vol.) non-fat dry milk in TBS containing 0.1% Tween (Sigma-Aldrich, Steinheim, Germany) for CML and methylglyoxal, or with 1% (wt/vol.) BSA + 5% (vol./vol.) goat serum in TBS/T for nitrotyrosine. Membranes were incubated overnight with the following primary antibodies at 4°C: (1) mouse monoclonal nitrotyrosine (0.8 µg/ml in TBS/T; ALX-804-204, Alexis Biochemicals; Axxora Deutschland GmbH, Germany); (2) mouse monoclonal CML (1:10,000 in 5% milk in TBS/T [31]); and (3) methylglyoxal-H1 (1:2,000 in 5% milk in TBS/T [32]). After washing, the blots were incubated for 1 h at room temperature with horseradish peroxidase-conjugated goat anti-mouse secondary antibody diluted in 5% milk/TBS/T solution (1:3000, P0447; Dako Cytomation, Hamburg, Germany). Immunoreactive bands were visualised by incubation for 1 min in chemiluminescence reagent (Perkin Elmer, Boston, MA, USA), followed by development with autoradiography film (Amersham Hyperfilm MP; GE Healthcare Limited, Little Chalfont, Buckinghamshire, UK) in a processor system (X-OMAT 480 RA; Eastman Kodak, Rochester, NY, USA). Immune complex quantification was performed exactly as previously described [33].
Analysis of Ang-2 mRNA expression
Total RNA was extracted from retinas using Trizol (Invitrogen GmbH, Karlsruhe, Germany) according to the manufacturer’s protocol. After cDNA synthesis, cDNA was amplified using 16 µmol/l dNTPs (R0192; MBI Fermentas, Glen Burnie, MD, USA), 50 pg forward and reverse primer oligonucleotides, 1 unit Taq polymerase (GoTaq, M830B; Promega, Madison, WI, USA) and 1.2 mmol/l MgCl2 (A351H; Promega). PCR reactions were performed using a Thermocycler (Biometra, Göttingen, Germany) with the following protocol: denaturation 4 min at 94°C, followed by primer-specific number of cycles of amplification for 45 s at 94°C, 45 s at specific primer annealing temperature and 1 min at 72°C, with a final extension at 72°C for 10 min. The following primers were used: rat Ang-2 (180 bp, 55°C, 35 cycles), sense (5′-CTG AAG ATC CAG CTG AAG-3′) and antisense (5′-ATT GTC CGA ATC CTT TGT-3′); β-actin (416 bp, 58°C, 23 cycles), sense (5′-CCT GAA CCC TAA GGC CAA CCG-3′) and antisense (5′-GCT CAT AGC TCT TCT CCA GGG-3′). All amplified samples were separated on 1% (wt/vol., β-actin) or 1.5% (wt/vol., Ang-2) agarose gel electrophoresis. Ang-2 expression was calculated relative to expression of the housekeeping gene β-actin.
Imunohistochemical analysis
Antigen retrieval was performed on ocular paraffin sections (6 µm) by incubation in citrate buffer (glycerolgelatine and di-sodium hydrogen phosphate dihydrate) and heating in the microwave (2 × 5 min at 500 W and 2 × 5 min at 270 W). Afterwards sections were permeabilised and blocked in a 1% BSA/0.5% Triton-100/PBS solution for 30 min at room temperature. Primary antibodies rabbit anti-glial fibrillary acidic protein (GFAP) (1:200 in PBS; Dako Cytomation) and HSP-27 (1:50 in PBS, sc-1048; Santa Cruz Biotechnology, Heidelberg, Germany), or rabbit anti-rat p-AKT (1:25 in PBS; 9266; Cell Signaling, Frankfurt/Main, Germany) and rabbit anti-rat AKT (1:300 in PBS, 2938; Cell Signaling) were incubated overnight at 4°C. After washing, sections were incubated for 1 h with secondary antibody swine anti-rabbit FITC for GFAP, p-AKT and AKT (1:20 in PBS, F0205; Dako Cytomation) and chicken anti-goat Alexa Fluor 488 for HSP-27 (1:200 in PBS, A21467; Invitrogen) at room temperature. After washing, sections were mounted with 50% glycerol/PBS on glass slides and images were taken with a fluorescence microscope (DMRBE; Leica Microsystems, Wetzlar, Germany). The staining intensity was quantified using Image J software (National Institutes of Health, Bethesda, MD, USA). The intensity of non-diabetic was defined as 1, and the intensities of diabetic and epoetin delta-treated diabetic groups were expressed as the ratio normalised to the intensity of non-diabetic controls.
