Abstract
Background
Serial rib fractures and flail chest injury can be treated by positive-pressure ventilation. Operative techniques reduce intensive care unit (ICU) stay, overall costs, mortality and morbidity, as well as pain. The aim of this study was to evaluate the benefit of surgical rib stabilisation in comparison to non-operative treatment in patients with severe trauma of the chest wall.
Materials and methods
From 2006 to 2011, the data of 44 patients with flail chest and serial rib fractures were collected retrospectively. A surgical group and an intensive care group with only intensive care therapy were formed. Rib and sternal fractures, flail chest, injury severity, thoracic injuries, mechanical ventilation, time in the ICU, overall hospital stay and mortality were evaluated.
Results
No postoperative surgical complications had been observed. The time under mechanical ventilation in the surgical group was 10.6 ± 10.2 days, whereas in the non-surgical group, it was 13.7 ± 13.7 days. Mechanical ventilation time after surgery was 6.9 ± 6.5 days. Time in the ICU for the surgical group was 16.4 ± 13.6 days, compared to the non-surgical group with 20.1 ± 16.2 days. Postoperative time in the ICU was 11.7 ± 10.3 days. The mortality in the surgical group was 10 % and in the non-surgical group it was 17 %.
Conclusions
Operative rib stabilisation with plates is a safe therapy option for severe trauma of the chest wall. Provided that the duration of preoperative mechanical ventilation and time spent in the ICU is minimised due to early operation, our data suggest that the stabilisation of serial rib fractures and flail chest may lead to a reduced time of mechanical ventilation, time in the ICU and mortality.
Similar content being viewed by others
Introduction
The management of rib fractures and flail chest injury is still a subject of controversy for orthopaedic and trauma surgeons.
In 1956, Avery et al. [1] were the first to report on the “internal splinting” of flail chest segments, using positive-pressure ventilation with improved outcomes in comparison to existing conservative and operative techniques. From the mid-1970s to the mid-1980s, positive-pressure ventilation as well as treatment without mechanical ventilatory support was advocated [2–4]. However, positive-pressure ventilation resulted in prolonged time under mechanical ventilation, leading to ventilator-associated pneumonia and mortality rates of 10–36 % [5–7]. In addition, positive-pressure ventilation led to painful non-union of fractured ribs and symptomatic chest wall deformity, resulting in volume loss and atelectasis [8, 9]. Thus, non-operative treatment with and without mechanical ventilation caused long-term disability, with chest wall pain and deformity, reduction of activity levels and shortness of breath [6, 7, 10].
From the mid-1970s onwards, different techniques for operative rib stabilisation have been reported. Various plates and different techniques of pinning were used, which, in general, improved results relative to non-surgical historical control groups [8, 9, 11–16]. The operative repair of severe chest wall injury restores chest wall integrity, improves pulmonary function and is associated with lower rates of long-term morbidity and pain [17]. Several studies reported a reduction in mortality and morbidity due to surgical stabilisation [7, 18–21]. Ten years ago, Tanaka et al. [19] presented a randomised controlled trial comparing surgical stabilisation to conservative treatment using internal pneumatic stabilisation. They were able to show a reduction of nosocomial pneumonia, duration of ventilatory support, length of intensive care unit (ICU) stay, medical costs and a quicker return to work in their surgical group. Despite numerous reports suggesting beneficial outcomes for patients after operative rib stabilisation, indications for surgery are still varying [7, 9, 13, 16, 22]. Newly available materials and techniques for rib fracture repair have brought surgical rib stabilisation into focus once again [20, 23–26].
The aim of this non-randomised study was to evaluate the benefit of surgical rib stabilisation in comparison to non-operative treatment in patients with severe trauma of the chest wall.
Materials and methods
From January 2006 to December 2011, the data of 44 patients with flail chest and serial rib fractures were collected retrospectively and made anonymous. Medical confidentiality was applied. Approval from the local study/ethical committee was obtained.
