Abstract
Background and Purpose:
To evaluate patterns of care as well as effectiveness and side effects of palliative treatment in four German radiation oncology departments.
Patients and Methods:
All referrals in four German radiation oncology departments (two university hospitals, one academic hospital, one private practice) were prospective documented for 1 month in 2008 (2 months at one of the university hospitals). In palliatively irradiated patients, treatment aims and indications as well as treated sites and fractionation schedules were recorded. In addition, symptoms and side effects were analyzed with standardized questionnaires before and at the end of radiotherapy.
Results:
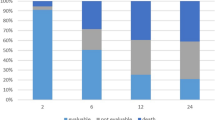
During the observation period, 603 patients underwent radiation therapy in the four centers and 153 (24%, study popu-lation) were treated with palliative intent. Within the study, patients were most frequently treated for bone (34%) or brain (27%) metastases. 62 patients reported severe or very severe pain, 12 patients reported severe or very severe dyspnea, 27 patients reported neurological deficits or signs of cranial pressure, and 43 patients reported a poor or very poor sense of well-being. The most frequent goals were symptom relief (53%) or prevention of symptoms (46%). Life prolongation was intended in 37% of cases. A wide range of fractionation schedules was applied with total doses ranging from 3–61.2 Gy. Of the patients, 73% received a slightly hypofractionated treatment schedule with doses of > 2.0 Gy to ≤ 3.0 Gy per fraction and 12% received moderate to highly hypofractionated therapy with doses of > 3.0 Gy to 8.0 Gy. Radiation therapy led to a significant improvement of well-being (35% of patients) and reduction of symptoms, especially with regard to pain (66%), dyspnea (61%), and neurological deficits (60%). Therapy was very well tolerated with only 4.5% grade I or II acute toxicities being observed. Unscheduled termination was observed in 19 patients (12%).
Conclusions:
Palliative radiation therapy is effective in reducing symptoms, increases subjective well-being, and has minimal side effects. More studies are necessary for subgroup analyses and for clarifying the different goals in palliative radiotherapy.
Zusammenfassung
Ziel:
Evaluation der Alltagspraxis, des Symptomverlaufs und akuter Nebenwirkungen bei palliativer Strahlentherapie in vier strahlentherapeutischen Einrichtungen.
Patienten und Methode:
Alle Erstvorstellungen in den vier Einrichtungen (zwei Universitätskliniken, ein Lehrkrankenhaus und eine private Praxis) wurden einen Monat lang im Jahr 2008 prospektiv dokumentiert und ausgewertet (über 2 Monate in einer der Universitätskliniken). Bei den palliativ bestrahlten Patienten wurden die Indikationen, Behandlungsziele, die bestrahlten Regionen, die Therapiekonzepte und der Behandlungsverlauf dokumentiert. Klinische Symptome und akute Nebenwirkungen wurden zu Beginn und bei Abschluss der Strahlentherapie standardisiert erfasst.
Ergebnisse:
Im Beobachtungszeitraum erhielten 603 Patienten eine Strahlentherapie. 153 Patienten (24%) wurden unter palliativer Zielsetzung bestrahlt, zumeist wegen Knochenmetastasen (34%) oder Hirnmetastasen (27%). Die häufigsten Behandlungsziele waren Symptomlinderung (53%) oder die Prävention klinischer Beschwerden (46%). 66 Patienten berichteten über mittlere oder starke Schmerzen zu Beginn, 12 Patienten berichteten über mittlere oder starke Dyspnoe, 27 Patienten über mittlere oder starke neurologische Ausfälle bzw. Hirndrucksymptomatik, und 43 Patienten berichteten über weniger gutes oder schlechtes Wohlbefinden. In 37% zielte die Strahlentherapie auch auf Lebensverlängerung. Die applizierte Gesamtdosis betrug 3–61,2 Gy. 73% der Patienten wurden mäßig hypofraktioniert bestrahlt (Einzeldosen > 2,0 Gy bis ≤ 3,0 Gy), und 12% der Strahlentherapien wurden mit Einzeldosen > 3,0 Gy–8,0 Gy durchgeführt. Das Allgemeinbefinden war bei 34% der Patienten bei Abschluss der Strahlentherapie signifikant gebessert. 66% der Patienten berichteten eine signifikante Schmerzlinderung, bei 61% konnte Dys-pnoe signifikant gelindert werden, und bei 60% besserten sich neurologische Defizite oder Hirndrucksymptomatik. Die Behand-lung wurde mit 4,5% Grd-I- bis -II-Toxizitäten gut vertragen. 19 Behandlungen wurden vorzeitig abgebrochen (12%).
