Abstract
Purpose
Evidence for a hospital volume–outcome relationship in hip fracture surgery is inconclusive. This study aimed to analyze the association between hospital volume as a continuous parameter and several processes and outcomes of hip fracture care.
Methods
Adult patients registered in the nationwide Dutch Hip Fracture Audit (DHFA) between 2018 and 2020 were included. The association between annual hospital volume and turnaround times (time on the emergency ward, surgery < 48 h and length of stay), orthogeriatric co-treatment and case-mix adjusted in-hospital and 30 days mortality was evaluated with generalized linear mixed models with random effects for hospital and treatment year. We used a fifth-degree polynomial to allow for nonlinear effects of hospital volume. P-values were adjusted for multiple comparisons using the Bonferoni method.
Results
In total, 43,258 patients from 68 hospitals were included. The median annual hospital volume was 202 patients [range 1–546]. Baseline characteristics did not differ with hospital volume. Provision of orthogeriatric co-treatment improved with higher volumes but decreased at > 367 patients per year (p < 0.01). Hospital volume was not significantly associated with mortality outcomes. No evident clinical relation between hospital volume and turnaround times was found.
Conclusion
This is the first study analyzing the effect of hospital volume on hip fracture care, treating volume as a continuous parameter. Mortality and turnaround times showed no clinically relevant association with hospital volume. The provision of orthogeriatric co-treatment, however, increased with increasing volumes up to 367 patients per year, but decreased above this threshold. Future research on the effect of volume on complications and functional outcomes is indicated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The expected increase in hip fracture incidence due to the aging population underlines the importance of effective and efficient treatment, leading to the best achievable outcomes. [1,2,3] There is a growing interest in centralization of hip fracture care as treating hip fracture patients in higher-volume hospitals may allow for system-based solutions to minimize operative delay and enable co-management by multidisciplinary teams, thereby improving outcomes while being more cost-effective [4,5,6,7].
The hospital volume–outcome relationship has been examined in several surgical fields, for which a positive effect of higher hospital volume was found on mortality, length of stay, costs and readmissions [8]. Almost 90 percent of the studies published on the hospital volume–outcome relationship in orthopedic surgery found a positive effect of higher hospital volumes on outcomes [8]. However, evidence for the relationship between hospital volume and outcomes of hip fracture surgery is inconclusive [9,10,11].
The varying results in the literature concerning hip fracture surgery outcomes and hospital volume are likely caused by the wide range of cutoff values used to define hospital volume, which is a common problem in volume–outcome analyses [12]. To overcome this problem, the volume–outcome relationship might be studied with hospital volume on a continuous scale [10]. Another drawback of the literature on this topic is that most studies focus primarily on mortality as outcome of care. Other outcomes may also be associated with hospital volume and may therefore be of consequence for setting thresholds or defining the quality of care provided by hospitals [8, 12]. Hence, there is a need for analyses with hospital volume as a continuous parameter that focus on more outcomes of care than mortality only.
This study aimed to analyze the effect of hospital volume as a continuous parameter on several processes in and outcomes of hip fracture care, using data obtained from the nationwide Dutch Hip Fracture Audit in the Netherlands.
Material and methods
Data for this cohort study were retrieved from the Dutch Hip Fracture Audit (DHFA), a nationwide registry of hip fracture patients in the Netherlands [13]. All registered adult hip fracture patients treated in 68 hospitals between 1-1-2018 and 31-12-2020 were included. Patients with non-operative treatment and patients who suffered a peri-prosthetic or pathological fracture were excluded. DHFA data were supplemented with dates of death from the Dutch Vektis institute, which collects data from health insurance reimbursements [14]. DHFA and Vektis data were joined by a trusted third party using social security numbers.
The outcomes and processes used in the analysis were measured on patient level. Therefore, hospital volume was defined as the number of hip fracture patients treated in a specific hospital and calendar year, and was assigned to every patient treated in that hospital in that particular year.
Two types of outcome measures were studied: (1) hospital process variables measured, including turnaround times [length of stay in the emergency department (ED) in minutes, time to surgery within 48 h and duration of hospital stay in days (HLOS)] and orthogeriatric co-treatment, and (2) outcomes including in-hospital and 30 days mortality.