In 21 patients, surgery to stabilise the rib cage was performed, while 23 patients underwent non-operative treatment with intensive care therapy. Two treatment groups have been compared:
-
A surgical group, which consisted of 21 patients with surgical rib repair
-
A non-surgical group, which consisted of 23 patients with intensive care therapy (Table 1).
All patients were treated at a level-I trauma centre according to the criteria established by the American College of Surgeons (ACS) with a 24-h computed tomography (CT) and operating capacity. Trauma care was provided according to the principles of Advanced Trauma Life Support (ATLS™) and damage control surgery [27]. Apart from chest tubes, no emergency thoracotomy had to be carried out in the emergency room. Demographic data were recorded, as well as the mechanisms of injury, the American Society of Anesthesiologists (ASA) classification [28], the Injury Severity Score (ISS) [29], the Abbreviated Injury Scale (AIS) of the thorax [30], time on the ventilator, time in the ICU, time from hospital admission until surgery, length of overall hospital stay and clinical mortality. Patients who were extubated on the day of surgery were not considered as postoperatively ventilated.
Rib fractures, thoracic injuries and mechanical ventilation
The number and location of rib fractures, sternal fracture and flail chest, pneumo- and haemothorax, as well as lung contusion were assessed using a CT scan of the thorax. The degree of pulmonary contusion was classified as “mild” if an infiltrate involved less than one segment, “moderate” if the infiltrate was more than one segment but less than a lobe, and “severe” if the infiltrate was involving more than one lobe. In cases where no CT scan of the thorax was available, the same criteria were applied for the evaluation of pulmonary contusion using conventional X-ray of the thorax [31]. Every patient of the surgical and non-surgical group underwent an emergency CT scan. The need for a chest tube and mechanical ventilation immediately after the injury was documented, as well as the need for tracheotomy during intensive care therapy. Pneumonia was diagnosed according to Tanaka et al. [19] by the following criteria: purulent expectorate or tracheal aspirate, continued fever >38 °C, leucocytosis >10,000/μl and infiltrate shadows on chest radiographs.
Operative treatment
Every single operation was the result of an individual decision process. The decision for surgery was made under agreement of the anaesthetist in the ICU and the trauma surgeon on duty, with approval from the head of the department for trauma surgery.
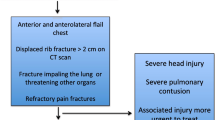
At the beginning of the study period, the diagnosis of failure of respiratory weaning and a thoracotomy because of associated thoracic injuries led to the indication for operative chest wall stabilisation. Due to positive experience during the study period, indication 3 (see below) was added. In summary, three different indications led to the decision of surgical rib stabilisation in order to treat acute chest wall injuries:
-
1.
Patients who required a thoracotomy because of associated thoracic injuries
-
2.
Patients with flail chest and uni- or bilateral serial rib fractures with respiratory failure and deteriorating pulmonary function (with or without pulmonary contusion) (Fig. 1)
Fig. 1 Flail chest pre- and postoperatively with angle-stable 3.5-mm 1/3 tubular plates a Preoperative three-dimensional computed tomography (CT) image reconstruction. b Postoperative three-dimensional CT image reconstruction. c Preoperative chest radiograph with chest wall deformity of the left hemithorax. d, e Postoperative chest radiographs after restoring the chest wall
-
3.
Patients with massive dislocations of fractured ribs and irritation of underlying organs, e.g. lung, liver or spleen, and consecutive pulmonary affection, e.g. pneumo-, haemo- or serothorax (Fig. 2)
A lateral approach was performed to expose the ribs. In general, the latissimus dorsi muscle was identified and retracted dorsally. If it was not possible to reach the dorsal parts of the ribs, the muscle was dissected and divided, as well as the serratus anterior muscle. The fractured ribs were exposed and care was taken not to strip the periosteum. The ribs were restored and angle-stable 3.5-mm 1/3 tubular plates were used for internal fixation (Synthes™, Umkirch, Germany). The number of stabilised ribs depended on their accessibility. For our study, the first three and last two ribs were never stabilised, since it is known that these rib do not contribute to the overall stability of the chest cage. A chest tube was inserted before closing the soft tissue.