Retinal digests preparation and quantitative retinal morphometry
Quantitative retinal morphometry was performed in retinal digest preparations to evaluate capillary endothelial cell and pericyte numbers. In brief, eyes were fixed in 4% formaldehyde for at least 1 day. Next, retinas were isolated and incubated for 30 min in distilled water at 37°C, then digested for 2 to 3 h in 3% trypsin dissolved in 0.2 mol/l Tris–HCl (pH 7.4) solution at 37°C. After washing under a dissection microscope, the isolated retinal vasculature was dried on glass slides. Retinal digest preparations were stained with periodic acid–Schiff’s reagent [16] and Meyer’s haematoxylin (1:2; Merck, Darmstadt, Germany). Endothelial cell and pericyte numbers were quantified in ten randomly selected areas (magnification ×400) in a circular area of the middle third of the retina, using an image analysing system (CUE-2; Olympus Opticals, Hamburg, Germany). Cell numbers were calculated relative to the retinal capillary area (numbers of cells per mm2 of capillary area) of each quantified field by software (AnalySIS; Soft Imaging System, Muenster, Germany).
Statistical analysis
Data from all experiments are presented as mean ± SD. One-way ANOVA was used for statistical analysis. A p value of <0.05 was considered statistically significant.
Results
Epoetin delta treatment had no effect on metabolic control
Epoetin delta treatment with low-frequency dose (384 IU/kg once weekly) and with high-frequency dose (128 IU/kg three times a week) started from the second week after hyperglycaemia induction and had no effect on the decreased body weight observed in hyperglycaemic animals at the end of 3 months (diabetic 295 ± 23.0 g, diabetic low-frequency 315.6 ± 14.2 g, diabetic high-frequency 313.6 ± 19.2 g; Fig. 1a). Streptozotocin injection resulted in stable hyperglycaemia over the study period. The blood glucose levels in diabetic rats were five- to sixfold higher than in non-diabetic controls, which had levels below 8 mmol/l. Blood glucose levels were not altered by 3 months of epoetin delta treatment at low frequency, but a 20% reduction was observed at high-frequency treatment (non-diabetic 6.8 ± 1.2 mmol/l, diabetic 32.9 ± 0.7 mmol/l, diabetic low-frequency 33.3 ± 0.1 mmol/l, diabetic high-frequency 21.2 ± 4.6 mmol/l; Fig. 1b). HbA1c levels in diabetic groups were significantly increased compared with controls, but were not influenced by 3 months of epoetin delta treatment (non-diabetic 6.7 ± 0.6%, diabetic 15.5 ± 1.4%, diabetic low-frequency 15.4 ± 1.4%, diabetic high-frequency 14.0 ± 2.4%; p < 0.0001; Fig. 1c). Thus, the moderate reduction of blood glucose by erythropoietin given thrice weekly (high-frequency) is unlikely to have caused any of the biochemical changes observed (see below).
Epoetin delta has no effect on body weight (a), blood glucose (b) and HbA1c (c) levels. Wistar rats were divided into four groups: non-diabetic (N), diabetic (D), diabetic treated with low-frequency dose of epoetin delta (384 IU/kg once weekly; D + LF) and diabetic treated with high-frequency dose of epoetin delta (128 IU/kg three times a week; D+HF). Epoetin delta injection (i.p.) started from the second week of hyperglycaemia. a After 3 months, untreated and epoetin delta-treated diabetic rats had lower body weight than non-diabetic rats. b The blood glucose levels in hyperglycaemic animals were increased compared with non-diabetic controls. Epoetin delta treatment at low frequency did not affect the increased blood glucose level, but a reduction was observed with high-frequency treatment. *p < 0.05. White circles, non-diabetic; black circles, diabetic; white triangles, diabetic low-frequency; black triangles, diabetic high-frequency. c Diabetes for 3 months induced a significant increase of HbA1c level compared with non-diabetic. Epoetin delta did not influence HbA1c level. † p < 0.0001. Values are given as means ± SD. Animals used: non-diabetic n = 5; diabetic n = 4; diabetic low-frequency n = 6; diabetic high-frequency n = 7
Haematological variables were not changed after 3 months of epoetin delta treatment
The haematological variables haemoglobin, erythrocytes count and haematocrit were analysed in blood samples of non-diabetic, diabetic and diabetic rats treated with the two regimens of epoetin delta after 3 months to confirm that the administered dosage had been sub-erythropoietic. Levels of these variables remained stable over the entire observation period and were not influenced either by hyperglycaemia or by epoetin delta treatment (Fig. 2).