Evidently incorrect values for process times were excluded from the analyses to avoid bias. These values included entries exceeding 24 h of stay in the ED, 7 days to surgery and 90 days of hospital stay. Orthogeriatric co-treatment was analyzed for patients aged 70 years or older. Orthogeriatric co-treatment was considered present if a geriatrician or internal medicine physician specialized in the elderly either was consulted peri-operatively or was head practitioner or if the patient was treated on a specialized geriatric trauma ward. In the case of a onetime postoperative consultation, orthogeriatric co-treatment was considered absent, as this is not according to the standards of the Dutch Health Care Inspectorate (IGJ).
Case-mix variables included age, sex, fracture side, fracture type, pre-fracture mobility, degree of independence, comorbidity, pre-fracture diagnosis of osteoporosis and risk of malnutrition. Fracture types were defined as undislocated and dislocated femoral neck fractures, trochanteric fractures type AO-A1, AO-A2 and AO-A3, and subtrochanteric fractures [15]. Pre-fracture mobility was based on the Fracture Mobility Score [18]. Pre-fracture degree of independence was based on the KATZ Index of Activities of Daily Living (KATZ-6 ADL) score [16] and categorized as independent (KATZ-6-ADL = 0) or dependent (KATZ-6 ADL ≥ 1). Comorbidity was based on the preoperative American Society of Anesthesiologist physical status classification (ASA score) [17] and categorized as no or mild systemic disease (ASA 1–2) and severe or life-threatening systemic disease (ASA 3–5). The risk of malnutrition was measured during hospital stay using the Short Nutritional Assessment Questionnaire (SNAQ) or the Malnutrition Universal Screening Tool (MUST) and categorized as low (SNAQ = 0 or MUST = 0), medium (SNAQ 1–2 or MUST 1) or high risk (SNAQ ≥ 3, MUST ≥ 2) [18, 19].
Statistical analysis
Baseline characteristics are reported using descriptive statistics. For reporting patient and treatment characteristics, hospital volume was divided into quartiles representing low, low–mid, mid–high and high annual hospital volume. To determine whether there was an association between hospital volume and outcome measures, mixed-effects regression models were constructed with hospital volume as a predictor. To account for the association between patients treated within the same hospital, we added hospital as a random intercept. To allow for a flexible relation between volume and the dependent variable, we used a polynomial with a degree between 1 and 5, which was determined using Akaike's information criterion [20].
In analyzing mortality as outcome measure, all case-mix factors described above were added as fixed effects. Missing values for case-mix factors were imputed with the median value for age and the mode for the categorical variables.
The effect of hospital volume on outcomes was tested by comparing the fit of models with and without hospital volume. To account for multiple testing, we adjusted the significance level according to Bonferroni; we multiplied all p values by the number of tests (i.e., 8) [21]. Adjusted p values < 0.05 were regarded statistically significant.
Statistical analysis was performed using R Version 4.0.2 using the ‘lme4’ package for the mixed-effects analysis [22, 23].
Results
Sixty-two hospitals registered data of hip fracture patients in the DHFA in 2018, 63 in 2019 and 68 in 2020. Data of 43,258 operatively treated patients were available for analysis. The median annual registered hospital volume was 202 patients and ranged between 1 and 546. Annual hospital volumes were similar in the three calendar years (Fig. 1). Patient characteristics showed no clinically relevant differences between volume quartile categories (Table 1). Data quality of turnaround times, orthogeriatric co-treatment and mortality was the lowest in low-volume hospitals (Table 1). The registration of these parameters was considered adequate: For none of these parameters, missingness exceeded 10% between 2018 and 2022.
There was wide variation in the mean time in the ED between hospitals (range 86–280 min), regardless of the annual patient volume. In the mixed-effects polynomial regression model, the modeled time in the ED fluctuated between 161 and 181 min, with the widest variation between lower-volume hospitals. This association was statistically significant (p < 0.01) (Fig. 2).
The probability of surgery within 48 h was higher than 0.79 for all hospitals. The modeled probability of surgery within 48 h was stable at 0.94 up to an annual volume of 224 patients, while higher-volume hospitals showed a decrease to 0.91. There was a statistically significant association between the probability of surgery within 48 h and hospital volume (p = 0.04; Fig. 3).
The mean HLOS varied widely between the hospitals, especially for the lower-volume hospitals. However, no association between HLOS and hospital volume was found (p = 1; Fig. 4).
