Abstract
Purpose
Early enteral feeding within 24–48 h of intensive care unit admission is recommended for critically ill patients. This study aimed to determine if early enteral feeding could be safely implemented with purported benefits in patients with abdominal trauma.
Methods
A retrospective cohort study was performed that included 88 adult patients with abdominal trauma. Patients receiving enteral feeding within 72 h of surgical intensive care unit (SICU) admission (early-initiation group, n = 28) were compared to those receiving enteral feeding later (delayed-initiation group, n = 60).
Results
The two groups were comparable in demographic characteristics and injury severity. There were no differences in feeding intolerance (53.6 vs. 43.3 %, p = 0.37) and mortality at 28 days (0 vs. 5 %, p = 0.55) between the early-initiation group and the delayed-initiation group. However, patients in the early-initiation group had fewer infectious complications (17.9 vs. 40 %, p = 0.04) and shorter length of stay in SICU and hospital (p < 0.01) than patients in the delayed-initiation group.
Conclusions
Early enteral feeding administered within 72 h of SICU admission was associated with improved clinical outcomes without risk of increasing feeding intolerance in patients with abdominal trauma. Our results support the implementation of early enteral feeding in abdominal trauma management.
Similar content being viewed by others
Introduction
Trauma patients are characterized by hypermetabolism and hypercatabolism [1], and therefore are at risk of malnutrition. Malnutrition has been shown to be associated with increased infectious complications, compromised wound healing, prolonged length of hospitalization, and increased mortality [2]. As such, nutritional support is essential in trauma care. Adequate nutritional support may correct catabolism, enhance immune function, and improve clinical outcomes [3].
Enteral nutrition (EN) is the preferred method of nutritional support in trauma patients, since it is associated with lower infectious complications and mortality compared to parenteral nutrition (PN) [4]. However, optimal timing of initiating EN remains unclear. In recent years, there is emerging evidence suggesting that early EN, initiated within 24–48 h of injury or intensive care unit (ICU) admission, is associated with improved outcomes in critically ill patients, including those suffering multiple trauma [5–7]. Furthermore, a recent meta-analysis showed that early EN administered within 24 h of injury is associated with lower mortality compared to standard EN in trauma patients [8]. These findings support the implementation of early EN in trauma care.
Despite the body of evidence in favor of early EN in critically ill and trauma patients [9–12], considerable variability exists in administration of early EN in clinical practice [13, 14]. Average time to initiate EN may range from 8.2 to 149.1 h in critically ill patients [14]. One of the major factors contributing to this variability is the patient population in whom early EN is administered. Patients with abdominal trauma represent one population in whom surgeons and ICU specialists may be reluctant to introduce early EN. This is because of the fear of feeding intolerance and feeding-associated complications such as abdominal distention, vomiting, diarrhea, and ileus. Moreover, evidence supporting early EN in patients with abdominal trauma is scarce and limited by small sample size [15].
Given that it remains uncertain whether early EN could be safely administered with purported benefits in patients with abdominal trauma, we performed a retrospective cohort study to evaluate our nutrition practice in abdominal trauma management. We aimed to determine if early enteral feeding, provided within 72 h of surgical intensive care unit (SICU) admission, was tolerated and beneficial in patients with abdominal trauma.
Methods
This retrospective cohort study utilized the prospectively collected data of patients with abdominal trauma at Department of General Surgery, Jinling Hospital. The study protocol was approved by the ethics committee of Jinling Hospital. The ethics committee also approved waiver of informed consent from patients due to the retrospective nature of the study. Jinling Hospital is a tertiary teaching hospital in Nanjing, China. The Department of General Surgery provides state-of-the-art care for patients admitted to the hospital with abdominal trauma. Patients with abdominal trauma at emergency room (ER) are transferred to one of the two SICUs of Department of General Surgery after emergency operation, or directly transferred to SICU from ER. The two SICUs have a total of 35 beds including high dependency beds. The abdominal trauma management was led by two attending surgeons and two attending SICU specialists.
