Abstract
Purpose
Numerous studies have modified the Trauma Injury and Severity Score (TRISS) to improve its predictive accuracy for specific trauma populations. The aim of this study was to develop and validate a simple and practical prediction model that accurately predicts mortality for all acute trauma admissions.
Methods
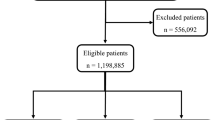
This retrospective study used Dutch National Trauma Registry data recorded between 2015 and 2018. New models were developed based on nonlinear transformations of TRISS variables (age, systolic blood pressure (SBP), Glasgow Coma Score (GCS) and Injury Severity Score (ISS)), the New Injury Severity Score (NISS), the sex–age interaction, the best motor response (BMR) and the American Society of Anesthesiologists (ASA) physical status classification. The models were validated in 2018 data and for specific patient subgroups. The models’ performance was assessed based on discrimination (areas under the curve (AUCs)) and by calibration plots. Multiple imputation was applied to account for missing values.
Results
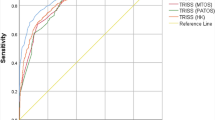
The mortality rates in the development and validation datasets were 2.3% (5709/245363) and 2.5% (1959/77343), respectively. A model with sex, ASA class, and nonlinear transformations of age, SBP, the ISS and the BMR showed significantly better discrimination than the TRISS (AUC 0.915 vs. 0.861). This model was well calibrated and demonstrated good discrimination in different subsets of patients, including isolated hip fractures patients (AUC: 0.796), elderly (AUC: 0.835), less severely injured (ISS16) (AUC: 878), severely injured (ISS ≥ 16) (AUC: 0.889), traumatic brain injury (AUC: 0.910). Moreover, discrimination for patients admitted to the intensive care (AUC: s0.846), and for both non-major and major trauma center patients was excellent, with AUCs of 0.940 and 0.895, respectively.
Conclusion
This study presents a simple and practical mortality prediction model that performed well for important subgroups of patients as well as for the heterogeneous population of all acute trauma admissions in the Netherlands. Because this model includes widely available predictors, it can also be used for international evaluations of trauma care within institutions and trauma systems.




Similar content being viewed by others
References
Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma score and the injury severity score. J Trauma. 1987;27(4):370–8.
Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW, et al. The major trauma outcome study: Establishing national norms for trauma care. J Trauma Inj Infect Crit Care. 1990;30(11):1356–65.
Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma Inj Infect Crit Care. 1989;29(5):623–9.
Healey C, Osler TM, Rogers FB, Healey MA, Glance LG, Kilgo PD, et al. Improving the glasgow coma scale score: motor score alone is a better predictor. J Trauma United States. 2003;54:671–80.
Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma United States. 1997;43:922–6.
Brenneman FD, Boulanger BR, McLellan BA, Redelmeier DA. Measuring injury severity: time for a change? J Trauma United States. 1998;44:580–2.
de Munter L, Ter Bogt NCW, Polinder S, Sewalt CA, Steyerberg EW, de Jongh MAC. Improvement of the performance of survival prediction in the ageing blunt trauma population: A cohort study. PLoS ONE. 2018;13: e0209099.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGU™: the Revised Injury Severity Classification, version II. Crit Care. 2014;18:476.
Bouamra O, Jacques R, Edwards A, Yates DW, Lawrence T, Jenks T, et al. Prediction modelling for trauma using comorbidity and “true” 30-day outcome. Emerg Med J England. 2015;32:933–8.
Lefering R, Huber-Wagner S, Bouillon B, Lawrence T, Lecky F, Bouamra O. Cross-validation of two prognostic trauma scores in severely injured patients. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc Germany. 2020;47(6):1837–45.
Newgard CD, Caughey A, McConnell KJ, Lin A, Eckstrom E, Griffiths D, et al. Comparison of injured older adults included in vs excluded from trauma registries with 1-year follow-up. JAMA Surg. 2019;154: e192279.
van der Vliet QMJ, Hietbrink F, Leenen LPH. Inclusion of all patients admitted for trauma in trauma Registries. JAMA Surg United States. 2020;155(3):264–5.
Newgard CD, Bulger EM. Inclusion of all patients admitted for trauma in trauma registries-Reply. JAMA Surg United States. 2020;155(3):265–6.
Driessen MLS, Sturms LM, Bloemers FW, ten Duis HJ, Edwards MJR, den Hartog D, et al. The Dutch nationwide trauma registry: The value of capturing all acute trauma admissions. Injury. 2020;51(11):2553–9.
Rotondo M, Cribari C SS. Resources for optimal care of the injured patient-2014. Bull Am Coll Surg. 2014.
