Abstract
Background
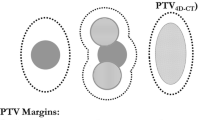
High-dose radiotherapy of lung cancer is challenging. Tumors may move by up to 2 cm in craniocaudal and anteroposterior directions as a function of breathing cycle. Tumor displacement increases with treatment time, which consequentially increases the treatment uncertainty.
Objective
This study analyzed whether automatically gated cone-beam-CT (CBCT)-controlled intensity modulated fast deep inspiration breath hold (DIBH) stereotactic body radiation therapy (SBRT) in flattening filter free (FFF) technique and normofractionated lung DIBH intensity-modulated radiotherapy (IMRT)/volumetric-modulated arc therapy (VMAT) treatments delivered with a flattening filter can be applied with sufficient accuracy within a clinically acceptable timeslot.
Materials and methods
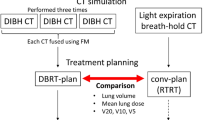
Plans of 34 patients with lung tumors were analyzed. Of these patients, 17 received computer-controlled fast DIBH SBRT with a dose of 60 Gy (5 fractions of 12 Gy or 12 fractions of 5 Gy) in an FFF VMAT technique (FFF-SBRT) every other day and 17 received conventional VMAT with a flattening filter (conv-VMAT) and 2-Gy daily fractional doses (cumulative dose 50–70 Gy).
Results
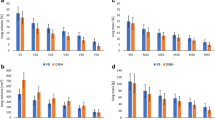
FFF-SBRT plans required more monitor units (MU) than conv-VMAT plans (2956.6 ± 885.3 MU for 12 Gy/fraction and 1148.7 ± 289.2 MU for 5 Gy/fraction vs. 608.4 ± 157.5 MU for 2 Gy/fraction). Total treatment and net beam-on times were shorter for FFF-SBRT plans than conv-VMAT plans (268.0 ± 74.4 s vs. 330.2 ± 93.6 s and 85.8 ± 25.3 s vs. 117.2 ± 29.6 s, respectively). Total slot time was 13.0 min for FFF-SBRT and 14.0 min for conv-VMAT. All modalities could be delivered accurately despite multiple beam-on/-off cycles and were robust against multiple interruptions.
Conclusion
Automatically gated CBCT-controlled fast DIBH SBRT in VMAT FFF technique and normofractionated lung DIBH VMAT can be applied with a low number of breath-holds in a short timeslot, with excellent dosimetric accuracy. In clinical routine, these approaches combine optimally reduced lung tissue irradiation with maximal delivery precision for patients with small and larger lung tumors.
Zusammenfassung
Hintergrund
Die Hochdosisstrahlentherapie des Bronchialkarzinoms ist eine Herausforderung. Bis zu 2 cm kann sich der Tumor in kraniokaudaler und anteroposteriorer Richtung bewegen – abhängig vom Atemzyklus. Die Tumorverschiebung nimmt mit der Behandlungsdauer zu, was also die Behandlungsunsicherheit vermehrt.
Ziel
In der vorliegenden Studie wurde untersucht, ob die automatisch gesteuerte, Cone-Beam-Computertomographie(CBCT)-kontrollierte, intensitätsmodulierte stereotaktische Strahlentherapie („stereotactic body radiation therapy“, SBRT) im Atemanhalt nach schneller tiefer Inspiration („deep inspiration breath hold“, DIBH) ohne Ausgleichskörper („flattening filter free“, FFF) und die mit einem Ausgleichskörper applizierte normal fraktionierte intensitätsmodulierte DIBH-Strahlentherapie/volumenmodulierte Strahlentherapie mit Rotation des Bestrahlungsarms („volumetric-modulated arc therapy“, VMAT) der Lunge mit ausreichender Genauigkeit innerhalb eines klinisch akzeptablen Zeitfensters angewendet werden können.
Material und Methoden
Die Bestrahlungspläne von 34 Patienten mit Bronchialkarzinomen wurden ausgewertet. Von diesen Patienten erhielten 17 eine computergesteuerte SBRT mit schneller DIBH und einer Dosis von 60 Gy (5 Fraktionen à 12 Gy oder 12 Fraktionen à 5 Gy) in FFF-VMAT-Technik (FFF-SBRT) jeden 2. Tag, und 17 erhielten eine konventionelle VMAT mit Ausgleichskörper (conv-VMAT) und täglichen Teildosen von 2 Gy (kumulative Dosis: 50–70 Gy).
