Abstract
Introduction
Traumatic out-of-hospital cardiac arrest (tOHCA) has a mortality rate over 95%. Many current protocols dictate rapid intra-arrest transport of these patients. We hypothesized that on-scene advanced life support (ALS) would increase the odds of arriving at the emergency department with ROSC (ROSC at ED) in comparison to performance of no ALS or ALS en route.
Methods
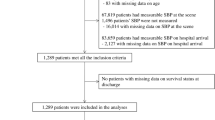
We utilized the 2018–2021 ESO Research Collaborative public use datasets for this study, which contain patient care records from ~2000 EMS agencies across the US. All OHCA patients with an etiology of “trauma” or “exsanguination” were screened (n=15,691). The time of advanced airway management, vascular access, and chest decompression was determined for each patient. Logistic regression modeling was used to evaluate the association of ALS intervention timing with ROSC at ED.
Results
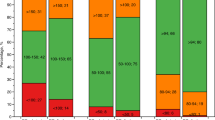
4942 patients met inclusion criteria. 14.6% of patients had ROSC at ED. In comparison to no vascular access, on-scene (aOR: 2.14 [1.31, 3.49]) but not en route vascular access was associated with increased odds of having ROSC at ED arrival. In comparison to no chest decompression, neither en route nor on-scene chest decompression were associated with ROSC at ED arrival. Similarly, in comparison to no advanced airway management, neither en route nor on-scene advanced airway management were associated with ROSC at ED arrival. The odds of ROSC at ED decreased by 3% (aOR: 0.97 [0.94, 0.99]) for every 1-minute increase in time to vascular access and decreased by 5% (aOR: 0.95 [0.94, 0.99]) for every 1-minute increase in time to epinephrine.
Conclusion
On-scene ALS interventions were associated with increased ROSC at ED in our study. These data suggest that initiating ALS prior to rapid transport to definitive care in the setting of tOHCA may increase the number of patients with a palpable pulse at ED arrival.



Similar content being viewed by others
Data availability
The data used for these analyses is not available from the authors. The data may be accessed via ESO upon reasonable request.
References
Evans CC, et al. Prehospital traumatic cardiac arrest: management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J Trauma Acute Care Surg. 2016;81(2):285–93.
Vianen NJ, et al. Prehospital traumatic cardiac arrest: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2022. https://doi.org/10.1007/s00068-022-01975-2.
Grunau B, et al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. JAMA. 2020;324(11):1058–67.
Olasveengen TM, Wik L, Steen PA. Quality of cardiopulmonary resuscitation before and during transport in out-of-hospital cardiac arrest. Resuscitation. 2008;76(2):185–90.
Zive D, et al. Variation in out-of-hospital cardiac arrest resuscitation and transport practices in the Resuscitation Outcomes Consortium: ROC Epistry-Cardiac Arrest. Resuscitation. 2011;82(3):277–84.
StataCorp. Melogit—Multilevel mixed-effects logistic regression. Available from: https://www.stata.com/manuals/memelogit.pdf. Accessed 1 Jan 2023
Barnard EBG, et al. Prehospital determinants of successful resuscitation after traumatic and non-traumatic out-of-hospital cardiac arrest. Emerg Med J. 2019;36(6):333–9.
Tran A, et al. Pre-arrest and intra-arrest prognostic factors associated with survival following traumatic out-of-hospital cardiac arrest—a systematic review and meta-analysis. Resuscitation. 2020;153:119–35.
Benhamed A, et al. Prehospital predictors for return of spontaneous circulation in traumatic cardiac arrest. J Trauma Acute Care Surg. 2022;92(3):553–60.
Seamon MJ, et al. An evidence-based approach to patient selection for emergency department thoracotomy: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;79(1):159–73.
Lin YR, et al. Time to epinephrine treatment is associated with the risk of mortality in children who achieve sustained ROSC after traumatic out-of-hospital cardiac arrest. Crit Care. 2019;23(1):101.
Andersen LW, et al. Time to epinephrine and survival after pediatric in-hospital cardiac arrest. JAMA. 2015;314(8):802–10.
Hansen M, et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation. 2018;137(19):2032–40.
Donnino MW, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. BMJ. 2014;348: g3028.
Krug EG, Powell KE, Dahlberg LL. Firearm-related deaths in the United States and 35 other high- and upper-middle-income countries. Int J Epidemiol. 1998;27(2):214–21.
Funding
National Institute of General Medical Sciences, 5U54GM104942-05, James Bardes.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the listed authors have any financial or other conflicts of interest that may have influenced the results of this study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Smida, T., Price, B.S., Scheidler, J. et al. Stay and play or load and go? The association of on-scene advanced life support interventions with return of spontaneous circulation following traumatic cardiac arrest. Eur J Trauma Emerg Surg 49, 2165–2172 (2023). https://doi.org/10.1007/s00068-023-02279-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02279-9