For hospitals with annual volumes of up to 200 patients, the probability of orthogeriatric co-treatment varied between 0 and 100%. In the mixed-effects model, the probability of orthogeriatric co-treatment was low in lower-volume hospitals and was especially low in-hospital volumes between 0 and 100 patients. This probability increased when annual hospital volume increased to 367 patients per year (estimated probability of 0.93). A further increase in annual hospital volume was associated with a decreasing probability of orthogeriatric co-treatment (p < 0.01; Fig. 5).
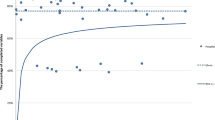
The case-mix adjusted models for both in-hospital and 30 days mortality showed no statistically significant association with hospital volume (p = 0.20 and p = 1, respectively; Figs. 6 and 7).
Multi-level first-degree polynomial regression model of probability of case-mix adjusted in-hospital mortality* and annual hospital volume. * Reference categories used were female gender, left-sided fracture, trochanteric AO-A2 fracture type, mobile outdoors with two aids or frame, independent in daily living activities, ASA score 3, 4 or 5, and no risk of malnutrition
Multi-level polynomial regression model of probability of case-mix adjusted 30 days mortality* and annual hospital volume. *Reference categories used were female gender, left-sided fracture, trochanteric AO-A2 fracture type, mobile outdoors with two aids or frame, independent in daily living activities, ASA score 3, 4 or 5, and no risk of malnutrition
Discussion
This study aimed to analyze the hospital volume effect on quality of hip fracture care in several domains: turnaround times, orthogeriatric co-treatment, and case-mix adjusted in-hospital and 30 days mortality. We found a significant and relevant relation between annual hospital volume and orthogeriatric co-treatment. Although statistically significant, models showed no clinically meaningful association between hospital volume and time in the ED and time to surgery within 48 h. No statistically significant effect of hospital volume was found for HLOS, and in-hospital and 30 days mortality. There seemingly is a wider variance in scores on processes and outcomes in lower-volume centers; however, this is likely explained by their smaller sample sizes.
Several generally accepted explanations exist for a positive effect of high volume on processes and outcomes. First, the ‘practice makes perfect’ principle; operating on higher patient numbers is assumed to make surgeons better at it, likely decreasing the risk of surgery-related complications. High patient volumes may not only affect the performance of individual surgeons; treating more patients may also affect processes and outcomes on institutional levels. Higher institutional volumes may allow for increased workflow, more homogeneity in treatment, better resource utilization and specialization of personnel [24]. A positive volume–outcome effect may also result from ‘selective referral’: a vicious circle in which high-performing hospitals increasingly receive more patients and gain more experience [12]. Examples of organizational benefits of high volume in hip fracture care are specific timeslots for hip fracture surgery, dedicated hip fracture treatment teams, specialized wards and implementation of evidence-based hip fracture care pathways [25]. Alternatively, higher volumes might lead to suboptimal quality of care and can negatively affect processes and outcomes, if high patient volumes lead to greater workloads than the organizational structure can handle.
The most striking result of our study is the relationship between hospital volume and orthogeriatric co-treatment. The probability of receiving orthogeriatric co-treatment increased with higher volumes, up to 367 patients per year. This is in line with the study by Shabani et al., who also found that higher-volume hospitals scored better on several preoperative medical assessments [9]. It is plausible that these hospitals are more likely dedicated hip fracture centers, with an orthogeriatric ward or a dedicated hip fracture team allowing co-treatment by a geriatrician. In our study, the probability of receiving orthogeriatric co-treatment decreased in hospitals treating over 367 patients per year. Possibly, under-capacity of staffing limits the relationship between hospital volume and this quality of care indicator.On the other hand, a more differentiated approach toward orthogeriatric co-treatment in higher-volume hospitals, based on extensive experience, may lead to a more selective deployment of medical specialist. More research is needed to elucidate these findings.
