Abstract
Aims/hypothesis
The aims of this work were to determine the effect of hypothyroidism on insulin-stimulated glucose turnover and to unravel the potential mechanisms involved in such an effect.
Methods
Hypothyroidism was induced by administration of propylthiouracil, with partial T4 substitution. Euglycaemic–hyperinsulinaemic clamps, associated with the labelled 2-deoxy-d-glucose technique for measuring tissue-specific glucose utilisation, were used. To assess a possible involvement of leptin in the modulation of glucose metabolism by hypothyroidism, leptin was infused intracerebroventricularly for 6 days. A group of leptin-infused rats was treated with rT3 to determine a potential role of T3 in mediating the leptin effects.
Results
Compared with euthyroid rats, hypothyroid animals exhibited decreased overall glucose turnover and decreased glucose utilisation indices in skeletal muscle and adipose tissue. Leptinaemia in hypothyroid rats was lower while resistin mRNA expression in adipose tissue was higher than in euthyroid animals. Intracerebroventricular leptin infusion in hypothyroid rats partially restored overall, muscle and adipose tissue insulin-stimulated glucose utilisation and improved the reduced glycaemic response observed during insulin tolerance tests. The leptin effects were due neither to the observed increase in plasma T3 levels nor to changes in the high adipose tissue resistin expression of hypothyroid rats. The administration of leptin to hypothyroid animals was accompanied by increased expression of muscle and adipose tissue carnitine palmitoyl transferases, decreased plasma NEFA levels and reduced muscle triglyceride content.
Conclusions/interpretation
Hypothyroidism is characterised by decreased insulin responsiveness, partly mediated by an exaggerated glucose–fatty acid cycle that is partly alleviated by intracerebroventricular leptin administration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid hormones are known to play a role in the regulation of basal metabolic rate, and in the stimulation of thermogenesis [1, 2]. They have also been shown to influence lipid metabolism, favouring lipolysis and providing fatty acids as fuels for the induction of energy expenditure [3]. With regard to glucose metabolism, the effects of thyroid hormones have been primarily studied in vitro. Thus, several investigations have demonstrated a stimulatory effect of T3 on insulin-stimulated glucose transport and/or phosphorylation in muscle [4, 5], on the insulin-sensitive muscle/fat glucose transporter, GLUT4 [4, 6], and on glycolysis in isolated muscle [5]. Other data showed decreased insulin-stimulated glucose transport and/or phosphorylation, as well as a lower rate of glycolysis in isolated muscles from hypothyroid animals, as induced by propylthiouracil (PTU) administration [5, 7]. Similar findings were obtained when studying isolated adipocytes from hypothyroid patients, as these cells exhibited decreased insulin responsiveness with regard to glucose utilisation. In this latter study, thyroid hormone concentrations were shown to be positively correlated with the insulin responsiveness of the adipocytes [8].
In vivo data pertaining to the effects of thyroid hormone excess or of hypothyroidism on glucose metabolism appear to be less numerous and are complex in their interpretation. Indeed, hypothyroid patients are usually reported to be glucose intolerant [9], but glucose intolerance is also observed in hyperthyroidism (for review, see [10]). PTU-induced hypothyroidism in sheep was shown to result in insulin resistance, as tested during euglycaemic–hyperinsulinaemic clamps [11].
Leptin is another hormone playing a major role in the regulation of energy balance by modulating food intake, thermogenesis, as well as glucose and lipid metabolism [12, 13]. Regarding possible interactions between thyroid hormones and leptin, the influence of the thyroid function, and of hypothyroidism in particular, on circulating leptin levels provided conflicting data. Thus, decreases [14–16], increases [17–19] or no change [20, 21] in leptinaemia were reported in hypothyroid patients. Such divergent results may be explained by the fact that leptin levels primarily reflect changes in fat mass, this parameter varying according to sex, age and duration of hypothyroidism.
Leptin has been shown to stimulate the hypothalamo–pituitary–thyroid axis, a stimulation that was particularly evident when studying animals during food restriction [22–27]. We have shown, in particular, that leptin produced an increase in plasma T3 levels that was due to a stimulation of both the hepatic deiodinase type 1 (D1) and the brown adipose tissue deiodinase type 2 (D2) [25, 27]. As reviewed in [13], we and other investigators also reported that leptin increased glucose metabolism in muscle and brown adipose tissue [28], effects that appeared to be centrally mediated [29].
On the basis of the studies summarised above, it could be envisioned that T3 and leptin may act in a coordinated manner to favour carbohydrate and lipid utilisation, thereby contributing to the maintenance of normal metabolic homeostasis.
Given this background, the present studies aimed to: (1) determine the impact of hypothyroidism on insulin-mediated glucose turnover, as measured in vivo during euglycaemic–hyperinsulinaemic clamps and during insulin tolerance tests; and (2) unravel a potential role of leptin in the metabolic consequences of hypothyroidism.
Materials and methods
Animals
Eight- to nine-week-old 175- to 200-g male Wistar rats purchased from BRL (Basle, Switzerland) were housed under conditions of controlled temperature (23°C) and illumination (07.00–19.00 h). They were allowed access to water and standard laboratory chow (Provimi Lacta, Cossonay, Switzerland) until they were included into the protocol described below.