Patient population
The abdominal trauma database was searched to identify eligible patients between January 2007 and December 2012. For the purpose of this study, adult patients admitted to SICU within 72 h of injury were included. Exclusion criteria were absence of enteral feeding in SICU, early death (within 48 h of admission) due to injury, and early transfer (within 5 days of admission) to other hospitals. All included patients were subsequently divided into the early-initiation group (enteral feeding initiated within 72 h of SICU admission) and the delayed-initiation group (enteral feeding initiated after 72 h).
Nutrition management
For a patient with abdominal trauma, nutritional status was assessed every day, followed by discussion of nutritional support protocol between the treating surgeon and SICU specialists. The timing of initiation of enteral feeding was at the discretion of the treating surgeon and SICU specialist. In general, enteral feeding was commenced as soon as the patient was stable hemodynamically and expected to tolerate according to the judgement by the treating team. Enteral feeding included administration of commercial EN products via mouth, nasogastric tube (NGT), nasojejunal tube (NJT), or jejunostomy feeding tube (JFT). Amino acid formula (Vivonex, Nestlé, Minneapolis, USA) or peptide-based formula (Peptisorb, Nutricia, Wuxi, China) was used as starter EN, followed by a transition towards whole protein formula (Nutrison or Nutrison Fiber, Nutricia, Wuxi, China). In selected cases, supplemental glutamine or fish oil might be administered along with EN fluid. Calory and protein goal of enteral feeding were 25 and 1.5–2.0 g/kg/day, respectively. The initial feeding rate was 15 ml/h. The rate advanced gradually by 15–20 ml every 12 h according to the patient’s tolerance, until reaching the calory goal of enteral feeding. If feeding intolerance occurred, feeding rate was reduced by 1/4–1/2. If severe feeding intolerance persisted, enteral feeding was disrupted and attempted again 12 h later. Supplemental PN (all-in-one PN, Jinling Hospital, Nanjing, China) might be given if EN was insufficient. As administration of EN increased, administration of PN decreased accordingly, and was weaned when reaching 1/3–1/2 of full strength of EN. Prokinetic agents and somatostatin were used in selected cases. Short-term insulin was administered for glucose control.
Data collection
Demographic characteristics including age, gender, and body mass index (BMI) were collected. Injury mechanism, injured organs, injury severity score (ISS), abdominal abbreviated injury scale (AIS), and first day acute physiology and chronic health evaluation (APACHE) II score were also collected.
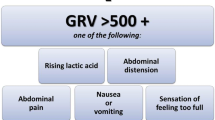
Daily nutritional support protocol until 14 days after SICU admission or SICU discharge was noted, with particular attention to the time of initiation of enteral feeding, route of enteral feeding, presence of supplemental PN, and daily energy delivered from enteral feeding and PN. Occurrence of feeding intolerance, defined as abdominal distension, vomiting, diarrhea, or high gastric residual volume (>200 ml) was noted, as well as disruption of enteral feeding due to persistent feeding intolerance.
Clinical outcomes of interest included need for emergency laparotomy, mortality at 28 days after SICU admission, length of stay in SICU and hospital, and incidence of infectious complications. Infectious complications of interest were pneumonia, intra-abdominal abscess, wound infection, and bacteremia. Diagnosis of infectious complication was made by the treating surgeon or SICU specialist based on clinical manifestations, radiological findings, and results of laboratory tests. Accuracy of collected data was checked by an independent researcher who was not involved in data collection before analysis.
Statistical analysis
Statistical analysis was performed using SPSS software (v19.0 for Windows, SPSS, Inc, an IBM Company, Chicago, USA). Normally distributed continuous variables were analyzed using Student’s t test. Continuous variables with unknown or skewed distribution were analyzed using Mann–Whitney U test. Categorical variables were analyzed using Chi-square test or Fisher’s exact test when expected frequency was less than 5. Feeding intolerance and infectious complications were analyzed as dichotomous variables, regardless of the number of events of feeding intolerance and infection in an individual patient. Significance was set as p < 0.05.