One could hypothesize that turnaround times are positively affected by the aforementioned organizational benefits of higher hospital volumes. However, the findings in our study do not clearly substantiate this hypothesis. Although we found statistically significant associations between patient volume and both time spent in the ED and surgery within 48 h, the clinical relevance of this finding is questionable. For time in the ED, the polynomial spline fluctuated, especially for lower volumes with a wider confidence interval, but did not show a trend toward increasing or decreasing turnaround times with the increase of volume. For surgery within 48 h, the modeled probability changed only by 3% (between 91 and 94%).The effect of hospital volume on turnaround times in the ED was only studied earlier by Shabani et al., who did not find an effect of volume on time to admission to an orthopedic ward, nor on the HLOS [9]. The latter finding corresponds with our study in which HLOS was not associated with hospital volume. The absence of this relation in our study contradicts most previous studies included in two reviews that both found that patients treated in low-volume centers had longer HLOS. However, these reviews and meta-analyses were limited by the various volume thresholds [10, 26]. Another striking finding is the relatively high percentage of patients operated on within 48 h. The time to surgery was used as an obligatory quality indicator for the Dutch Health Care Inspectorate in the past few years, which may have led to a shortening of the time to surgery, regardless of the hospital volume. We believe this to be a promising finding that underlines the expediency of hip fracture audits.
We did not find a relationship between hospital volume and case-mix corrected in-hospital and 30 days mortality. Wiegers et al. published a review analyzing over 2 million patients in 2019, including a meta-analysis. Ten out of twenty studies reported no hospital volume effect on in-hospital mortality, eight studies reported lower mortality in high-volume centers (threshold of > 170 patients/year), and two reported lower mortality in low-volume centers. The meta-analysis did not show an overall statistically significant association between hospital volume and in-hospital mortality. However, we believe that this nonsignificant overall result, again, is due to the wide variance in thresholds used [10]. Contradictorily, a scoping review of studies covering twelve different surgical specialties by Levaillant et al. reported that 86.2% of the studies included showed a significantly positive effect of higher hospital volume on mortality. The absence of a volume–outcome relation for mortality in hip fractures and the apparent presence of this volume–outcome relation in other surgical specialties might be explained by differences in the complexity of the surgical interventions [8].
This is the first study in which a large cohort of hip fractures is used to analyze the volume effect on multiple processes and outcomes on a patient level, using volume as a continuous parameter. Another strength of this study is the use of an extensive case-mix model in the analysis of mortality outcomes. The main limitation of this study concerns the use of registry data, of which the researchers could not validate the quality. Due to limitations in the number of complete years of registration, we could not perform internal validation of the models.
Our study has implications for the debate on centralization of hip fracture care. Our results do not justify the centralization of hip fracture services for the sole purpose of improving the quality of care provided. Needless to say, this conclusion holds true only for the process and mortality outcome parameters tested in this study. Future studies could analyze surgical complications and functional outcomes and evaluate the effect of provider volume. Also, future studies could include a continuous volume–value analysis, as the effect of higher volume or centralization may not merely impact the quality of care but also affect hip fracture care costs [11]. We believe orthogeriatric co-treatment to be impacted by hospital volume in the Netherlands and should therefore be further investigated. Instead of centralizing care and thereby withholding patients geographically accessible care, it would be better to share best practices and enhance collaborations between hospitals to improve the quality of hip fracture care on a national level.
Conclusion
This study showed that hospital volume does not have a clinically relevant effect on turnaround times, nor does it affect in-hospital and 30 days mortality. However, orthogeriatric co-treatment within the nationwide hip fracture registry in the Netherlands seems to be provided more often in higher-volume hospital with a maximum of 367 patients and should be further analyzed. Although our findings may be relevant in the centralization debate, additional analysis of complications and functional outcomes treating volume as a continuous parameter is indicated to draw final conclusions on the effect of hospital volume on the quality of hip fracture care.
Data Availability
The data that support the findings of this study are available on request through the Dutch Institute of Clinical Auditing. Restrictions apply to the availability of these data, which were used under license for this study.
References
Konnopka A, Jerusel N, König H-H. The health and economic consequences of osteopenia- and osteoporosis-attributable hip fractures in Germany: estimation for 2002 and projection until 2050. Osteoporos Int. 2008;207(20):1117–29.
Williamson S, Landeiro F, McConnell T, et al. Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int. 2017;28:2791–800.
Veronese N, Kolk H, Maggi S. Epidemiology of Fragility Fractures and Social Impact. 2020 Aug 21. In: Falaschi P, Marsh D, editors. Orthogeriatrics: The Management of Older Patients with Fragility Fractures [Internet]. 2nd ed. Cham (CH): Springer; 2021. Chapter 2.
Dy CJ, McCollister KE, Lubarsky DA, Lane JM. An economic evaluation of a systems-based strategy to expedite surgical treatment of hip fractures. J Bone Jt Surg Am. 2011;93:1326–34.