Epoetin delta did not change haematological variables of diabetic animals over 3 months of treatment. Haemoglobin (a), erythrocyte numbers (b) and haematocrit (c) were analysed in rat groups as follows: non-diabetic, diabetic, diabetic with low-frequency dose epoetin delta (384 IU/kg one weekly) and diabetic with high-frequency dose epoetin delta (128 IU/kg three times a week). White circles, non-diabetic; black circles, diabetic; white triangles, diabetic low-frequency; black triangles, diabetic high-frequency. a The haemoglobin levels of all groups analysed were comparable over the 3 months of epoetin delta treatment. b The numbers of erythrocytes were not changed by hyperglycaemia or by epoetin delta treatment. c The haematocrit levels were comparable in all groups analysed. Animals used: non-diabetic n = 5; diabetic n = 4; diabetic low-frequency n = 6; diabetic high-frequency n = 7
Epoetin delta treatment did not result in anti-epoetin delta antibody formation
Rats were monitored for the development of anti-epoetin delta antibodies. After 3 months of epoetin delta treatment with the same weekly dose, but with two application frequencies, anti-epoetin delta antibodies could not be detected in serum samples of non-diabetic, diabetic and both epoetin delta-treated groups (Table 1).
Antioxidative effect of epoetin delta in diabetic rats
Oxidative stress is considered to be a crucial contributor to the pathogenesis of diabetic retinopathy. To investigate whether epoetin delta had antioxidative effects in diabetic rats, we analysed CML-modified proteins as a general marker of hyperglycaemia-induced oxidative stress. As shown in Fig. 3a, the CML level was significantly increased in retinas of the diabetic group compared with the non-diabetic group after 3 months. Both treatment regimens with epoetin delta significantly reduced the hyperglycaemia-induced increase in CML levels (p < 0.05). In the kidney, the CML level was higher in the diabetic group than in the non-diabetic group, while the high-frequency treated group showed a significant reduction of CML levels compared with the untreated diabetic group (p < 0.05; Fig. 3b). Figure 3c shows the significantly increased CML level in the hearts of the diabetic group, which was normalised by both epoetin delta treatments (p < 0.05, p < 0.01).
Epoetin delta treatment reduced the oxidative stress induced by diabetes. The protein level of CML as a marker of oxidative stress was investigated in the retina (a), kidney (b) and heart (c) of rat groups as follows: non-diabetic (N), diabetic (D), diabetic with low-frequency dose epoetin delta (D+LF) and diabetic with high-frequency dose epoetin delta (D+HF). a Blot and bar graph showing that in retina the CML level was significantly increased in the diabetic group compared with the non-diabetic group. Both epoetin delta doses significantly reduced the increased CML level observed in hyperglycaemic animals. *p < 0.05. b The CML level was higher in the diabetic kidney than in non-diabetic kidney. The increased CML level in diabetic kidney was significantly reduced by high-frequency epoetin delta treatment. *p < 0.05. c The significantly increased CML level in the diabetic heart was normalised by both epoetin delta dosages. The level of GAPDH served as loading controls. *p < 0.05; **p < 0.01. Values are based on four different animals per group
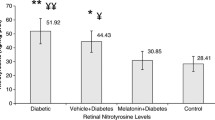
Nitrotyrosine develops as a consequence of peroxynitrite reaction with proteins and is therefore a marker of nitrosative stress. Nitrotyrosine levels were measured after 3 months in retina, kidney and heart samples from all groups. Hyperglycaemia resulted in increased nitrotyrosine levels in the retina, kidney and heart (p < 0.05; Fig. 4a–c). Low-frequency treatment resulted in a ∼16% reduction of nitrotyrosine levels compared with the untreated diabetic retina (p < 0.05; Fig. 4a), while high-frequency treatment normalised nitrotyrosine levels in the retina (p < 0.05; Fig. 4a). Figure 4b, c shows a significant reduction of nitrotyrosine levels by high-frequency treatment in diabetic kidney and heart samples (p < 0.05).
Epoetin delta reduces the level of nitrosative stress marker, nitrotyrosine (NT), in the diabetic retina (a), kidney (b) and heart (c) after 3 months of treatment. Organs of the following were analysed by western blot: non-diabetic (N), diabetic (D), diabetic with low-frequency epoetin delta dose (D+LF) and diabetic with high-frequency epoetin delta dose (D+HF). a Blot and bar graph showing that hyperglycaemia resulted in increased NT levels in the retina (*p < 0.05). Both epoetin delta doses significantly reduced NT levels after 3 months of treatment (*p < 0.05). b In the kidney, the NT level was significantly upregulated in the diabetic compared with the non-diabetic group (*p < 0.05). The high-frequency epoetin delta dose normalised the increased NT levels observed in the diabetic group (*p < 0.05). c High-frequency epoetin delta significantly reduced the NT level in the heart, which was significantly increased in diabetic compared non-diabetic rats (*p < 0.05). The level of GAPDH served as loading controls. Values are based on four animals for each group
Diabetes-induced increase of methylglyoxal levels in the retina after 3 months was reduced by epoetin delta
In this study, we analysed methylglyoxal levels in the retina after 3 months of epoetin delta treatment. The methylglyoxal level was significantly upregulated in the diabetic group compared with non-diabetic controls. Epoetin delta treatment at a dose of 256 IU/kg three times per week significantly reduced the hyperglycaemia-induced elevation of methylglyoxal levels (p < 0.05; Fig. 5).