Ergebnisse
Für Pläne mit FFF-SBRT waren mehr Überwachungseinheiten („monitor units“, MU) erforderlich als für Pläne mit con-VMAT (2956,6 ± 885,3 MU für 12 Gy/Fraktion bzw. 1148,7 ± 289,2 MU für 5 Gy/Fraktion vs. 608,4 ± 157,5 MU für 2 Gy/Fraktion). Die Dauer der Gesamttherapie und der Beam-on-Zeit („Strahl ein“) waren für FFF-SBRT-Pläne kürzer als für Pläne mit conv-VMAT (268,0 ± 74,4 s vs. 330,2 ± 93,6 s bzw. 85,8 ± 25,3 s vs. 117,2 ± 29,6 s). Das Gesamtzeitfenster betrug 13,0 min für FFF-SBRT und 14,0 min für conv-VMAT. Alle Therapiemodalitäten konnten genau appliziert werden – trotz mehrerer Beam-on-/-off-Zyklen – und waren bei mehrfachen Unterbrechungen stabil.
Schlussfolgerung
Automatisch gesteuerte CBCT-kontrollierte SBRT mit schneller DIBH in VMAT-FFF-Technik und normal fraktionierte DIBH-Lungen-VMAT können mit wenigen Malen Luftanhalten in einem kurzen Zeitfenster mit ausgezeichneter dosimetrischer Genauigkeit appliziert werden. Im klinischen Alltag wird bei diesen Ansätzen die optimal reduzierte Bestrahlung des Lungengewebes mit maximaler Bestrahlungspräzision für Patienten mit kleinen und größeren Bronchialkarzinomen kombiniert.


Similar content being viewed by others
References
Padda SK, Burt BM, Trakul N, Wakelee HA (2014) Early-stage non-small cell lung cancer: surgery, stereotactic radiosurgery, and individualized adjuvant therapy. Semin Oncol 41:40–56
Cykert S, Dilworth-Anderson P, Monroe MH, Walker P, McGuire FR, Corbie-Smith G, Edwards LJ, Bunton AJ (2010) Factors associated with decisions to undergo surgery among patients with newly diagnosed early-stage lung cancer. JAMA 303:2368–2376
Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, Fakiris A, Bezjak A, Videtic G, Johnstone D, Fowler J, Gore E, Choy H (2010) Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA 303:1070–1076
Fakiris AJ, McGarry RC, Yiannoutsos CT, Papiez L, Williams M, Henderson MA, Timmerman R (2009) Stereotactic body radiation therapy for early-stage non-small-cell lung carcinoma: four-year results of a prospective phase II study. Int J Radiat Oncol Biol Phys 75:677–682
Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, Fakiris A, Bezjak A, Videtic G, Choy H (2009) Stereotactic body radiation therapy for medically inoperable early-stage lung cancer patients: analysis of RTOG 0236. Int J Radiat Oncol Biol Phys 75:1092–1099
Aupérin A, Le Péchoux C, Rolland E, Curran WJ, Furuse K, Fournel P, Belderbos J, Clamon G, Ulutin HC, Paulus R, Yamanaka T, Bozonnat MC, Uitterhoeve A, Wang X, Stewart L, Arriagada R, Burdett S, Pignon JP (2010) Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol 28:2181–2190
Bradley J (2005) A review of radiation dose escalation trials for non-small cell lung cancer within the Radiation Therapy Oncology Group. Semin Oncol 32:111–113
Bradley JD, Paulus R, Komaki R, Masters GA, Forster K, Schild S, Bogart J, Garces YI, Narayan S, Kavadi V, Nedzi LA, Michalski JM, Johnson D, MacRae RM, Curran WJ, Choy H (2013) A randomized phase III comparison of standard-dose (60 Gy) versus high-dose (74 Gy) conformal chemoradiotherapy with or without cetuximab for stage III non-small cell lung cancer: Results on radiation dose in RTOG 0617. J Clin Oncol 31:Abstr 7501
Seppenwoolde Y, Shirato H, Kitamura K, Shimizu S, van Herk M, Lebesque JV, Miyasaka K (2002) Precise and real-time measurement of 3D tumor motion in lung due to breathing and heartbeat, measured during radiotherapy. Int J Radiat Oncol Biol Phys 53:822–834
Keall PJ, Cattell H, Pokhrel D, Dieterich S, Wong KH, Murphy MJ, Vedam SS, Wijesooriya K, Mohan R (2006) Geometric accuracy of a real-time target tracking system with dynamic multileaf collimator tracking system. Int J Radiat Oncol Biol Phys 65:1579–1584