The animals studied were either euthyroid or mildly hypothyroid, as previously described and validated [27]. Briefly, the mild hypothyroid group was obtained by giving PTU (Fluka Chemie, Buchs, Switzerland) in the drinking water of normal rats at a dose of 0.025% for 3 weeks. During the last week of this experimental period, the PTU-treated animals were supplemented with a daily i.p. injection of T4 (0.6 nmol·100 g body weight−1·day−1) for 3 days, followed by a 3-day continuous T4 infusion (0.6 nmol·100 g body weight−1·day−1) using subcutaneously implanted osmotic minipumps (Model 2001; Alza Corporation, Palo Alto, CA, USA). Dosage of the administered T4 was chosen based on preliminary experiments and aimed to produce a state of moderate hypothyroidism.
All procedures used were approved by the “Office Vétérinaire Fédéral et Cantonal”, Geneva, Switzerland.
Implantation of cannula in the lateral cerebral ventricle
Animals were anaesthetised with intramuscular ketamine–xylazine used at 45 and 9 mg/kg, respectively (Parke-Davis and Bayer, Leverkusen, Switzerland), and equipped with a cannula positioned in the right lateral cerebral ventricle (i.c.v.). After 1 week of recovery, subcutaneously implanted osmotic minipumps delivering the vehicle or leptin were connected to the i.c.v. infusion cannula via a polyethylene catheter, as previously described [30]. Minipumps (Model 2001; Alza Corporation, Palto Alto, CA, USA) infused either isotonic saline (vehicle), or 10 μg of leptin ([Ala-100] hleptin, a human leptin analogue provided by Eli Lilly and Company, Indianapolis, IN, USA) per day for 6 days.
One of the leptin-infused hypothyroid group was additionally infused with reverse T3 (rT3) given subcutaneously by minipumps for the last 3 days of the experiment (25 nmol·100 g body weight−1·day−1). Given the inhibitory effect of PTU on type 1 deiodinase [31] and the fact that rT3 inhibits type 2 deiodinase activity [27, 32, 33], i.c.v. leptin-infused rats treated with rT3 were deficient in both type 1 and type 2 deiodinase activities.
Feeding conditions of animals
All the animals throughout this study had the same food intake for the following reasons: (1) one of the aims of the study was to investigate the metabolic effects of i.c.v. leptin infusion in hypothyroid rats; (2) central leptin infusion results in decreased food intake; and (3) valid comparisons of metabolic data require the presence of similar intergroup food intakes. This was achieved by supplying groups of euthyroid and hypothyroid rats with the same amount of food as that actually consumed by the respective leptin-infused animals (pair-feeding). Thus, and as shown in Table 1, food intake of hypothyroid and euthyroid pair-fed animals was similarly reduced by 38 to 42% compared with that of the respective ad-libitum-fed groups. Pair-feeding of euthyroid and hypothyroid rats was accompanied by a loss in body weight that was of the same magnitude as that produced by leptin in hypothyroid animals.
In the present studies, comparisons of metabolic parameters were made between euthyroid pair-fed and hypothyroid pair-fed rats, and between hypothyroid pair-fed and i.c.v. leptin-infused rats, treated or not with rT3.
Euglycaemic–hyperinsulinaemic clamps
Euglycaemic–hyperinsulinaemic clamps were carried out in 5-h fasted euthyroid or mildly hypothyroid rats. In the first series of experiments on euthyroid vs hypothyroid animals, the glucose infusion rate (GIR) needed to maintain normoglycaemia at the same level of imposed hyperinsulinaemia was determined and compared. At the end of these euglycaemic–hyperinsulinaemic clamps, a bolus of 2-deoxy-d-[1-3H]glucose (2-DG; 1.110 MBq/rat; Amersham, Aylesbury, UK) was injected i.v. to measure the in vivo insulin-stimulated glucose utilisation index of muscles (red quadriceps) and white adipose tissue (epididymal fat), as previously described [34, 35]. The tissues mentioned were freeze-clamped for further analysis. In other groups of euthyroid and hypothyroid animals, as well as of hypothyroid leptin-infused rats treated or not with rT3, the rates of total glucose utilisation (rate of glucose disappearance, Rd) and of hepatic glucose production (rate of glucose appearance, Ra) were determined during euglycaemic–hyperinsulinaemic clamps with an infusion of d-[U-14C]glucose (1.850 MBq/rat; Amersham, Aylesbury, UK), according to a method previously described [36]. At the end of these clamps, muscle and adipose tissue insulin-stimulated glucose utilisation indices were determined with the 2-DG technique mentioned above.
Analytical procedures related to the clamp studies
Two-deoxy-d-[1-3H]-glucose- and d-[U-14C]-glucose-specific activities were determined in deproteinised blood samples as previously reported [34, 35]. Measurement of tissue concentrations of 2-DG-6-phosphate allowed us to calculate the in vivo glucose utilisation index by individual tissues, and was expressed in ng·min−1·mg tissue−1 [34, 35].
Insulin tolerance tests
Other groups of euthyroid rats, hypothyroid rats and hypothyroid leptin-infused animals were treated as those mentioned above. On day 4, all the animals were subjected to an insulin tolerance test. Insulin (Actrapid HM, 100 IE·U−1·ml−1; Novo Nordisk, Bagsvaerd, Denmark) was given i.p. at a dose of 0.75 U/kg and blood samples were taken from the tip of the tail at the time points 0, 15, 30, 60 and 120 min for measurement of plasma glucose levels. Glucose areas over these 120-min test periods were calculated and compared.