Epoetin delta reduces hyperglycaemia-induced increases in methylglyoxal (MG) levels at 3 months in the retina. Methylglyoxal was analysed by western blot in diabetic retina after 3 months epoetin delta treatment at a dosage of 256 IU/kg body weight (three times a week). The methylglyoxal level was significantly increased in the diabetic group compared with non-diabetic control. Epoetin delta (EPO) significantly reduced the hyperglycaemia-induced upregulation of methylglyoxal (p < 0.05). Values are based on four different retinas per group
Hyperglycaemia-induced increase of Ang-2 levels was reduced in kidney after 3 months of epoetin delta treatment
It has been suggested that the ANG–TIE system is involved in diabetic pericyte loss. Ang-2, as a natural antagonist of Ang-1, is upregulated prior to pericyte loss in the diabetic retina. In this experiment, we assessed Ang-2 expression in animals treated with epoetin delta for 4 weeks and 3 months. After 4 weeks of hyperglycaemia, Ang-2 expression showed a trend towards upregulation in the retina. High-dose epoetin delta treatment (256 IU/kg three times a week) significantly reduced Ang-2 expression in the retina (p < 0.05; Fig. 6a). High-frequency and low-frequency epoetin delta treatment for 3 months did not alter retinal Ang-2 expression (Fig. 6b). After 3 months, Ang-2 expression was significantly upregulated in the diabetic kidney (p < 0.01; Fig. 6c), but was reduced by low-frequency epoetin delta treatment (p < 0.05; Fig. 6c). In heart tissue, Ang-2 expression was not changed by hyperglycaemia and was not influenced by 3 months of epoetin delta treatment (Fig. 6d).
Hyperglycaemia increases Ang-2 gene expression levels, which is reduced by epoetin delta treatment in the diabetic kidney. Ang-2 gene expression was assessed by semi-quantitative RT-PCR in the following rat groups: non-diabetic (N), diabetic (D), diabetic with low-frequency epoetin delta dose (D+LF), diabetic with high-frequency epoetin delta dose (D+HF) and diabetic with epoetin delta (256 IU/kg thrice weekly) (EPO). a In the retina, Ang-2 expression was upregulated in the diabetic group after 4 weeks. Epoetin delta treatment significantly reduced Ang-2 expression in the diabetic retina (*p < 0.05) after 4 weeks, an effect also observed as trend (b) after 3 months of epoetin delta treatment. c After 3 months, Ang-2 expression was significantly upregulated in the diabetic kidney (**p < 0.01) and was reduced by low-frequency epoetin delta treatment (*p < 0.05). d In the heart, Ang-2 gene expression was comparable in all groups analysed. Quantification was based on four different animals for each group
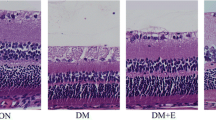
Epoetin delta treatment for 3 months reduced diabetes-induced HSP-27 levels and glial activation
It is known that the level of HSP-27 is upregulated under various conditions of stress, including oxidative stress, and that HSP-27 exhibits cytoprotective activity. In this study, double immunofluorescence staining for HSP-27 (green) and GFAP as a glial marker (red) was performed on retinal paraffin sections of non-diabetic and diabetic rats with and without epoetin delta treatment. Figure 7a shows the effect of 3 months of epoetin delta treatment (256 IU/kg body weight three times a week) on HSP-27 and GFAP levels. After 3 months, the staining intensity of GFAP was significantly greater in the diabetic retina than in that of non-diabetic controls (p < 0.001; Fig. 7b). Epoetin delta treatment significantly reduced GFAP levels (p < 0.05; Fig. 7b). The intensity of HSP-27 was also stronger in diabetic than in non-diabetic rat retinas (p < 0.01). This was modestly ameliorated by epoetin delta treatment.