Guckenberger M, Meyer J, Wilbert J, Baier K, Sauer O, Flentje M (2007) Precision of image-guided radiotherapy (IGRT) in six degrees of freedom and limitations in clinical practice. Strahlenther Onkol 183:307–313
Choi K, Xing L, Koong A, Li R (2013) First study of on-treatment volumetric imaging during respiratory gated VMAT. Med Phys 40:040701
Tahir BCM, Lawless SE, Hatton MQ, Ireland RH (2010) Dosimetric evaluation of inspiration and expiration breath-hold for intensity-modulated radiotherapy planning of non-small cell lung cancer. Phys Med Biol 55:N191–N199
Saito T, Sakamoto T, Oya N (2009) Comparison of gating around end-expiration and end-inspiration in radiotherapy for lung cancer. Radiother Oncol 93:430–435
Kontrisova K, Stock M, Dieckmann K, Bogner J, Pötter R, Georg D (2006) Dosimetric comparison of stereotactic body radiotherapy in different respiration conditions: a modeling study. Radiother Oncol 81:97–104
Boda-Heggemann J, Fleckenstein J, Lohr F, Wertz H, Nachit M, Blessing M, Stsepankou D, Löb I, Küpper B, Kavanagh A, Hansen VN, Brada M, Wenz F, McNair H (2011) Multiple breath-hold CBCT for online image guided radiotherapy of lung tumors: simulation with a dynamic phantom and first patient data. Radiother Oncol 98:309–316
Boda-Heggemann J, Frauenfeld A, Weiss C, Simeonova A, Neumaier C, Siebenlist K, Attenberger U, Heußel CP, Schneider F, Wenz F, Lohr F (2014) Clinical outcome of hypofractionated breath-hold image-guided SABR of primary lung tumors and lung metastases. Radiat Oncol 9:10
Panakis N, McNair HA, Christian JA, Mendes R, Symonds-Tayler JR, Knowles C, Evans PM, Bedford J, Brada M (2008) Defining the margins in the radical radiotherapy of non-small cell lung cancer (NSCLC) with active breathing control (ABC) and the effect on physical lung parameters. Radiother Oncol 87:65–73
Fu W, Dai J, Hu Y, Han D, Song Y (2004) Delivery time comparison for intensity-modulated radiation therapy with/without flattening filter: a planning study. Phys Med Biol 49:1535–1547
Stieler F, Fleckenstein J, Simeonova A, Wenz F, Lohr F (2013) Intensity modulated radiosurgery of brain metastases with flattening filter-free beams. Radiother Oncol 109:448–451
Navarria P, Ascolese AM, Mancosu P, Alongi F, Clerici E, Tozzi A, Iftode C, Reggiori G, Tomatis S, Infante M, Alloisio M, Testori A, Fogliata A, Cozzi L, Morenghi E, Scorsetti M (2013) Volumetric modulated arc therapy with flattening filter free (FFF) beams for stereotactic body radiation therapy (SBRT) in patients with medically inoperable early stage non small cell lung cancer (NSCLC). Radiother Oncol 107:414–418
Verbakel WF, van den Berg J, Slotman BJ, Sminia P (2013) Comparable cell survival between high dose rate flattening filter free and conventional dose rate irradiation. Acta Oncol 52:652–657
Steenken C, Fleckenstein J, Kegel S, Jahnke L, Simeonova A, Hartmann L, Kübler J, Wenz F, Herskind C, Giordano FA (2015) Impact of flattening-filter-free (FFF) radiation on the clonogenic survival of astrocytic cell lines. Strahlenther Onkol 191:590–596
Boda-Heggemann J, Mai S, Fleckenstein J, Siebenlist K, Simeonova A, Ehmann M, Steil V, Wenz F, Lohr F, Stieler F (2013) Flattening-filter-free intensity modulated breath-hold image-guided SABR (Stereotactic ABlative Radiotherapy) can be applied in a 15-min treatment slot. Radiother Oncol 109(3):505–509
Shimizu S, Shirato H, Kagei K, Nishioka T, Bo X, Dosaka-Akita H, Hashimoto S, Aoyama H, Tsuchiya K, Miyasaka K (2000) Impact of respiratory movement on the computed tomographic images of small lung tumors in three-dimensional (3D) radiotherapy. Int J Radiat Oncol Biol Phys 46(5):1127–1133
Mechalakos J, Yorke E, Mageras GS, Hertanto A, Jackson A, Obcemea C, Rosenzweig K, Clifton Ling C (2004) Dosimetric effect of respiratory motion in external beam radiotherapy of the lung. Radiother Oncol 71:191–200