Results
Patient characteristics
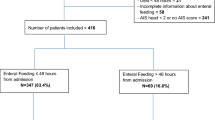
There were 209 patients with abdominal trauma between January 2007 and December 2012, of whom 163 met the inclusion criteria. Seventy-five patients were excluded due to absence of enteral feeding in SICU (n = 66), trauma-induced early death (n = 4), and early transfer to other hospitals (n = 4). Finally, a total of 88 patients were included for analysis (Fig. 1).
Of the 88 patients, 28 (31.8 %) received early enteral feeding within 72 h of SICU admission. These patients were allocated to the early-initiation group, whereas the remaining 60 patients who received enteral feeding after 72 h of admission were allocated to the delayed-initiation group. The two groups were similar in age, gender, BMI, ISS, abdominal AIS, and APACHE II (Table 1). There were, however, more frequent patients with penetrating injury (p = 0.03) and less frequent patients with stomach injury (p = 0.01) in the early-initiation group than the delayed-initiation group.
Nutrition management
Nutrition management was summarized in Table 2. The mean time of initiation of enteral feeding was 2.1 ± 0.7 days for the early-initiation group and 6.5 ± 2.5 days for the delayed-initiation group (p < 0.01). JFT was the leading route of enteral feeding in both groups. Patients in the early-initiation group were less likely to receive supplemental PN than patients in the delayed-initiation group (28.6 vs. 66.7 %, p < 0.01). Furthermore, patients in the early-initiation group receive significantly higher daily enteral calory than patients in the delayed-initiation group from day 2 to day 8 in SICU (Fig. 2), whereas calory from PN was similar between the two groups (Fig. 3).
Feeding intolerance was common in both groups, with 15 (53.6 %) patients in the early-initiation group and 26 (43.3 %) in the delayed-initiation group having at least one episode of feeding intolerance. Of note, there was no difference in the incidence of feeding intolerance between the two groups (p = 0.37). In addition, disruption of enteral feeding due to persistent feeding intolerance was uncommon, occurring in two (7.1 %) patients in the early-initiation group and three (5 %) in the delayed-initiation group (p = 0.65).
Clinical outcomes
All patients but seven in the early-initiation group and one in the delayed-initiation group underwent emergency laparotomy. No difference was found in mortality at 28 days between the early-initiation group and the delayed-initiation group (0 vs. 5 %, p = 0.55). Length of stay in SICU (7.5 vs. 11 days, p < 0.01) and hospital (9 vs. 13 days, p < 0.01) were significantly shorter in the early-initiation group than the delayed-initiation group. In terms of infectious complications, the percentage of patients having at least one infectious complication was significantly lower in the early-initiation group than the delayed-initiation group (17.9 vs. 40 %, p = 0.04). There were no differences in the incidence of pneumonia, intra-abdominal abscess, wound infection, and bacteremia between the two groups.
Discussion
This cohort study compared early versus delayed enteral feeding in patients with abdominal trauma. Our results showed that early enteral feeding, delivered within 72 h of SICU admission, could be implemented without risk of increasing feeding intolerance in these patients. Moreover, early enteral feeding was associated with improved clinical outcomes including lower infectious complications and reduced length of stay in SICU and hospital. These findings support the administration of early enteral feeding in patients with abdominal trauma.
Enteral nutrition is superior to PN because of its potential in preserving mucosal integrity and modulating immune response. Recent clinical practice guidelines have recommended initiation of enteral feeding within 24–48 h of ICU admission in critically ill patients [11, 12]. However, it is challenging to adhere to the guideline recommendations in providing early enteral feeding to some patient populations, such as patients with abdominal trauma. Reluctance may exist in delivering early EN to these patients because of fear of feeding-associated complications.