Diabetes induces HSP-27 production and glial activation, an effect reduced by epoetin delta treatment. a Double immunofluorescence staining for HSP-27 (green) and GFAP as a glial marker (red) was performed on retinal paraffin sections of rat groups as follows: non-diabetic (N), diabetic (D) and diabetic with epoetin delta treatment (256 IU/kg body weight thrice weekly) (D+EPO). b Compared with the non-diabetic group (white bars), staining intensity of HSP-27 and GFAP was stronger in the diabetic (black bars) retina (**p < 0.01 and ***p < 0.001 respectively). The increased intensity of GFAP was ameliorated by epoetin delta treatment (hatched bars, *p < 0.05). Quantification was based on three different retinal sections of each group
Epoetin delta treatment induced phosphorylation of AKT after 3 months
It has been suggested that the activation of AKT by phosphoinositide-3-kinase results in inhibition of apoptotic signals and promotion of cell survival signals [34]. To investigate whether epoetin delta may induce AKT activation by phosphorylation (p-AKT), which is dominantly responsible for cytoprotection in oxidative stress, we assessed the levels of AKT and p-AKT in the retina of non-diabetic, diabetic and epoetin delta-treated groups. The staining intensity of total AKT was comparable in all groups. The intensity of p-AKT was decreased in the diabetic group at 3 months compared with the non-diabetic group. Epoetin delta treatment at a dosage of 256 IU/kg three times a week induced phosphorylation of AKT after 3 months of treatment (Fig. 8).
Epoetin delta treatment induces activation of Akt phosphorylation after 3 months of treatment. Levels of AKT and p-AKT were assessed on retinal paraffin sections of the following rat groups after 3 months: non-diabetic (N), diabetic (D), diabetic with epoetin delta treatment (256 IU/kg body weight thrice weekly; D+EPO, n = 1 animals for each group). The staining intensity of total AKT was comparable in all groups. AKT phosphorylation was decreased after 3 months of diabetes as compared with the staining intensity in non-diabetic rats. Epoetin delta treatment for 3 months induced the phosphorylation of AKT
Epoetin delta treatment reduced pericyte loss in the diabetic retina
In retinal digest preparations we investigated the effect of 3 months of epoetin delta treatment on early vascular changes in the diabetic retina. Cells were identified as pericytes by their characteristic protuberant position within the vascular bed, their darker nuclear staining and their typical morphology (Fig. 9a). In the diabetic retina, pericyte numbers were reduced by ∼9% compared with non-diabetic controls (non-diabetic vs diabetic 2,065 ± 71 vs 1,917 ± 152 pericytes per square millimetre capillary area; p < 0.05; Fig. 9b). Pericyte numbers were increased in the epoetin delta-treated group (256 IU/kg body weight three times a week) compared with the diabetic group (diabetic vs epoetin delta-treated group 1,917 ± 152 vs 2,048 ± 94 pericytes per square millimetre capillary area; p < 0.05; Fig. 9b). The numbers of endothelial cells were not changed by hyperglycaemia and were not affected by epoetin delta treatment (Fig. 9c).
Epoetin delta prevents the hyperglycaemia-induced loss of pericyte numbers in the diabetic retina after 3 months. Retinal digest preparations of non-diabetic (N), diabetic (D), and epoetin delta-treated diabetic (D+EPO) rats were used to quantify endothelial cells (EC) and pericyte (PC) numbers. a Retinal digest preparations of non-diabetic, diabetic and epoetin delta-treated groups. Arrows indicate pericytes in the capillaries. b Pericyte cell numbers per mm2 of capillary (cap.) area in the diabetic retina were reduced by ∼9% compared with non-diabetic controls (*p < 0.05). High-frequency epoetin delta increased pericyte numbers compared with the diabetic group (*p < 0.05). c The number of endothelial cells was not changed by hyperglycaemia or by epoetin delta treatment. Animals used: n = 5 (non-diabetic), n = 4 (diabetic) and n = 7 (epoetin delta-treated diabetic)
Discussion
Administration of suberythropoietic epoetin delta reduces oxidative stress in target tissues of diabetic complications, ameliorates prosurvival signals involving AKT and reduces the loss of pericytes in the diabetic retina.
Evidence for oxidative stress in eye, kidney and heart of diabetic individuals is strong [2, 35]. According to the unifying hypothesis, hyperglycaemia-induced mitochondrial overproduction of ROS induces PARP activation and excess methylglyoxal formation with subsequent substrate overflow due to polyribosylation-mediated inhibition of GAPDH [1, 32]. Our study and that of others are consistent in demonstrating that glycaemia and early glycation products are not affected by suberythropoietic erythropoietin doses [36]. Thus, the reduction of AGE and glycoxidation product formation is unrelated.
Erythropoietin can reduce oxidative stress via different mechanisms, acting as a direct and as an indirect antioxidant. As demonstrated earlier, small glycopolypeptides efficiently scavenge hydroxyl radicals, suggesting that erythropoietin reduces oxidative stress by reducing superoxide and other radicals. Furthermore, erythropoietin can induce glutathione peroxidase, which is downregulated in the diabetic retina [37, 38], thus improving the balance between pro- and antioxidative factors.