Data collection included the number of plates used per patient, the number of ribs stabilised with two plates, the overall surgery time, as well as surgical complications.
Statistical methods
Microsoft Excel™ software was used for collecting the data. Thereafter, the data were imported into SAS™ system, release 9.2 (SAS Institute Inc., Cary, NC, USA) for statistical analysis. Frequencies are given in absolute numbers and percentages. The percentages were rounded to the nearest integer. Quantitative variables are presented by their mean value, together with the median, range and standard deviation (SD). In order to compare the frequencies of two groups, the Chi-square test or Fisher’s exact test was used, as appropriate. For ordinal-scaled data, the Cochran–Armitage trend test was performed. Quantitative variables which were approximately normally distributed were compared with a two-sample t-test. For variables with skewed distribution (i.e. hospitalisation time or time in the ICU), the Mann–Whitney U-test was used.
Testing for significance was always two-sided. A test result with p < 0.05 was considered to be statistically significant.
Results
Cohort, mechanism of injury and injury severity
The test results of the surgical group and the non-surgical group are presented in Table 1. There was no statistically significant difference regarding patients’ average age and sex. About the same proportion of patients in the surgical group (71 %) and the non-surgical group (74 %) had severe mechanisms of injury. In both groups, the ISS and AIS were approximately the same. The average ISS was that of a polytraumatised patient (>16). No significant differences concerning the number of rib fractures of both hemithoraces, bilateral rib fractures, flail chest, sternal fractures, pulmonary contusion, pneumo- and haemothorax, and the number of chest tubes inserted immediately after the injury were found. The total number of rib fractures was significantly higher (p = 0.05) in the surgical group; however, the difference was rather small (median values of 8 and 7) (Table 1). At the same time, significantly (p = 0.004) more patients of the non-surgical group were intubated and mechanically ventilated immediately after the injury. However, the need for tracheotomy during mechanical ventilation showed no significant difference (Table 2).
Ventilation time, time in the ICU, hospital stay and mortality
In the surgical group, 16 patients (76 %) and in the non-surgical group, 21 patients (91 %) were ventilated. The results were not statistically significantly different. The ventilation and hospitalisation times are presented in Table 2. The average time of mechanical ventilation in the surgical group was about 3 days shorter than in the non-surgical group, but, due to high variability, the difference was not statistically significant. The mechanical ventilation time after surgery was about half the ventilation time in the non-surgical group but was not significantly different (p = 0.09) (Table 2).
The average time spent in the ICU for the surgical group was about 4 days shorter compared to the non-surgical group, but, again, due to high variability, the difference was not statistically significant. However, the postoperative time in the ICU was about half compared to the total time in the ICU of the non-surgical group. The p-value was not statistically significantly different (p = 0.07). The total length of time of hospital stay for both groups was the same and did not show any difference (Table 2).
In the non-surgical group, the mortality rate (n = 4, 17 %) was higher than the rate of the surgical group (n = 2, 10 %), but this was not statistically significant (Table 2).
Rib stabilisation
Surgery was performed at 7.1 ± 4.4 days (median 6; range 1–15) after injury. On average, 3.7 plates (median 4; range 1–6) per patient were implanted. The average duration of operation was 89.3 min, with a range from 35 min for the implantation of one plate to 130 min in a patient receiving six plates. No postoperative surgical complications were observed.
Implant costs
The average price for an angle-stable 3.5-mm 1/3 tubular plate is 2 EUR, ranging from 21.76 EUR for a four-hole plate to 27.59 EUR for a ten-hole plate. The same average price accounts for a single angle-stable screw. Thus, the average costs for one plate with five screws is about 150 EUR. The average implant cost for one patient (3.6 plates per patient) accounts for 540 EUR and it was 600 EUR for four plates.