While previous studies have showed that EN could be delivered at as early as 12 h after operation [15, 16] or 24 h after injury [17] in patients with abdominal trauma, a critical evaluation of our nutrition practice suggested that early administration of EN could be difficult, as indicated by implementation of enteral feeding within 72 h of SICU admission in only 31.8 % of patients in this cohort. A major reason for our hesitance to introduce early enteral is fear of feeding intolerance, which was found to be common in both patients receiving early enteral feeding (57.1 %) and delayed enteral feeding (43.3 %). Abdominal distention is the major event of feeding intolerance, arising in 14 (50 %) patients in the early-initiation group and 19 (31.7 %) in the delayed-initiation group. This is similar with the previous finding of a meta-analysis including high-risk surgical patients, of whom the majority were trauma patients, that the incidence of abdominal distention could be as high as 46 % in patients receiving total EN within 72 h after operation [18]. We believed that the frequent occurrence of feeding intolerance might be associated with the impaired gastrointestinal function as a result of hit of trauma, operation, and massive fluid resuscitation. This was supported by the significant higher abdominal AIS (p = 0.02) in patients having feeding intolerance than those who did not, and a trend towards higher incidence of feeding intolerance in patients undergoing surgery (50 vs. 12.5 %). Moreover, the frequent development of feeding intolerance might explain the consistent enteral underfeeding during the first week in SICU.
However, it is noteworthy that feeding intolerance was relieved after lowering the rate of enteral feeding in the majority of patients, as evidenced by low frequency of disruption of enteral feeding in both the early-initiation group (7.1 %) and the delayed-initiation group (5 %). Furthermore, incidence of feeding intolerance was not significantly different between the two groups (p = 0.23), indicating that early enteral feeding did not increase feeding intolerance. These findings suggest the safety of early enteral feeding in patients with abdominal trauma, and may promote the implementation of early enteral feeding in our future nutrition practice in abdominal trauma management.
In consistent with the results of previous studies enrolling critically ill and trauma patients [15, 19], the present study demonstrated that early enteral feeding was associated with reduced infectious complications compared to delayed enteral feeding in patients with abdominal trauma. There are two possible explanations for this finding. First, EN has the potential to maintain gut barrier integrity and prevent bacterial translocation. In patients with abdominal trauma, bacterial translocation may occur at as early as the onset of laparotomy, as evidenced by positive culture of mesenteric lymph node obtained during laparotomy [20]. Given the association between bacterial translocation and infectious complications, early enteral feeding may be better than delayed enteral feeding in preventing infectious complications resulted from gut barrier dysfunction and bacterial translocation at the early phase after injury. Second, early enteral feeding may reduce the risk of infection associated with supplemental PN. In a retrospective cohort study of patients with severe blunt trauma, Sena et al. [21] found that supplemental PN within 7 days of injury was associated with increased nosocomial infections. In the present study, patients in the early-initiation group were less likely to receive supplemental PN than those in the delayed-initiation group (28.6 vs. 66.7 %, p < 0.01). Therefore, it was possible that the reduction of infectious complications in the early-initiation group was associated with the lower requirement for supplemental PN.
Another finding of this study was that patients receiving early enteral feeding had higher enteral calory intake than those receiving delayed enteral feeding during the first week in SICU. This was not surprising given the early initiation of enteral feeding in this group and the same strategy in advancing enteral feeding in the two groups. However, we were not able to establish the potential association between the increase of enteral calory intake and the improved clinical outcomes in the early-initiation group. To date, optimal amount of enteral feeding remains controversial. A number of observational studies have demonstrated improved clinical outcomes including reduced infectious complications, lower mortality, and shorter duration of mechanical ventilation days in patients receiving a higher percentage of calory requirement [22], whereas conflicting results were reported by other authors [23]. Furthermore, a recent multicenter randomized study of patients with acute lung injury showed that initial permissive hypocaloric feeding did not improve ventilator-free days, infectious complications, and mortality. Given the evidence in the current literature, it is uncertain whether the increased enteral calory intake contributed to improved clinical outcomes in patients of the early-initiation group, but this merits further investigation.
We also found in this study that early enteral feeding was associated with reduced length of stay in SICU and hospital. The reduction of infectious complications and increase of enteral calory intake might be two major contributors to the shorter stay in SICU and hospital. Infectious complication is one of the major factors leading to prolonged stay in ICU and hospital, and adequate enteral calory intake is an important factor contributing to the decision of discharge. However, no significant difference in mortality at 28 days was found between patients receiving early and delayed enteral feeding in this study. This might be explained by the small sample size and moderate injury severity in overall.