A third mechanism by which erythropoietin reduces oxidative stress is by stimulating AKT. Our data show that activation of p-AKT by erythropoietin treatment occurred predominantly in cells of the inner nuclear layer in the diabetic retina. Cells at this localisation belong to the neuroglia, but vascular cells may also be involved. In this context, Liu et al. demonstrated that methylglyoxal-modified matrix caused dephosphorylation of AKT in pericytes seeded on to the modified matrix [27]. Although speculative, a link between both reduced methylglyoxal formation and matrix modification and AKT phosphorylation of retinal cells is conceivable. In the diabetic kidney, erythropoietin exerts antioxidant properties by inhibiting renal activation and overexpression of NADPH oxidase [36]. A similar mechanism may be operative in other diabetic tissues.
Once hyperglycaemia-induced oxidative stress predominates, multiple changes in gene transcription activities ensue, leading to a complex re-arrangement of protective and deleterious mechanisms over time. Our observation that hyperglycaemia-induced upregulation of Ang-2 is reduced by erythropoietin treatment, together with the notion that pericytes are preserved in erythropoietin-treated diabetic rats, is consistent with recent data. Hyperglycaemia increases methylglyoxal formation and ANG-2 production [14, 39]. A link between elevated methylglyoxal and ANG-2 levels is suggested by the findings of Yao et al. that hyperglycaemia-induced formation of methylglyoxal modifies the transcriptional co-repressor (mSin3A), resulting in increased recruitment of O-linked N-acetylglucosamine transferase to an mSin3A-transcription factor specificity protein 3 (Sp3) complex and the subsequent increased modification of Sp3 by O-linked N-acetylglucosamine [14]. Modification of Sp3 by O-linked N-acetylglucosamine causes decreased binding of the repressor complex to the glucose-responsive GC-box in the ANG-2 promoter, increasing Ang-2 expression [16]. Our data suggest that erythropoietin treatment, by inhibiting methylglyoxal formation, reduces pericyte dropout via reduction of Ang-2 upregulation.
ANG-2 upregulation is part of a complex process involved in early pericyte loss of the diabetic retina. Pericyte loss is likely to result from various mechanisms such as apoptosis and pericyte migration. According to available data, the proportion of pericyte apoptosis contributing to total loss of pericytes may not exceed one third. Thus, pericyte migration can be a major factor contributing to pericyte loss. Pericyte migration is controlled by Ang-2 [40]. Since erythropoietin modifies both Ang-2 expression and apoptotic cell death, it is possible that erythropoietin preserves pericytes by two mechanisms. The question of whether erythropoietin affects pericyte apoptosis in diabetic rats needs further evaluation. Preliminary experiments using retinal digest preparations and Tunel staining did not reveal an increase in pericyte apoptosis (H.P. Hammes, Q. Wang and Y. Feng, unpublished observations).
Increasing cell stress in the diabetic retina causes multiple changes, also in the transcriptome of the neuroglia. One general indicator of retinal astrogliosis is GFAP, which is produced in astrocytes of the normal retina. In diabetes, GFAP is upregulated in glial Müller cells [41]. Among the genes activated in the diabetic retina are those encoding small HSPs. For example, HSP-31 abundance was found in Müller cells of the diabetic retina, in the vicinity of capillaries of the deep plexus [11, 42]. HSP-27 is a small HSP regulated by cellular stress. For example, in rat retinal ischaemia models, HSP-27 is upregulated and the protection of retina from ischaemia–reperfusion stress is accompanied by a reduction in HSP-27 [43]. In our experiments, we found HSP-27 colocalised with GFAP in the inner retina up to the inner nuclear layer, suggesting that astrocytes and Müller cells produced HSP-27 upon stress. Interestingly, the production was reduced by erythropoietin treatment, consistent with experiments in which the alleviation of stress is associated with a reduction in the cell stress protective gene.
The use of a suberythropoietic erythropoietin doses has the advantage of avoiding undesired side-effects associated with chronic treatment. One effect of high-dose treatment is the induction of angiogenesis. In patients undergoing renal replacement therapy because of end-stage diabetic nephropathy, erythropoietin treatment leads to an increased incidence of proliferative diabetic retinopathy [17]. Experimentally, high-dose erythropoietin promotes retinal proliferations in an acute mouse model of proliferative retinopathy, when administered in the presence of high VEGF levels [44]. However, VEGF levels during the early period of experimental diabetic retinopathy were not increased until several months of disease.
Together, our data suggest that suberythropoietic administration of erythropoietin over an extended period of time reduces oxidative stress in target tissues of diabetic complications and prevents pericyte loss in the diabetic retina. The results reported here need to be further validated in long-term studies and confirmed by use of larger animal numbers.