Discussion
Indications for rib stabilisation
Indications leading to surgical rib stabilisation have been described in detail above. Several authors have tried to standardise indications for surgical rib stabilisation. Our indications 1 and 2 are almost concordant with the indications published by Lardinois et al. [7], Quell and Vécsei [13], Schmit-Neuerburg et al. [9], Voggenreiter et al. [16] and Casali et al. [22]. Lardinois et al. [7] and Schmit-Neuerburg et al. [9] consider severe pulmonary contusion as a contraindication for surgical rib stabilisation. Voggenreiter et al. [16] and Casali et al. [22] have different indications for patients with and without pulmonary contusion. Lung contusions lead to a parenchyma-dependent reduction of gas exchange and have a high risk for the development of pneumonia. Pulmonary contusion does not necessarily contradict surgical rib stabilisation treatment [8]. Although surgical rib stabilisation does not address lung contusions directly, a stable chest benefits more from resuscitation compared to an unstable chest due to restored chest wall motility [7, 18–21]. In addition, a stable chest wall is important for the patient to be able to breathe on their own [8]. Our indication 3 for rib stabilisation is concordant with Lardinois et al. [7].
Surgical procedure
Although stabilisation of every other rib was recommended [32], according to Gasparri et al. [26] and Lardinios et al. [7], we stabilised as many rib as we could get easy access to, with the exception of the first three and last two ribs, because they do not contribute to the overall stability of the chest cage. Stabilisation of a rib fracture prevents the development of non-union or pseudarthrosis and, therefore, reduces pain [26]. In addition, the fixation of all accessible fractures restores anatomic chest wall contour to the greatest degree, minimises volume loss and maximises the biodynamics of the chest wall [26]. When fixing a flail chest segment, both sides have to be fixed in order not to convert a flail chest to serial rib fracture [26]. Other authors like Casali et al. [22] consider it enough to convert a flail chest to a simple serial rib fracture. Like Gasparri et al. [26], in a flail chest, we fix at least one rib at both fracture sites in order to gain stability.
Lardinios et al. [7] reported on two superficial wound infections in 66 patients with operative chest wall stabilisation. We did not find any postoperative surgical complications in our study. Granetzny et al. [18], Tanaka et al. [19] and Gasparri et al. [26] did not report on postoperative surgical complications either.
Group demographics
The demographic data of the surgical and non-surgical groups were not significantly different. Except for the total number of fractured ribs, there was no difference between the two groups with respect to the injury severity of the chest (Table 1). The data of our two groups are similar to the groups of Tanaka et al. [19]. Our groups consisted of 21 and 23 patients, respectively, with a mean ISS of 36 in both groups and a number fractured ribs of 9.2 and 7.3, respectively. Tanaka et al. [19] reported on two groups with 18 and 19 patients, respectively, having an ISS of 33 and 30, respectively, and the number of fractured ribs summed to 8.2 for both groups.
Ventilation time, time in the ICU and hospital stay
Overall, surgical rib stabilisation leads to an improvement of respiratory mechanics, with a reduction in the duration of ventilatory support and ventilator-associated pneumonia, length of ICU stay, medical costs and mortality [7, 18–21]. However, in contrast to Tanaka et al. [19], we did not observe any differences in the need for tracheostomy or the presence of pneumonia for both of our groups.
With respect to the time from injury to surgery, we observed similar results (7.1 ± 4.4 days) to those reported by Tanaka et al. (8.2 ± 4.1 days) [19]. Patients profit from early surgical therapy. Prolonged time of mechanical ventilation leads to ventilator-associated pneumonia and mortality rates of up to 36 % [5–7]. That is the reason why, today, we regard a time period from injury to surgery of about 1 week as being too long. As for our study, the reason for an average time period until surgery of 1 week was due to our cautious attitude towards operative measures initially. Based on our positive experience, the decision for surgery is much faster today than at the beginning of our study period. Now, we are aiming to operate on patients with flail chest within 3 days after admission. Due to a faster decision at the end of the study period, 60 % of the patients were operated within 4 days after hospital admission. The earlier the decision for operative treatment with a reduction of preoperative ventilation time and time in the ICU, the higher the differences in the total mechanical ventilation time and time in the ICU between the two groups (Table 2).