Ringdal KG, Coats TJ, Lefering R, Di Bartolomeo S, Steen PA, Røise O, et al. The Utstein template for uniform reporting of data following major trauma: A joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16(1):1–19.
Dripps RD. New Classification of Physical Status. Anesthesiology. 1963;24:111.
Gennarelli TA, Wodzin E. AIS 2005: A contemporary injury scale. Injury. 2006;37(12):1083–91.
Moons KGM, Altman DG, Reitsma JB, Ioannidis JPA, Macaskill P, Steyerberg EW, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med United States. 2015;162:W1-73.
R Core Team (2020). R: A language and enviroment for statistic computing. R Foundation for Statistical Computing, Vienne Austria; 2020.
van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Software 2011;1(3).
Landelijk Netwerk Acute Zorg (LNAZ) Jaarrapport Landelijke Trauma Registratie (LTR) 2015–2019. 2020.
Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling. Appl Stat. 1994;43(3):429–53.
Harrell FE J. RMS: Regression Modeling Strategies. 2019.
Nagelkerke NJD. A note on a general definition of the coefficient of determination. Biometrika. 1991.
Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol Off Publ Int Assoc Study Lung Cancer United States. 2010;5:1315–6.
Hosmer D Jr, Lemeshow SSR. Applied Logistic Regression. New York: John Wiley and Sons; 2000. p. 160–4.
de Munter L, Polinder S, Nieboer D, Lansink KWW, Steyerberg EW, de Jongh MAC. Performance of the modified TRISS for evaluating trauma care in subpopulations: A cohort study. Injury Netherlands. 2018;49:1648–53.
Vassar MJ, Lewis FRJ, Chambers JA, Mullins RJ, O’Brien PE, Weigelt JA, et al. Prediction of outcome in intensive care unit trauma patients: a multicenter study of Acute Physiology and Chronic Health Evaluation (APACHE), Trauma and Injury Severity Score (TRISS), and a 24-hour intensive care unit (ICU) point system. J Trauma United States. 1999;47:324–9.
Skaga NO, Eken T, Søvik S. Validating performance of TRISS, TARN and NORMIT survival prediction models in a Norwegian trauma population. Acta Anaesthesiol Scand. 2018;62:253–66.
Network TTA& R. Procedures manual 2016. Manchester, UK.; 2016.
Hannan EL, Mendeloff J, Farrell LS, Cayten CG, Murphy JG. Multivariate models for predicting survival of patients with trauma from low falls: the impact of gender and pre-existing conditions. J Trauma United States. 1995;38:697–704.
Davis JW, Parks SN, Kaups KL, Gladen HE, O’Donnell-Nicol S. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma United States. 1996;41:769–74.
MacKenzie EJ, Shapiro S, Eastham JN. The Abbreviated Injury Scale and Injury Severity Score. Levels of inter- and intrarater reliability. Med Care United States. 1985;23:823–35.
Zoltie N, de Dombal FT. The hit and miss of ISS and TRISS. Yorkshire Trauma Audit Group. BMJ. 1993;307:906–9.
Twiss E, Krijnen P, Schipper I. Accuracy and reliability of injury coding in the national Dutch Trauma Registry. Int J Qual Heal care. 2021;30(1). https://doi.org/10.1093/intqhc/mzab041.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis England. 1987;40:373–83.
Bergeron E, Rossignol M, Osler T, Clas D, Lavoie A. Improving the TRISS methodology by restructuring age categories and adding comorbidities. J Trauma United States. 2004;56:760–7.
Gabbe BJ, Magtengaard K, Hannaford AP, Cameron PA. Is the Charlson Comorbidity Index useful for predicting trauma outcomes? J Soc Acad Emerg Med United States. 2005;12:318–21.
Kennedy RL, Grant PT, Blackwell D. Low-impact falls: demands on a system of trauma management, prediction of outcome, and influence of comorbidities. J Trauma United States. 2001;51:717–24.
Acknowledgements
The lead author (Mitchell Driessen) affirms that the manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
Author information
Authors and Affiliations
Contributions
DK, MD, MJ, LL and LS conceived and designed the study. DK analyzed the data. Interpretation of the data and writing the first draft of the paper: Driessen, Sturms, van Klaveren. All authors contributed to writing the paper and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare to have no conflict of interest, including financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Driessen, M.L.S., van Klaveren, D., de Jongh, M.A.C. et al. Modification of the TRISS: simple and practical mortality prediction after trauma in an all-inclusive registry. Eur J Trauma Emerg Surg 48, 3949–3959 (2022). https://doi.org/10.1007/s00068-022-01913-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01913-2