Abbreviations
- AKT:
-
Protein kinase B
- ANG:
-
Angiopoietin
- CML:
-
N ε-Carboxymethyl-lysine
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GFAP:
-
Glial fibrillary acidic protein
- HSP:
-
Heat shock protein
- MCV:
-
Mean corpuscular volume
- mSin3A:
-
Transcriptional co-repressor
- PARP:
-
Poly-ADP-ribose polymerase
- ROS:
-
Reactive oxygen species
- Sp3:
-
Transcription factor specificity protein 3
- VEGF:
-
Vascular endothelial growth factor
References
Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54:1615–1625
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820
Bierhaus A, Nawroth PP (2009) Multiple levels of regulation determine the role of the receptor for AGE (RAGE) as common soil in inflammation, immune responses and diabetes mellitus and its complications. Diabetologia 52:2251–2263
Coughlan MT, Thorburn DR, Penfold SA et al (2009) RAGE-induced cytosolic ROS promote mitochondrial superoxide generation in diabetes. J Am Soc Nephrol 20:742–752
Obrosova IG, Minchenko AG, Vasupuram R et al (2003) Aldose reductase inhibitor fidarestat prevents retinal oxidative stress and vascular endothelial growth factor overexpression in streptozotocin-diabetic rats. Diabetes 52:864–871
Karachalias N, Babaei-Jadidi R, Ahmed N, Thornalley PJ (2003) Accumulation of fructosyl-lysine and advanced glycation end products in the kidney, retina and peripheral nerve of streptozotocin-induced diabetic rats. Biochem Soc Trans 31:1423–1425
Januszewski AS, Alderson NL, Metz TO, Thorpe SR, Baynes JW (2003) Role of lipids in chemical modification of proteins and development of complications in diabetes. Biochem Soc Trans 31:1413–1416
Friess U, Waldner M, Wahl HG et al (2003) Liquid chromatography-based determination of urinary free and total N(epsilon)-(carboxymethyl)lysine excretion in normal and diabetic subjects. J Chromatogr B Analyt Technol Biomed Life Sci 794:273–280
Zheng L, Kern TS (2009) Role of nitric oxide, superoxide, peroxynitrite and PARP in diabetic retinopathy. Front Biosci 14:3974–3987
Pacher P, Obrosova IG, Mabley JG, Szabo C (2005) Role of nitrosative stress and peroxynitrite in the pathogenesis of diabetic complications. Emerging new therapeutical strategies. Curr Med Chem 12:267–275
Hammes HP, Bartmann A, Engel L, Wulfroth P (1997) Antioxidant treatment of experimental diabetic retinopathy in rats with nicanartine. Diabetologia 40:629–634
Song JH, Miyazawa T (2001) Enhanced level of n-3 fatty acid in membrane phospholipids induces lipid peroxidation in rats fed dietary docosahexaenoic acid oil. Atherosclerosis 155:9–18
Lieberthal W, Levine JS (2009) The role of the mammalian target of rapamycin (mTOR) in renal disease. J Am Soc Nephrol 20:2493–2502
Yao D, Taguchi T, Matsumura T et al (2007) High glucose increases angiopoietin-2 transcription in microvascular endothelial cells through methylglyoxal modification of mSin3A. J Biol Chem 282:31038–31045
Frank RN (2004) Diabetic retinopathy. N Engl J Med 350:48–58
Aiello LP, Avery RL, Arrigg PG et al (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Watanabe D, Suzuma K, Matsui S et al (2005) Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. N Engl J Med 353:782–792
Spinowitz BS, Pratt RD, Epoetin Delta 2002 Study Group (2006) Epoetin delta is effective for the management of anaemia associated with chronic kidney disease. Curr Med Res Opin 22:2507–2513
Watanabe D (2007) Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. Nippon Ganka Gakkai Zasshi 111:892–898 (article in Japanese)
Rabie T, Marti HH (2008) Brain protection by erythropoietin: a manifold task. Physiology (Bethesda) 23:263–274
Brines M, Grasso G, Fiordaliso F et al (2004) Erythropoietin mediates tissue protection through an erythropoietin and common beta-subunit heteroreceptor. Proc Natl Acad Sci USA 101:14907–14912
Chong ZZ, Kang JQ, Maiese K (2002) Erythropoietin is a novel vascular protectant through activation of Akt1 and mitochondrial modulation of cysteine proteases. Circulation 106:2973–2979
Zhang J, Wu Y, Jin Y et al (2008) Intravitreal injection of erythropoietin protects both retinal vascular and neuronal cells in early diabetes. Invest Ophthalmol Vis Sci 49:732–742
Brines M, Cerami A (2005) Emerging biological roles for erythropoietin in the nervous system. Nat Rev Neurosci 6:484–494
Brines M, Cerami A (2006) Discovering erythropoietin’s extra-hematopoietic functions: biology and clinical promise. Kidney Int 70:246–250