Quantitative RT-PCR procedure
On day 6, the animals were killed by decapitation and various tissues were removed, freeze-clamped and stored at −70°C for subsequent measurements of mRNA expression of liver D1, adipose tissue resistin, adipose tissue and liver carnitine palmitoyl transferase 1α (CPT-1α), and muscle carnitine palmitoyl transferase 1β (CPT-1β) by real-time quantitative PCR (Lightcycler; Roche Diagnostics, Basle, Switzerland), and for determination of muscle triglyceride content.
Total RNA was extracted from frozen tissue samples using the Trizol reagent (Life Technologies, Gibco, BRL, Rockville, MD, USA). RNA integrity was assessed by performing a 1% agarose-gel electrophoresis in 1× TBE, and its concentration was determined by spectrophotometry. cDNA templates for RT-PCR were obtained using 2.5 μg of total RNA. Reverse transcription reaction was performed with random hexamers (Microsynth, Geneva, Switzerland), dNTPs, the RNAse inhibitor, Rnasin (Catalys, Promega Corporation, Madison, WI, USA), and the M-MLV-RT enzyme kit (Life Technologies).
Amplification of cyclophilin A, D1, resistin, CPT-1α and CPT-1β cDNAs was performed with the SYBR Green I DNA master kit (Roche Diagnostics, Mannheim, Germany), according to the light cycler standard protocol, using around 70 ng of template cDNA. All primers were used at a final concentration of 0.5 μmol/l. After each run, a relative quantification of the amplified PCR product in the different samples was performed. This was based on the relative comparison of the PCR products during the log–linear phase of the amplification process. A standard curve was used to obtain the relative concentration of the target gene and the results were corrected according to the concentration of cyclophilin, used as the housekeeping gene.
Primer sequences
Primers for rat cyclophilin A, D1, resistin, CPT-1α and CPT-1β were designed online with Primer 3 software (http://www-genome.wi.mit.edu/cgi-bin/primer/primer3_www.cgi) and synthesised by Microsynth (Balgach, Switzerland). The sequence and main characteristics of the primers used are provided in Table 2.
The adequacy of the different PCR products was verified by nucleic acid sequencing and agarose gel electrophoresis.
Muscle triglyceride content
For the determination of triglyceride content in skeletal muscle (tibialis), weighed quantities of frozen tissue were powdered under liquid N2 and extracted overnight at 4°C in 6 ml chloroform : methanol (2:1 v/v), after which 1 mol/l H2SO4 was added and the solution was centrifuged. Two millilitres of the lower organic phase were removed and evaporated under N2 [37]. The resulting pellet was resuspended in 200 μl assay buffer, and triglyceride content was determined by colorimetric enzymatic analysis (BioMérieux, Marcy-l’Etoile, France).
Basal levels of plasma metabolites and hormones
Plasma glucose was measured by the glucose oxidase method (glucose analyser 2; Beckman Coulter, Fullerton, CA, USA). Plasma NEFA concentrations were determined using a kit from Wako Chemicals (Neuss, Germany), triglycerides with a kit from Biomérieux (as above), plasma leptin levels by a commercial RIA kit for rat leptin (Linco Research, St Louis, MO, USA), and plasma insulin levels by a RIA described previously [38]. Plasma T4 levels were measured using a commercial RIA kit (Immulite 2000; Diagnostic Product Corporation, Los Angeles, CA, USA), plasma T3 levels by an in-house method of Rotterdam (Erasmus University, Rotterdam, The Netherlands) with 2% intra-assay and 6% interassay coefficients of variation. These measurements were performed on samples that were collected 5 h after food removal.
D2 was measured in freshly prepared homogenates of brown adipose tissue, as previously described [27].
Statistical analysis
The results were analysed by one-way ANOVA followed by the Tukey’s procedure for multiple comparisons. The calculations were performed using the Sigma STAT software (SPSS, Chicago, IL, USA). A p value of less than 0.05 was considered statistically significant.
Results
As depicted in Table 3, the presence of hypothyroidism produced by PTU administration with partial T4 replacement (see “Materials and methods”) was substantiated by the occurrence of much higher TSH levels and lower T3 concentrations in hypothyroid than in euthyroid rats, whether they were fed ad libitum or pair-fed to the amount of food consumed by leptin-infused rats. Plasma T4 levels were not different in hypothyroid and euthyroid animals under both feeding conditions. Such effects of PTU on thyroid hormones were similar to those reported in humans [39, 40]. The state of hypothyroidism induced by PTU was also documented by the observation of a marked decrease in the mRNA expression of liver D1 (51.1±4.7 arbitrary units in hypothyroid pair-fed rats vs 100.0±14.2 arbitrary units in euthyroid pair-fed rats, p<0.001).
Overall and tissue-specific glucose utilisation indices were determined by performing euglycaemic–hyperinsulinaemic clamps associated with the labelled 2-DG technique. As mentioned in “Materials and methods”, comparisons were made between euthyroid and hypothyroid pair-fed animals, as these two groups had similar food intake and delta body weight changes (Table 1) allowing for valid interpretation of intergroup metabolic differences.