Guckenberger M, Meyer J, Wilbert J, Baier K, Mueller G, Wulf J, Flentje M (2006) Cone-beam CT based image-guidance for extracranial stereotactic radiotherapy of intrapulmonary tumors. Acta Oncol 45:897–906
Wu J, Betzing C, He TT, Fuss M, D’Souza WD (2013) Dosimetric comparison of patient setup strategies in stereotactic body radiation therapy for lung cancer. Med Phys 40:051709
Partridge M, Tree A, Brock J, McNair H, Fernandez E, Panakis N, Brada M (2009) Improvement in tumour control probability with active breathing control and dose escalation: a modelling study. Radiother Oncol 91:325–329
Barnes EA, Murray BR, Robinson DM, Underwood LJ, Hanson J, Roa WH (2001) Dosimetric evaluation of lung tumor immobilization using breath hold at deep inspiration. Int J Radiat Oncol Biol Phys 50:1091–1098
Wong JW, Sharpe MB, Jaffray DA, Kini VR, Robertson JM, Stromberg JS, Martinez AA (1999) The use of active breathing control (ABC) to reduce margin for breathing motion. Int J Radiat Oncol Biol Phys 44:911–919
Cheong KH, Kang SK, Lee M, Kim SS, Park S, Hwang TJ, Kim KJ, Oh do H, Bae H, Suh TS (2010) Evaluation of delivered monitor unit accuracy of gated step-and-shoot IMRT using a two-dimensional detector array. Med Phys 37:1146–1151
Ahunbay E, Li XA (2007) Investigation of the reliability, accuracy, and efficiency of gated IMRT delivery with a commercial linear accelerator. Med Phys 34:2928–2938
Cui G, Housley D, Chen F, Mehta V, Shepard D (2012) Delivery Efficiency and Dosimetric Accuracy of Respiratorygated VMAT Using an Elekta digital accelerator. ASTRO 2012 Poster Presentation
Nicolini G, Vanetti E, Clivio A, Fogliata A, Cozzi L (2010) Pre-clinical evaluation of respiratory-gated delivery of volumetric modulated arc therapy with RapidArc. Phys Med Biol 55:N347–357
Fleckenstein J, Hesser J, Wenz F, Lohr F (2015) Robustness of sweeping-window arc therapy treatment sequences against intrafractional tumor motion. Med Phys 42:1538–1545
Riley C, Yang Y, Li T, Zhang Y, Heron DE, Hug MS (2014) Dosimetric evaluation of the interplay effect in respiratory-gated RapidArc radiation therapy. Med Phys 41:011715
Clivio A, Belosi MF, Cozzi L, Nicolini G, Vanetti E, Bolard G, Fenoglietto P, Krauss H, Fogliata A (2014) On the determination of reference levels for quality assurance of flattening filter free photon beams in radiation therapy. Med Phys 41:021713
Fogliata A, Garcia R, Knoos T, Nicolini G, Clivio A, Vanetti E, Khamphan C, Cozzi L (2012) Definition of parameters for quality assurance of flattening filter free (FFF) photon beams in radiation therapy. Med Phys 39:6455–6464
Hrbacek J, Lang S, Graydon SN, Klöck S, Riesterer O (2014) Dosimetric comparison of flattened and unflattened beams for stereotactic ablative radiotherapy of stage I non-small cell lung cancer. Med Phys 41:031709
Chang Z, Wu Q, Adamson J, Ren L, Bowsher J, Yan H, Thomas A, Yin FF (2012) Commissioning and dosimetric characteristics of TrueBeam system: composite data of three TrueBeam machines. Med Phys 39:6981–7018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A. Simeonova-Chergou, A. Jahnke, L. Jahnke, K. Siebenlist, F. Stieler, S. Mai, J. Boda-Heggemann, F.Wenz, and F. Lohr state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Additional information
Anna Simeonova-Chergou and Anika Jahnke contributed equally to this publication.
Rights and permissions
About this article
Cite this article
Simeonova-Chergou, A., Jahnke, A., Siebenlist, K. et al. Automatically gated image-guided breath-hold IMRT is a fast, precise, and dosimetrically robust treatment for lung cancer patients. Strahlenther Onkol 192, 166–173 (2016). https://doi.org/10.1007/s00066-015-0934-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0934-z