Rezaeian F, Wettstein R, Amon M et al (2008) Erythropoietin protects critically perfused flap tissue. Ann Surg 248:919–929
Liu B, Bhat M, Padival AK, Smith DG, Nagaraj RH (2004) Effect of dicarbonyl modification of fibronectin on retinal capillary pericytes. Invest Ophthalmol Vis Sci 45:1983–1995
Villa P, van Beek J, Larsen AK et al (2007) Reduced functional deficits, neuroinflammation, and secondary tissue damage after treatment of stroke by nonerythropoietic erythropoietin derivatives. J Cereb Blood Flow Metab 27:552–563
Bahlmann FH, Song R, Boehm SM et al (2004) Low-dose therapy with the long-acting erythropoietin analogue darbepoetin alpha persistently activates endothelial Akt and attenuates progressive organ failure. Circulation 110:1006–1012
Kowluru RA, Chan PS (2007) Oxidative stress and diabetic retinopathy. Exp Diabetes Res 2007:43603
Hammes HP, Alt A, Niwa T et al (1999) Differential accumulation of advanced glycation end products in the course of diabetic retinopathy. Diabetologia 42:728–736
Shinohara M, Thornalley PJ, Giardino I et al (1998) Overexpression of glyoxalase-I in bovine endothelial cells inhibits intracellular advanced glycation endproduct formation and prevents hyperglycemia-induced increases in macromolecular endocytosis. J Clin Invest 101:1142–1147
Hammes HP, Du X, Edelstein D et al (2003) Benfotiamine blocks three major pathways of hyperglycemic damage and prevents experimental diabetic retinopathy. Nat Med 9:294–299
Nunez G, del Peso L (1998) Linking extracellular survival signals and the apoptotic machinery. Curr Opin Neurobiol 8:613–618
Chiu J, Xu BY, Chen S, Feng B, Chakrabarti S (2008) Oxidative stress-induced, poly(ADP-ribose) polymerase-dependent upregulation of ET-1 expression in chronic diabetic complications. Can J Physiol Pharmacol 86:365–372
Toba H, Sawai N, Morishita M et al (2009) Chronic treatment with recombinant human erythropoietin exerts renoprotective effects beyond hematopoiesis in streptozotocin-induced diabetic rat. Eur J Pharmacol 612:106–114
Obrosova IG, Drel VR, Kumagai AK, Szabo C, Pacher P, Stevens MJ (2006) Early diabetes-induced biochemical changes in the retina: comparison of rat and mouse models. Diabetologia 49:2525–2533
Genc S, Akhisaroglu M, Kuralay F, Genc K (2002) Erythropoietin restores glutathione peroxidase activity in 1-methyl-4-phenyl-1,2,5,6-tetrahydropyridine-induced neurotoxicity in C57BL mice and stimulates murine astroglial glutathione peroxidase production in vitro. Neurosci Lett 321:73–76
Lin J, Bierhaus A, Bugert P et al (2006) Effect of R-(+)-alpha-lipoic acid on experimental diabetic retinopathy. Diabetologia 49:1089–1096
Pfister F, Feng Y, vom Hagen F et al (2008) Pericyte migration: a novel mechanism of pericyte loss in experimental diabetic retinopathy. Diabetes 57:2495–2502
Hammes HP, Federoff HJ, Brownlee M (1995) Nerve growth-factor prevents both neuroretinal programmed cell-death and capillary pathology in experimental diabetes. Mol Med 1:527–534
Koistinaho J, Miettinen S, Keinanen R, Vartiainen N, Roivainen R, Laitinen JT (1996) Long-term induction of haem oxygenase-1 (HSP-32) in astrocytes and microglia following transient focal brain ischaemia in the rat. Eur J Neurosci 8:2265–2272
Schmeer C, Gamez A, Tausch S, Witte OW, Isenmann S (2008) Statins modulate heat shock protein expression and enhance retinal ganglion cell survival after transient retinal ischemia/reperfusion in vivo. Invest Ophthalmol Vis Sci 49:4971–4981
Chen J, Connor KM, Aderman CM, Smith LE (2008) Erythropoietin deficiency decreases vascular stability in mice. J Clin Invest 118:526–533
Acknowledgements
This study was supported by Shire Pharmaceuticals, the German Diabetes Association and the Deutsche Forschungsgemeinschaft. Q. Wang, F. Pfister and F. Vom Hagen are present or former graduate students of the international research training group (GRK 880 Vascular Medicine) at Deutsche Forschungsgemeinschaft. The excellent technical help of P. Bugert, N. Dietrich, U. Kaiser and V. Schwarz is greatly appreciated.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Q., Pfister, F., Dorn-Beineke, A. et al. Low-dose erythropoietin inhibits oxidative stress and early vascular changes in the experimental diabetic retina. Diabetologia 53, 1227–1238 (2010). https://doi.org/10.1007/s00125-010-1727-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1727-7