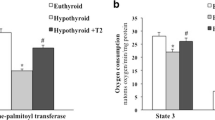
As depicted in Fig. 1, the GIR needed to maintain normoglycaemia during euglycaemic–hyperinsulinaemic clamps was markedly lower in hypothyroid rats than in euthyroid animals, indicating the presence of insulin resistance in hypothyroidism. The presence of decreased insulin responsiveness in hypothyroid rats was strengthened by measurements of tissue-specific glucose utilisation indices with the labelled 2-DG technique. Indeed, as shown in Fig. 2, both the insulin-stimulated glucose utilisation index of muscle (red quadriceps) and that of white adipose tissue (epididymal fat pad) from hypothyroid rats were markedly decreased, by more than 80% relative to values in euthyroid animals.
Glucose infusion rate (GIR) measured at the end of euglycaemic–hyperinsulinaemic clamps in euthyroid (open bar) and hypothyroid (black bar) pair-fed rats. Glycaemia measured at the end of euglycaemic–hyperinsulinaemic clamps was 6.0±0.2 mmol/l in euthyroid rats and 5.8±0.2 mmol/l in the hypothyroid group, NS. Insulinaemia was 22.2±1.1 and 20.3±2.6 ng/ml, NS. Similar GIR results were obtained when comparing euthyroid and hypothyroid animals that were fed ad libitum (21.5±0.8 and 16.3±1.6 mg·min−1·kg−1, respectively, p<0.05 at least). Means±SEM of five to six animals per group. *p<0.05 at least vs the euthyroid group
Insulin-stimulated glucose utilisation indices measured at the end of euglycaemic–hyperinsulinaemic clamps associated with the labelled 2-DG technique in muscle (red quadriceps) (a) and in epididymal white adipose tissue (b) in euthyroid (open bars) and hypothyroid (black bars) pair-fed rats. Similar results were obtained when comparing euthyroid and hypothyroid animals that were fed ad libitum (39.6±3.6 and 10.7±2.4 ng·min−1·kg−1, respectively, for red quadriceps, p<0.05 at least; 8.0±1.8 and 1.3±0.3 ng·min−1·kg−1, respectively, for epididymal white adipose tissue, p<0.05 at least). Means±SEM of six animals per group are shown. *p<0.05 at least vs the euthyroid group
In search of potential changes that could partly explain the hypothyroidism-induced decrease in insulin responsiveness, two observations were made, as shown in Fig. 3. The first was that, relative to euthyroid animals, plasma leptin levels were twofold lower in the hypothyroid group (Fig. 3a). The second was that adipose tissue mRNA expression of resistin more than doubled in the hypothyroid state (Fig. 3b). Additionally, and as shown in Table 4, plasma NEFA levels were higher in hypothyroid pair-fed than in euthyroid pair-fed rats, while plasma triglyceride concentrations were decreased by hypothyroidism. Glycaemia and insulinaemia were similar in the two groups of animals (Table 4).
The observed decrease in leptinaemia in hypothyroid rats led us to investigate the impact of i.c.v. leptin infusion on glucose turnover in the hypothyroid state. Insulin tolerance tests were performed in three groups of animals: euthyroid pair-fed rats, hypothyroid pair-fed rats and hypothyroid rats receiving i.c.v. leptin. As illustrated in Fig. 4, glucose areas during the 120-min test period were more than three times higher in hypothyroid than in euthyroid pair-fed rats, a defect that was partially corrected by i.c.v. leptin administration.
Glucose areas during insulin tolerance tests (ITT, 0.75 U/kg) performed on experimental day 4 in euthyroid pair-fed rats (open bar), hypothyroid pair-fed rats (black bar) and hypothyroid rats i.c.v. infused with leptin (hatched bar). Glucose areas were calculated during the 120 min of the tests. Means±SEM of five to eight animals per group are shown. *p<0.05 at least vs the euthyroid group; # p<0.05 at least vs the hypothyroid group
The Rd during euglycaemic–hyperinsulinaemic clamps was then assessed using 14C-labelled glucose as shown in Fig. 5. In keeping with the above-mentioned results of GIR and 2-DG in muscle and adipose tissue, Rd was lower in hypothyroid than in euthyroid rats. I.c.v. leptin infusion increased Rd while it did not modify the Ra (legend to Fig. 5). The observation that i.c.v. leptin infusion in hypothyroid rats resulted in increased plasma T3 levels compared with in hypothyroid rats (Table 3) led us to hypothesise that the beneficial effect of leptin on glucose utilisation might be partly mediated via T3. However, and as can be seen in Fig. 5, the stimulatory effect of leptin on Rd was still observed when i.c.v. leptin-infused hypothyroid rats were treated with rT3, a treatment preventing the leptin-induced increase in plasma T3 levels through an inhibition of D2 [27] (Table 3). Tissue-specific glucose utilisation indices were also increased by i.c.v. leptin administration to hypothyroid rats, both in muscle and in epididymal white adipose tissue, and whether or not the animals were treated with rT3 (Table 5).