Tanaka et al. [19] observed a relevant longer mean preoperative ventilation time (8.3 days) compared to our results (3.7 days). Furthermore, they reported a short average ventilation time of 2.5 days after surgery. In contrast, the mean postoperative ventilation time in our surgical group was 6.9 days (Table 2). Nevertheless, the mean duration of mechanical ventilation in our surgical group (10.6 days) was about the same as that described by Tanaka et al. [19] (10.8 days). Granetzny et al. [18] reported a much shorter mean ventilation time of 2 days for their surgical group. When comparing our mechanical ventilation time after surgery (6.9 ± 6.5 days) with the total time of mechanical ventilation of the non-surgical group (13.2 ± 13.7 days), it was about half. The p-value was 0.09, which was not statistically significant (Table 2). Provided that preoperative mechanical ventilation is minimised due to early operation, the p-value suggests a tendency to a shorter total time of mechanical ventilation in the surgical group. The total time under mechanical ventilation of our non-surgical group (13.2 days) was similar to that reported by Granetzny et al. [18] (12 days). Similarly, Tanaka et al. [19] observed a longer mean ventilation time of 18.3 days for their internal group (Table 2).
Tanaka et al. [19] reported a similar mean time in the ICU of 16.5 days compared to our results, with a total time in the ICU of 16.4 days for the surgical group. Similarly, Granetzny et al. [18] reported a shorter time of 9.6 days in the group with rib stabilisation. In our study, the postoperative time in the ICU (11.7 ± 10.3 days) was about half compared to the total time in the ICU of the non-surgical group (20.1 ± 16.2 days). The p-value was 0.07, which was not statistically significant (Table 2). Provided that the preoperative time in the ICU is minimised due to early operation, the p-value suggests a tendency to a shorter total postoperative time in the ICU of the surgical group. As for non-surgical treatment, we observed a mean time in the ICU of 20.1 days, which was between the time periods of Granetzny et al. (14.6 days) [18] and Tanaka et al. (26.8 days) [19].
Furthermore, an early decision for surgery with reduced ventilation time and time in the ICU minimises the total time of mechanical ventilation and, consequently, the total time in the ICU, which will approximate our results to that of Granetzny et al. [18].
In addition, Granetzny et al. [18] reported a duration of hospital stay for the surgical group that was half as much compared to the non-surgical group (11.7 vs. 23.1 days). In our study, the mean total time of hospital stay of both groups was about the same (31.8 vs. 30.0 days) (Table 2).
Mortality
Although this was not a randomised study, mortality in the non-surgical group (17 %) was higher than in the surgical group (10 %); however, the difference was not statistically significant (Table 2).
Those two patients of the surgical group that contributed to the mortality rate had an ASA classification score of 4 and an AIS of 5. A 70-year-old man had an ISS of 29 and died 16 days after rib stabilisation. He suffered from severe systemic diseases, including chronic renal failure and dialysis, heart failure and arrhythmia due to myocardial infarction, massive obesity [body mass index (BMI) > 40] and diabetes. Another 78-year-old man had an initial ISS of 33 and died 7 days after operation. He suffered from severe systemic diseases, with heart failure due to coronary heart disease, massive obesity (BMI > 40) and diabetes.
For the non-surgical group, those four patients that lead to the mortality rate of 17 %, the mean age was 59.5 years (range 25–79 years). The ASA classification score ranged from 2 to 4, with a mean of 3.5 (median 4). The mean ISS was 46.5 (median 51; range 25–59). All patients had severe thoracic injuries, with an AIS of 5. On average, these patients died in the ICU after 18 days (median 16; range 10–40 days) post injury. Three of the deceased patients had an ASA classification score of 4, with severe systemic diseases. One 54-year-old man had an ASA classification score of 2. The ISS was 57. Besides his severe thoracic injuries, he had suffered from severe traumatic liver disruption. He underwent multiple abdominal operations due to prolonged intra-abdominal bleeding. All patients died from pulmonary insufficiency due to septic multiple-organ failure.