Swart E, Vasudeva E, Makhni EC, et al. Dedicated perioperative hip fracture comanagement programs are cost-effective in high-volume centers: an economic analysis. Clin Orthop Relat Res. 2016;474:222–33.
Coyle S, Kinsella S, Lenehan B, Queally JM. Cost-utility analysis in orthopaedic trauma; what pays? A systematic review. Injury. 2018;49:575–84.
Gandjour A, Weyler EJ. Cost-effectiveness of referrals to high-volume hospitals: an analysis based on a probabilistic Markov model for hip fracture surgeries. Health Care Manag Sci. 2006;9:359–69.
Levaillant M, Marcilly R, Levaillant L, et al. Assessing the hospital volume-outcome relationship in surgery: a scoping review. BMC Med Res Methodol. 2021;21:204.
Shabani F, Tsinaslanidis G, Thimmaiah R et al. Effect of institution volume on mortality and outcomes in osteoporotic hip fracture care. Osteoporos Int. 2022 Nov;33(11):2287–92.
Wiegers EJAA, Sewalt CA, Venema E, et al. The volume-outcome relationship for hip fractures: a systematic review and meta-analysis of 2,023,469 patients. Acta Orthop. 2019;90:26–32.
Navarro SM, Frankel WC, Haeberle HS, et al. Evaluation of the volume-value relationship in hip fracture care using evidence-based thresholds. Hip Int. 2020;30(3):347–53.
Christian CK, Gustafson ML, Betensky RA, et al. The volume-outcome relationship: don’t believe everything you see. World J Surg. 2005;29:1241–4.
Voeten SC, Arends AJ, Wouters MWJM, et al. The Dutch Hip Fracture Audit: evaluation of the quality of multidisciplinary hip fracture care in the Netherlands. Arch Osteoporos. 2019;14:28.
Vektis - business intelligence centrum voor de zorg|Vektis.nl. https://www.vektis.nl/. Accessed 26 Feb 2021.
Colton C, Krikler S, Schatzker J, Trafton P AO Surgery Reference—a Comprehensive online reference in daily clinical life. https://www2.aofoundation.org/wps/portal/surgery. . Accessed 11 May 2017.
Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA J Am Med Assoc. 1963;185:914–9.
ASA Physical Status Classification System|American Society of Anesthesiologists (ASA). https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. Accessed 25 Jan 2021.
Kruizenga HM, Seidell JC, de Vet HCW, et al. Development and validation of a hospital screening tool for malnutrition: the short nutritional assessment questionnaire (SNAQ©). Clin Nutr. 2005;24:75–82.
Elia M. The malnutrition advisory group consensus guidelines for the detection and management of malnutrition in the community. Nutr Bull. 2001;26:81–3.
Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974. https://doi.org/10.1109/TAC.1974.1100705.
Bonferonni C (1936) Teoria statistica delle classi e calcolo delle probabilita. In: Pubblicazioni del R Istituto Superiore di Scienze Economiche e Commericiali di Firenze. pp 3–62.
RStudio Team (2020). RStudio: Integrated Development for R. RStudio, PBC, Boston, MA
Bates D, Mächler M, Bolker B, Walker S (2015). Fitting Linear Mixed-Effects Models Using lme4. J Stat Softw. 67(1):1–48.
Kraus TW, Büchler MW, Herfarth C. Relationships between volume, efficiency, and quality in surgery—a delicate balance from managerial perspectives. World J Surg. 2005;29:1234–40.
Mesman R, Westert GP, Berden BJMM, Faber MJ. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume–outcome relationships. Health Policy (New York). 2015;119:1055–67.
Malik AT, Panni UY, Masri BA, Noordin S. The impact of surgeon volume and hospital volume on postoperative mortality and morbidity after hip fractures: a systematic review. Int J Surg. 2018;54:316–27.
Funding
No funds, grants or other support was received.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Analysis were performed by FW, PK and EvZ. The first draft of the manuscript was written by FW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
Permission for the use of pseudonymized patient data for research purposes is assured within the Dutch Hip Fracture Audit. Due to the nature of this study no patient informed consent or approval of the medical ethical commission was required.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Würdemann, F.S., van Zwet, E.W., Krijnen, P. et al. Is hospital volume related to quality of hip fracture care? Analysis of 43,538 patients and 68 hospitals from the Dutch Hip Fracture Audit. Eur J Trauma Emerg Surg 49, 1525–1534 (2023). https://doi.org/10.1007/s00068-022-02205-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02205-5