Overall glucose utilisation rate (Rd) measured at the end of euglycaemic–hyperinsulinaemic clamps in euthyroid pair-fed rats (open bar), hypothyroid pair-fed rats (black bar), hypothyroid rats i.c.v. infused with leptin (hatched bar) and hypothyroid rats i.c.v. leptin-infused and treated with rT3 (grey bar). Basal hepatic glucose production was 5.3±0.5, 4.6±0.3, 4.6±0.7 and 5.6±0.5 mg·min−1·kg−1 for the euthyroid, the hypothyroid, the hypothyroid + leptin, and the hypothyroid + leptin + rT3 groups of rats, respectively (intergroup differences NS). Means±SEM of five to six animals per group are shown. *p<0.05 at least vs the euthyroid group; # p<0.05 at least vs the hypothyroid group
As shown in Table 4, the effect of leptin in ameliorating insulin responsiveness in hypothyroid rats was accompanied by decreases in plasma glucose, NEFA and triglyceride levels. In the presence of rT3, glycaemia was still lowered by i.c.v. leptin infusion, while the leptin effect on plasma triglycerides was no longer significant. Leptin infusion with or without rT3 did not have a significant effect on plasma insulin levels.
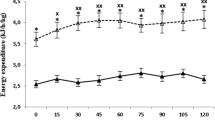
To explore the possibility that, under the present experimental conditions, leptin could favour fat utilisation in hypothyroid rats, CPT-1β expression in muscle, CPT-1α expression in white adipose tissue, and muscle triglyceride content were measured in untreated pair-fed and leptin-treated hypothyroid animals. As shown in Fig. 6a, leptin significantly increased the expression of both muscle CPT-1β and adipose tissue CPT-1α, without affecting liver CPT-1α (data not shown). Leptin also promoted a significant decrease in muscle triglyceride content (Fig. 6b).
Carnitine palmitoyl transferase 1β (CPT-1β) and 1α (CPT-1α) mRNA expression measured in muscle (tibialis) and in epididymal white adipose tissue (WATe) (a), and triglyceride (TG) content of tibialis muscle (b) of hypothyroid pair-fed rats (black bars) and hypothyroid rats i.c.v. infused with leptin (hatched bars). Means±SEM of seven animals per group are shown. *p<0.05 at least vs the hypothyroid group
Finally, it was observed that i.c.v. leptin infusion in hypothyroid rats did not modify the mRNA expression of adipose tissue resistin (100.0±11.7 arbitrary units in hypothyroid pair-fed rats and 123.2±26.1 arbitrary units in hypothyroid leptin-treated rats, n=7 and 8, respectively, NS).
Discussion
The purpose of this study was to investigate the consequences of mild hypothyroidism on glucose metabolism. Mild hypothyroidism was obtained by PTU administration to normal rats, followed by partial substitution of the animals with T4. Such mild hypothyroidism was characterised, relative to euthyroid animals, by high plasma TSH levels, low T3 concentrations and decreased mRNA expression of hepatic D1.
Under basal conditions, plasma glucose levels of hypothyroid rats were normal, and plasma insulin levels tended to be slightly but not significantly decreased, possibly reflecting an impairment of insulin secretion in hypothyroidism. When tested during euglycaemic–hyperinsulinaemic clamps, it was observed that the rate of glucose infusion needed to maintain normoglycaemia during euglycaemic–hyperinsulinaemic clamps was decreased by half in the hypothyroid group relative to the euthyroid one, indicating the presence of insulin resistance. This observation was corroborated by the finding that the insulin-stimulated glucose utilisation indices measured by the 2-DG method were six and 11 times lower in skeletal muscle and adipose tissue, respectively, in hypothyroid compared with euthyroid rats. These changes indicated the presence of decreased insulin responsiveness in hypothyroid animals, which is in keeping with the observed impaired glycaemic response during insulin tolerance tests.
In an attempt to unravel the causes of the decreased insulin responsiveness of hypothyroid animals, two parameters were determined in the hypothyroid and the euthyroid groups of rats. The first was basal plasma leptin levels, which were found to be markedly lowered in hypothyroid animals, possibly reflecting a decreased fat mass in these rats. Indeed, fat mass of hypothyroid animals was recently reported to be lower than that of euthyroid controls, although statistical significance was reached in the retroperitoneal fat pad only [41]. The second was resistin expression in adipose tissue whose levels were more than doubled in the hypothyroid group compared with in the euthyroid group. The decrease in plasma leptin levels is likely to have contributed to the decreased insulin responsiveness insofar as previous experiments have clearly shown that leptin administration to normal rats increases their insulin-mediated glucose metabolism [13, 28, 29]. In this respect, it is of interest to mention that decreased leptin levels have been observed in various models of lipodystrophy, in both humans and rodents, such models frequently exhibiting a state of insulin resistance [42–44].
The increased adipose tissue expression of resistin measured in hypothyroid animals is also likely to have contributed to the decreased insulin responsiveness of hypothyroid rats. Indeed, it is in keeping with in vitro and in vivo data of others showing that this adipose tissue-derived adipokine inhibits insulin-stimulated glucose utilisation in 3T3-L1 adipocytes [45] and skeletal muscle cells [46] while promoting hepatic insulin resistance [47]. Additionally, it has been reported that transgenic rodents overexpressing resistin in adipose tissue display impaired skeletal muscle glucose metabolism [48], a defect possibly related to the measured increase in plasma NEFA levels, and muscle triglyceride content. The result reported here showing a doubling of adipose tissue resistin mRNA expression in mild hypothyroidism is in keeping with other data showing that hyperthyroidism is accompanied by marked decreases in resistin mRNA expression in white adipose tissue, while hypothyroid rats exhibited a 40% increase in white adipose tissue resistin mRNA levels [49].