The mortality in our study was similar to the observations of Granetzny et al. [18]. They reported a mortality rate of 10 % for their surgical group and 15 % for their non-surgical group, which also was not significantly different.
Limitations
A limitation of our study, as well as the majority of studies reported in the literature so far, is the fact that it is based on a retrospective data analysis, involving only a limited number of patients. The basis of this study is clinical experience and not a formal randomised controlled trial. Thus, statistical significance has to be interpreted carefully.
When comparing different studies, certain limitations need to be taken into consideration. In our study, all the patients included suffered from more than just an injury to the chest. Concomitant injuries as well as pre-existing severe systemic diseases influence the overall therapy relevantly. In most of our cases, injuries of body regions other than the chest and consecutive operations counted for longer ventilation time and, respectively, longer time in the ICU. Therefore, when comparing different studies with regard to ventilation time, time in the ICU and overall hospital stay, as well as medical costs, this needs to be taken into consideration. Thus, presumable long-term sequelae such as chest wall pain, restrictive pulmonary function with consecutive reduction of activity and shortness of breath might be better indicators for the benefit of surgical rib stabilisation. Our future work is dedicated towards the evaluation of chest wall pain, pulmonary function and activity level in patients with severe thoracic trauma and flail chest injury.
Another limitation that needs to be taken into consideration when comparing different studies is related to outcomes between different therapeutic strategies. Obviously, randomised controlled trails are the best way to achieve high evidence. Still, it might be difficult to reach high numbers of selective patients that require surgical rib stabilisation, since single centres lack a high number of overall patient collectives. Only large multi-centre trials might be an option to reach results that reflect high evidence and, thereby, reveal new or better therapeutic strategies.
Conclusion
Due to missing postoperative surgical complications and a lower mortality rate in the surgical group, we consider rib stabilisation with plates to be a safe therapy option for severe trauma of the chest wall. Provided that the preoperative time under mechanical ventilation and time in the ICU is minimised due to a faster decision for early operation, our data suggest that operative treatment strategies of serial rib fractures and flail chest injury may lead to a reduced time under mechanical ventilation, time in the ICU and mortality.
References
Avery EE, Benson DW, Morch ET. Critically crushed chests; a new method of treatment with continuous mechanical hyperventilation to produce alkalotic apnea and internal pneumatic stabilization. J Thorac Surg. 1956;32:291–311.
Richardson JD, Adams L, Flint LM. Selective management of flail chest and pulmonary contusion. Ann Surg. 1982;196:481–7.
Shackford SR, Smith DE, Zarins CK, Rice CL, Virgilio RW. The management of flail chest. A comparison of ventilatory and nonventilatory treatment. Am J Surg. 1976;132:759–62.
Trinkle JK, Richardson JD, Franz JL, Grover FL, Arom KV, Holmstrom FM. Management of flail chest without mechanical ventilation. Ann Thorac Surg. 1975;19:355–63.
Cacchione RN, Richardson JD, Seligson D. Painful nonunion of multiple rib fractures managed by operative stabilization. J Trauma. 2000;48:319–21.
Landercasper J, Cogbill TH, Lindesmith LA. Long-term disability after flail chest injury. J Trauma. 1984;24:410–4.
Lardinois D, Krueger T, Dusmet M, Ghisletta N, Gugger M, Ris HB. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg. 2001;20:496–501.
Moore BP. Operative stabilization of nonpenetrating chest injuries. J Thorac Cardiovasc Surg. 1975;70:619–30.
Schmit-Neuerburg KP, Zerkowski HR, Hanke J. Stabilisierende operationen am thorax. Chirurg. 1986;57:1–14.
Beal SL, Oreskovich MR. Long-term disability associated with flail chest injury. Am J Surg. 1985;150:324–6.
Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. J Thorac Cardiovasc Surg. 1995;110:1676–80.
Hellberg K, de Vivie ER, Fuchs K, Heisig B, Ruschewski W, Luhr HG, Poutot M. Stabilization of flail chest by compression osteosynthesis—experimental and clinical results. Thorac Cardiovasc Surg. 1981;29:275–81.