Several limitations are noteworthy when interpreting the results of this study. The first limitation was the retrospective nature of this study, due to which we failed to achieve two identical patient groups, as shown by the differences in injury mechanism, injured organs, and need for emergency laparotomy between the two groups. Moreover, the decision of initiating enteral feeding was based on the judgment of the patient’s clinical situation by the treating surgeon or SICU specialist. Although the severity of injury and illness was similar between the two groups, as suggested by similar ISS and APACHE II, the variation in judgment between treating clinicians might influence the result of this study. Second, the small sample size undermined the power of this study. Moreover, 66 patients were excluded due to absence of enteral feeding in SICU. The majority of these patients were transferred to surgical wards within 3 days of admission, where nutritional support was provided. Since nutritional support protocol was not available in these patients, we did not include them in final analysis or set up a third group including them. Third, the influence of supplemental PN on clinical outcomes could not be eliminated. PN has been shown to be associated with adverse effects in critically ill trauma patients [21]. Since there were patients receiving supplemental PN in both groups, the effect of PN must be taken into consideration when interpreting the results. Finally, variability existed in the route of enteral feeding in this cohort, which might affect the outcomes given the potential benefits of postpyloric feeding [24].
Conclusion
This retrospective cohort study demonstrated that early enteral feeding, initiated within 72 h of SICU admission, was associated with lower infectious complications and reduced length of stay in SICU and hospital without increasing risk of feeding intolerance compared to delayed enteral feeding in patients with abdominal trauma. Prospective studies with larger sample size are needed to confirm the safety and benefits of early enteral feeding in patients with abdominal trauma.
Abbreviations
- SICU:
-
Surgical intensive care unit
- EN:
-
Enteral nutrition
- PN:
-
Parenteral nutrition
- ICU:
-
Intensive care unit
- ER:
-
Emergency room
- NGT:
-
Nasogastric tube
- NJT:
-
Nasojejunal tube
- JFT:
-
Jejunostomy feeding tube
- BMI:
-
Body mass index
- ISS:
-
Injury severity score
- AIS:
-
Abbreviated injury scale
- APACHE II:
-
Acute physiology and chronic health evaluation II
References
Uehara M, Plank LD, Hill GL. Components of energy expenditure in patients with severe sepsis and major trauma: a basis for clinical care. Crit Care Med. 1999;27(7):1295–302.
Goiburu ME, Goiburu MM, Bianco H, Diaz JR, Alderete F, Palacios MC, et al. The impact of malnutrition on morbidity, mortality and length of hospital stay in trauma patients. Nutr Hosp. 2006;21(5):604–10.
Todd SR, Kozar RA, Moore FA. Nutrition support in adult trauma patients. Nutr Clin Pract. 2006;21(5):421–9.
Weissenfluh GM, Brundage SI, Spain DA. Early enteral nutrition after abdominal trauma: effects on infectious morbidity and practicality. Nutr Clin Pract. 2006;21(5):479–84.
Doig G, Heighes P, Simpson F, Sweetman E, Davies A. Early enteral nutrition, provided within 24 h of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: a meta-analysis of randomised controlled trials. Intensive Care Med. 2009;35(12):2018–27.
Chuntrasakul C, Siltharm S, Chinswangwatanakul V, Pongprasobchai T, Chockvivatanavanit S, Bunnak A. Early nutritional support in severe traumatic patients. J Med Assoc Thai. 1996;79(1):21–6.
Kompan L, Vidmar G, Spindler-Vesel A, Pecar J. Is early enteral nutrition a risk factor for gastric intolerance and pneumonia? Clin Nutr. 2004;23(4):527–32.
Doig GS, Heighes PT, Simpson F, Sweetman EA. Early enteral nutrition reduces mortality in trauma patients requiring intensive care: a meta-analysis of randomised controlled trials. Injury. 2011;42(1):50–6.
Blesa Malpica AL, Garcia de Lorenzo y Mateos A, Robles Gonzalez A, Metabolism and Nutrition Working Group of the Spanish Society of Intensive Care Medicine and Coronary units. Guidelines for specialized nutritional and metabolic support in the critically-ill patient: update. Consensus SEMICYUC-SENPE: multiple trauma patient. Nutr Hosp. 2011;26(Suppl 2):63–6.
Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P, Canadian Critical Care Clinical Practice Guidelines C. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr. 2003;27(5):355–73.
Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, et al. ESPEN guidelines on enteral nutrition: intensive care. Clin Nutr. 2006;25(2):210–23.
McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2009;33(3):277–316.
Ilan R, Fowler RA, Geerts R, Pinto R, Sibbald WJ, Martin CM. Knowledge translation in critical care: factors associated with prescription of commonly recommended best practices for critically ill patients. Crit Care Med. 2007;35(7):1696–702.
Cahill NE, Dhaliwal R, Day AG, Jiang X, Heyland DK. Nutrition therapy in the critical care setting: what is “best achievable” practice? An international multicenter observational study. Crit Care Med. 2010;38(2):395–401.
Moore EE, Jones TN. Benefits of immediate jejunostomy feeding after major abdominal trauma—a prospective, randomized study. J Trauma. 1986;26(10):874–81.
Moore FA, Moore EE, Jones TN, McCroskey BL, Peterson VM. TEN versus TPN following major abdominal trauma–reduced infectious morbidity. J Trauma. 1989;29(7):916–22 discussion 22–23.
Kudsk KA, Croce MA, Fabian TC, Minard G, Tolley EA, Poret HA, et al. Enteral versus parenteral feeding. Effects on infectious morbidity after blunt and penetrating abdominal trauma. Ann Surg. 1992;215(5):503–11 discussion 11–13.
Moore FA, Feliciano DV, Andrassy RJ, McArdle AH, Booth FV, Morgenstein-Wagner TB, et al. Early enteral feeding, compared with parenteral, reduces postoperative infectious complications. The results of a meta-analysis. Ann Surg. 1992;216(2):172–83.
Woo SH, Finch CK, Broyles JE, Wan J, Boswell R, Hurdle A. Early vs delayed enteral nutrition in critically ill medical patients. Nutr Clin Pract. 2010;25(2):205–11.
Nieves E, Tobon LF, Rios DI, Isaza A, Ramirez M, Beltran JA, et al. Bacterial translocation in abdominal trauma and postoperative infections. J Trauma. 2011;71(5):1258–61.
Sena MJ, Utter GH, Cuschieri J, Maier RV, Tompkins RG, Harbrecht BG, et al. Early supplemental parenteral nutrition is associated with increased infectious complications in critically ill trauma patients. J Am Coll Surg. 2008;207(4):459–67.
Rubinson L, Diette GB, Song X, Brower RG, Krishnan JA. Low caloric intake is associated with nosocomial bloodstream infections in patients in the medical intensive care unit. Crit Care Med. 2004;32(2):350–7.
Arabi YM, Haddad SH, Tamim HM, Rishu AH, Sakkijha MH, Kahoul SH, et al. Near-target caloric intake in critically ill medical-surgical patients is associated with adverse outcomes. JPEN J Parenter Enteral Nutr. 2010;34(3):280–8.
Zhang Z, Xu X, Ding J, Ni H. Comparison of postpyloric tube feeding and gastric tube feeding in intensive care unit patients: a meta-analysis. Nutr Clin Pract. 2013;28(3):371–80.
Acknowledgments
This work was supported by grant from the National Natural Science Foundation of China (No. 81270945).
Conflict of interest
Jianyi Yin, Jian Wang, Shaoyi Zhang, Danhua Yao, Qi Mao, Wencheng Kong, Lele Ren, Yousheng Li, and Jieshou Li declare that they have no conflict of interest.
Ethical standard
This study was approved by the institutional ethics committee and was therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was waived because of the retrospective observational nature of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yin, J., Wang, J., Zhang, S. et al. Early versus delayed enteral feeding in patients with abdominal trauma: a retrospective cohort study. Eur J Trauma Emerg Surg 41, 99–105 (2015). https://doi.org/10.1007/s00068-014-0425-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-014-0425-4