Amongst the two potential causes of insulin resistance in hypothyroid animals just mentioned (low leptin, high resistin), the role of the former was further investigated in the present study.
It was observed that i.c.v. leptin infusion in hypothyroid animals significantly increased their Rd. This finding was corroborated by the observations of significant leptin-elicited increases in the insulin-stimulated glucose utilisation of both muscle and adipose tissue, and by decreased glucose areas during insulin tolerance tests. The increase in glucose utilisation of the hypothyroid group administered with leptin was accompanied by the occurrence of hypoglycaemia, compared with the normal plasma glucose levels of untreated hypothyroid animals. Together, these data are in keeping with those of the literature showing that peripheral leptin administration as well as transgenic leptin overexpression are able to correct, at least in part, insulin resistance of human and rodent models of lipodystrophy [43, 50–52]. Similarly, insulin resistance and the diabetic state of young obese patients suffering from congenital leptin deficiency were shown to be corrected by peripheral leptin administration [53]. Finally, central leptin infusion was reported to improve insulin sensitivity in streptozotocin-induced diabetic rats exhibiting low plasma leptin levels due to the lack of adipose tissue [54].
Of additional interest was the observation that plasma NEFA levels were lowered by central leptin infusion in hypothyroid rats relative to untreated hypothyroid controls and that leptin concomitantly increased adipose tissue CPT1-α as well as muscle CPT1-β expression, thereby decreasing muscle triglyceride content.
Thus, leptin may have ameliorated the decreased insulin responsiveness of hypothyroid animals by both increasing lipid oxidation (increasing CPT expression, decreasing NEFA levels, decreasing muscle triglyceride content) and increasing overall glucose oxidation, all events that are potentially related to the alleviation of a potential exaggerated glucose–fatty acid cycle [55].
Leptin administration did not modify the mRNA overexpression of resistin in adipose tissue of hypothyroid animals. This is in contrast with our previous finding [56] showing that i.c.v. leptin infusion in euthyroid rats decreased resistin mRNA expression in adipose tissue. These contradictory results could be reconciled by proposing that in hypothyroidism the increased resistin mRNA expression is related to decreased plasma T3 levels (Table 3), a situation that could prevail over the inhibitory effect of leptin. The observation of the present study that i.c.v. leptin did not decrease resistin mRNA expression in hypothyroid animals might be part of the reason why leptin did not completely restore insulin responsiveness in hypothyroid animals.
In conclusion, the results of the present study show that mild hypothyroidism induces a state of decreased insulin responsiveness, as assessed during euglycaemic–hyperinsulinaemic clamps and insulin tolerance tests. This effect is in part due to lowered plasma leptin levels, and it is potentially also related to the overexpression of resistin. These two factors combined may be the reasons why hypothyroid animals have low fatty acid oxidation, ultimately producing an increased glucose–fatty acid cycle, inhibitory to glucose disposal.
Abbreviations
- cDNA:
-
Complementary DNA
- CPT-1α:
-
Carnitine palmitoyl transferase 1α
- CPT-1β:
-
Carnitine palmitoyl transferase 1β
- D1:
-
Deiodinase type 1
- D2:
-
Deiodinase type 2
- 2-DG:
-
2-Deoxy-D-[1-3H]glucose
- GIR:
-
Glucose infusion rate
- i.c.v.:
-
Intracerebroventricular
- ITT:
-
Insulin tolerance test
- PTU:
-
Propylthiouracil
- Ra:
-
Rate of glucose appearance
- Rd:
-
Rate of glucose disappearance
References
Tata JR, Ernster L, Lindberg O (1962) Control of basal metabolic rate by thyroid hormones and cellular function. Nature 193:1058–1060
Silva JE (2003) The thermogenic effect of thyroid hormone and its clinical implications. Ann Intern Med 139:205–213
Oppenheimer JH, Schwartz HL, Lane JT et al (1991) Functional relationship of thyroid hormone-induced lipogenesis, lipolysis, and thermogenesis in the rat. J Clin Invest 87:125–132
Weinstein SP, O’Boyle E, Haber RS (1994) Thyroid hormone increases basal and insulin-stimulated glucose transport in skeletal muscle. The role of GLUT4 glucose transporter expression. Diabetes 43:1185–1189
Dimitriadis G, Parry-Billings M, Bevan S et al (1997) The effects of insulin on transport and metabolism of glucose in skeletal muscle from hyperthyroid and hypothyroid rats. Eur J Clin Invest 27:475–483
Weinstein SP, Watts J, Haber RS (1991) Thyroid hormone increases muscle/fat glucose transporter gene expression in rat skeletal muscle. Endocrinology 129:455–464