Quell M, Vécsei V. Zur operativen Stabilisierung von Thoraxwandbrüchen. Unfallchirurg. 1991;94:129–33.
Sánchez-Lloret J, Letang E, Mateu M, Callejas MA, Catalán M, Canalis E, Mestres CA. Indications and surgical treatment of the traumatic flail chest syndrome. An original technique. Thorac Cardiovasc Surg. 1982;30:294–7.
Thomas AN, Blaisdell FW, Lewis FR Jr, Schlobohm RM. Operative stabilization for flail chest after blunt trauma. J Thorac Cardiovasc Surg. 1978;75:793–801.
Voggenreiter G, Neudeck F, Aufmkolk M, Obertacke U, Schmit-Neuerburg KP. Operative chest wall stabilization in flail chest—outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998;187:130–8.
Mayberry JC, Kroeker AD, Ham LB, Mullins RJ, Trunkey DD. Long-term morbidity, pain, and disability after repair of severe chest wall injuries. Am Surg. 2009;75:389–94.
Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4:583–7.
Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–32.
Fitzpatrick DC, Denard PJ, Phelan D, Long WB, Madey SM, Bottlang M. Operative stabilization of flail chest injuries: review of literature and fixation options. Eur J Trauma Emerg Surg. 2010;36:427–33.
Mouton W, Lardinois D, Furrer M, Regli B, Ris HB. Long-term follow-up of patients with operative stabilisation of a flail chest. Thorac Cardiovasc Surg. 1997;45:242–4.
Casali C, Fontana G, Morandi U. Surgical stabilization of severe flail chest. CTSNet editorial. http://www.ctsnet.org/sections/clinicalresources/thoracic/expert_tech-24.html. Accessed Dec 2007.
Bemelman M, Poeze M, Blokhuis TJ, Leenen LPH. Historic overview of treatment techniques for rib fractures and flail chest. Eur J Trauma Emerg Surg. 2010;36:407–15.
Bottlang M, Walleser S, Noll M, Honold S, Madey SM, Fitzpatrick D, Long WB. Biomechanical rationale and evaluation of an implant system for rib fracture fixation. Eur J Trauma Emerg Surg. 2010;36:417–26.
Bottlang M, Long WB, Phelan D, Fielder D, Madey SM. Surgical stabilization of flail chest injuries with MatrixRIB implants: a prospective observational study. Injury. 2013;44:232–8. doi:10.1016/j.injury.2012.08.011.
Gasparri MG, Tisol WB, Haasler GB. Rib stabilization: lessons learned. Eur J Trauma Emerg Surg. 2010;36:435–40.
American College of Surgeons Committee on Trauma. Advanced trauma life support for doctors. Student course manual. Chicago: American College of Surgeons; 2004.
American Society of Anesthesiologists (ASA). New classification of physical status. Anesthesiology. 1963;24:11.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Copes WS, Sacco WJ, Champion HR, Bain LW. Progress in characterising anatomic injury. In: Proceedings of the 33rd Annual Meeting of the Association for the Advancement of Automotive Medicine (AAAM), Baltimore, MD, USA, October 1989, p 205–18.
Freedland M, Wilson RF, Bender JS, Levison MA. The management of flail chest injury: factors affecting outcome. J Trauma. 1990;30:1460–8.
Trunkey DD. Chest wall injuries. In: Blaisdell FW, Trunkey DD, editors. Cervicothoracic trauma. 2nd ed. Stuttgart: Georg Thieme Verlag; 1994. p. 190–214.
Acknowledgments
We thank Dr. Marie Reumann, Brighton, Australia, very much for the linguistic revision of the manuscript.
Conflict of interest
None. There was no funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muhm, M., Härter, J., Weiss, C. et al. Severe trauma of the chest wall: surgical rib stabilisation versus non-operative treatment. Eur J Trauma Emerg Surg 39, 257–265 (2013). https://doi.org/10.1007/s00068-013-0262-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-013-0262-x