Dimitriadis GD, Leighton B, Parry-Billings M et al (1989) Effects of hypothyroidism on the sensitivity of glycolysis and glycogen synthesis to insulin in the soleus muscle of the rat. Biochem J 257:369–373
Arner P, Bolinder J, Wennlund A et al (1984) Influence of thyroid hormone level on insulin action in human adipose tissue. Diabetes 33:369–375
Andreani D, Menzinger G, Fallucca F et al (1970) Insulin levels in thyrotoxicosis and primary myxoedema: response to intravenous glucose and glucagon. Diabetologia 6:1–7
Ahren B (1986) Hyperthyroidism and glucose intolerance. Acta Med Scand 220:5–14
Achmadi J, Terashima Y (1995) The effect of propylthiouracil-induced low thyroid function on secretion response and action of insulin in sheep. Domest Anim Endocrinol 12:157–166
van Dijk G (2001) The role of leptin in the regulation of energy balance and adiposity. J Neuroendocrinol 13:913–921
Ceddia RB, Koistinen HA, Zierath JR et al (2002) Analysis of paradoxical observations on the association between leptin and insulin resistance. FASEB J 16:1163–1176
Valcavi R, Zini M, Peino R et al (1997) Influence of thyroid status on serum immunoreactive leptin levels. J Clin Endocrinol Metab 82:1632–1634
Yoshida T, Momotani N, Hayashi M et al (1998) Serum leptin concentrations in patients with thyroid disorders. Clin Endocrinol (Oxf) 48:299–302
Iglesias P, Alvarez Fidalgo P, Codoceo R et al (2003) Serum concentrations of adipocytokines in patients with hyperthyroidism and hypothyroidism before and after control of thyroid function. Clin Endocrinol (Oxf) 59:621–629
Leonhardt U, Ritzel U, Schafer G et al (1998) Serum leptin levels in hypo- and hyperthyroidism. J Endocrinol 157:75–79
Pinkney JH, Goodrick SJ, Katz J et al (1998) Leptin and the pituitary–thyroid axis: a comparative study in lean, obese, hypothyroid and hyperthyroid subjects. Clin Endocrinol (Oxf) 49:583–588
Chen MD, Song YM, Tsou CT et al (2000) Leptin concentration and the Zn/Cu ratio in plasma in women with thyroid disorder. Biol Trace Elem Res 75:99–105
Sesmilo G, Casamitjana R, Halperin I et al (1998) Role of thyroid hormones on serum leptin levels. Eur J Endocrinol 139:428–430
Miyakawa M, Tsushima T, Murakami H et al (1999) Serum leptin levels and bioelectrical impedance assessment of body composition in patients with Graves’ disease and hypothyroidism. Endocr J 46:665–673
Ahima RS, Prabakaran D, Mantzoros C et al (1996) Role of leptin in the neuroendocrine response to fasting. Nature 382:250–252
Legradi G, Emerson CH, Ahima RS et al (1997) Leptin prevents fasting-induced suppression of prothyrotropin-releasing hormone messenger ribonucleic acid in neurons of the hypothalamic paraventricular nucleus. Endocrinology 138:2569–2576
Seoane LM, Carro E, Tovar S et al (2000) Regulation of in vivo TSH secretion by leptin. Regul Pept 92:25–29
Cusin I, Rouru J, Visser T et al (2000) Involvement of thyroid hormones in the effect of intracerebroventricular leptin infusion on uncoupling protein-3 expression in rat muscle. Diabetes 49:1101–1105
Flier JS, Harris M, Hollenberg AN (2000) Leptin, nutrition, and the thyroid: the why, the wherefore, and the wiring. J Clin Invest 105:859–861
Cettour-Rose P, Burger AG, Meier CA et al (2002) Central stimulatory effect of leptin on T3 production is mediated by brown adipose tissue type II deiodinase. Am J Physiol Endocrinol Metab 283:E980–E987
Rouru J, Cusin I, Zakrzewska KE et al (1999) Effects of intravenously infused leptin on insulin sensitivity and on the expression of uncoupling proteins in brown adipose tissue. Endocrinology 140:3688–3692
Cusin I, Zakrzewska KE, Boss O et al (1998) Chronic central leptin infusion enhances insulin-stimulated glucose metabolism and favors the expression of uncoupling proteins. Diabetes 47:1014–1019
Rohner-Jeanrenaud F, Walker CD, Greco-Perotto R et al (1989) Central corticotropin-releasing factor administration prevents the excessive body weight gain of genetically obese (fa/fa) rats. Endocrinology 124:733–739
Visser TJ (1996) Pathways of thyroid hormone metabolism. Acta Med Austriaca 23:10–16
Silva JE, Leonard JL (1985) Regulation of rat cerebrocortical and adenohypophyseal type II 5′-deiodinase by thyroxine, triiodothyronine, and reverse triiodothyronine. Endocrinology 116:1627–1635
Kaiser CA, Goumaz MO, Burger AG (1986) In vivo inhibition of the 5′-deiodinase type II in brain cortex and pituitary by reverse triiodothyronine. Endocrinology 119:762–770
Cusin I, Terrettaz J, Rohner-Jeanrenaud F et al (1990) Metabolic consequences of hyperinsulinaemia imposed on normal rats on glucose handling by white adipose tissue, muscles and liver. Biochem J 267:99–103
Vettor R, Zarjevski N, Cusin I et al (1994) Induction and reversibility of an obesity syndrome by intracerebroventricular neuropeptide Y administration to normal rats. Diabetologia 37:1202–1208
Terrettaz J, Assimacopoulos-Jeannet F, Jeanrenaud B (1986) Severe hepatic and peripheral insulin resistance as evidenced by euglycemic clamps in genetically obese fa/fa rats. Endocrinology 118:674–678
Kraegen EW, Clark PW, Jenkins AB et al (1991) Development of muscle insulin resistance after liver insulin resistance in high-fat-fed rats. Diabetes 40:1397–1403
Herbert V, Lau KS, Gottlieb CW et al (1965) Coated charcoal immunoassay of insulin. J Clin Endocrinol Metab 25:1375–1384
Geffner DL, Azukizawa M, Hershman JM (1975) Propylthiouracil blocks extrathyroidal conversion of thyroxine to triiodothyronine and augments thyrotropin secretion in man. J Clin Invest 55:224–229
Saberi M, Sterling FH, Utiger RD (1975) Reduction in extrathyroidal triiodothyronine production by propylthiouracil in man. J Clin Invest 55:218–223
Karakoc A, Ayvaz G, Taneri F et al (2004) The effects of hypothyroidism in rats on serum leptin concentrations and leptin mRNA levels in adipose tissue and relationship with body fat composition. Endocr Res 30:247–255
Shimomura I, Hammer RE, Richardson JA et al (1998) Insulin resistance and diabetes mellitus in transgenic mice expressing nuclear SREBP-1c in adipose tissue: model for congenital generalized lipodystrophy. Genes Dev 12:3182–3194
Ebihara K, Ogawa Y, Masuzaki H et al (2001) Transgenic overexpression of leptin rescues insulin resistance and diabetes in a mouse model of lipoatrophic diabetes. Diabetes 50:1440–1448
Haque WA, Shimomura I, Matsuzawa Y et al (2002) Serum adiponectin and leptin levels in patients with lipodystrophies. J Clin Endocrinol Metab 87:2395
Steppan CM, Bailey ST, Bhat S et al (2001) The hormone resistin links obesity to diabetes. Nature 409:307–312
Moon B, Kwan JJ, Duddy N et al (2003) Resistin inhibits glucose uptake in L6 cells independently of changes in insulin signaling and GLUT4 translocation. Am J Physiol Endocrinol Metab 285:E106–E115
Rajala MW, Obici S, Scherer PE et al (2003) Adipose-derived resistin and gut-derived resistin-like molecule-beta selectively impair insulin action on glucose production. J Clin Invest 111:225–230
Pravenec M, Kazdova L, Landa V et al (2003) Transgenic and recombinant resistin impair skeletal muscle glucose metabolism in the spontaneously hypertensive rat. J Biol Chem 278:45209–45215
Nogueiras R, Gualillo O, Caminos JE et al (2003) Regulation of resistin by gonadal, thyroid hormone, and nutritional status. Obes Res 11:408–414
Shimomura I, Hammer RE, Ikemoto S et al (1999) Leptin reverses insulin resistance and diabetes mellitus in mice with congenital lipodystrophy. Nature 401:73–76
Oral EA, Simha V, Ruiz E et al (2002) Leptin-replacement therapy for lipodystrophy. N Engl J Med 346:570–578
Petersen KF, Oral EA, Dufour S et al (2002) Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J Clin Invest 109:1345–1350
Farooqi IS, Jebb SA, Langmack G et al (1999) Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N Engl J Med 341:879–884
Hidaka S, Yoshimatsu H, Kondou S et al (2002) Chronic central leptin infusion restores hyperglycemia independent of food intake and insulin level in streptozotocin-induced diabetic rats. FASEB J 16:509–518
Randle PJ, Garland PB, Newsholme EA et al (1965) The glucose fatty acid cycle in obesity and maturity onset diabetes mellitus. Ann N Y Acad Sci 131:324–333
Asensio C, Cettour-Rose P, Theander-Carrillo C et al (2004) Changes in glycemia by leptin administration or high-fat feeding in rodent models of obesity/type 2 diabetes suggest a link between resistin expression and control of glucose homeostasis. Endocrinology 145:2206–2213
Acknowledgements
This work was carried out thanks to grant 3100A0-105889/1 of the Swiss National Science Foundation (Berne, Switzerland), and thanks to grants-in-aid of Eli Lilly and Company (Indianapolis, IN, USA), Hoffmann-La Roche (Basle, Switzerland), Novartis Foundation (Basle, Switzerland) and the Roche Research Foundation (Basle, Switzerland). We are grateful to and acknowledge Eli Lilly and Company for the generous gift of leptin. Finally, we thank Ellen Kaptein (Erasmus University, Rotterdam, The Netherlands) and Jean-Daniel Graf (University of Geneva, Geneva, Switzerland) for their excellent technical assistance. This study was part of the Geneva Program for Metabolic Disorders. F. Rohner-Jeanrenaud was also supported by the European Community (EC) FP6 funding (contract no. LSHM-CT-2003-503041). This publication reflects the authors’ views and not necessarily those of the EC. The information in this document is provided as it is and no guarantee or warranty is given that the information is fit for any particular purpose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cettour-Rose, P., Theander-Carrillo, C., Asensio, C. et al. Hypothyroidism in rats decreases peripheral glucose utilisation, a defect partially corrected by central leptin infusion. Diabetologia 48, 624–633 (2005). https://doi.org/10.1007/s00125-005-1696-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1696-4