Schlussfolgerungen:
Die Alltagspraxis und der Symptomverlauf wurden erfolgreich in der Routine dokumentiert. Die palliative Strahlentherapie war gut verträglich, nebenwirkungsarm und wirksam in Bezug auf das Allgemeinbefinden und die Symptomlinderung. Für Subgruppenanalysen und zur Abgrenzung der verschiedenen Endpunkte palliativer Strahlentherapie sind weitere Untersuchungen mit größeren Fallzahlen erforderlich.
Similar content being viewed by others
References
Barnes E, Parliament M, Hanson J et al. Palliative radiotherapy for patients with bone metastases: survey of primary care physicians. Radiother Oncol 2003;67:221–223.
Bradley N, Davis L, Chow E. Symptom distress in patients attending an outpatient palliative radiotherapy clinic. J Pain Symptom Manage 2005;30:123–131.
Bruera E, Michaud M, Vigano A et al. Multidisciplinary symptom control clinic in a cancer center: a retrospective study. Support Care Cancer 2001;9:162–168.
Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton Symptom Assessment Scale. Cancer 2000;88:2164–2171.
Chow E, Abdolell M, Panzarella T, Harris K et al. Validation of a predictive model for survival in metastatic cancer patients attending an outpatient palliative radiotherapy clinic. Int J Radiat Oncol Biol Phys 2009;73:280–287.
Chow E, Davis L, Holden L et al. Prospective assessment of patient-rated symptoms following whole brain radiotherapy for brain metastases. J Pain Symptom Manage 2005;30:18–23.
Chow E, Harris K, Fan G et al. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol 2007;25:1423–1436.
Erridge SC, Gaze MN, Price A et al. Symptom control and quality of life in people with lung cancer: a randomized trial of two palliative radiotherapy fractionation schedules. Clin Oncol (R Coll Radiol) 2005;17:61–67.
Fairchild A, Barnes E, Ghosh S et al. International patterns of practice in palliative radiotherapy for painful bone metastases: evidence-based practice? Int J Radiat Oncol Biol Phys 2009;75:1501–1510.
Fairchild A, Harris K, Barnes E et al. Palliative thoracic radiotherapy for lung cancer: a systematic review. J Clin Oncol 2008;26:4001–4011.
Fairchild A, Pituskin E, Rose B et al. The rapid access palliative radiotherapy program: blueprint for initiation of a one-stop multidisciplinary bone metastases clinic. Support Cancer Care 2009;17:163–170.
Feyer P, Sautter-Bihl ML, Budach W et al. DEGRO Practical Guidelines for palliative radiotherapy of breast cancer patients: brain metastases and leptomeningeal carcinomatosis. Strahlenther Onkol 2010;186:63–69.
Fine P. Palliative radiation therapy in end-of-life care: evidence-based utilization. Am J Hosp Palliat Care 2002;19:166–170.
Glare PA, Sinclair CT. Palliative medicine review: prognostication. J Palliat Med 2008;11:84–103.
Gripp S, Mjartan S, Boelke E et al. Palliative radiotherapy tailored to life expectancy in end-stage cancer patients. Cancer 2010;116:3251–3256.
Halperin E, Perez C, Brady L. Perez and Brady’s Principles and Practice of Radiation Oncology, 5th edn, Philadelphia, Lippincott Williams & Wilkins, 2007.
Janda M, Newman B, Obermair A et al. Impaired quality of life in patients commencing radiotherapy for cancer. Strahlenther Onkol 2004;180:78–83.
Janjan N, Lutz ST, Bedwinek JM et al. Therapeutic guidelines for the treatment of bone metastasis: a report from the American College of Radiology Appropriateness Criteria Expert Panel on Radiation Oncology. J Palliat Med 2009;12:417–426.
Kramer GW, Wanders SL, Noordijk EM et al. Results of the Dutch national study of the palliative effect of irradiation using two different treatment schemes for non-small-cell lung cancer. J Clin Oncol 2005;23:2962–2970.
Lohr KN, Steinwachs DM. Health services research: an evolving definition of the field. Health Services Research 2002;37:15–17.
Lutz S, Spence C, Chow E et al. Survey on use of palliative radiotherapy in hospice care. J Clin Oncol 2004;22:3581–3586.
Lutz S, Chow L, Hartsell W et al. A review of hypofractionated palliative radiotherapy. Cancer 2007;109:1462–1470.
McCloskey SA, Tao ML, Rose CM et al. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J 2007;13:130–137.
National Cancer Institut (NCI). Common toxicity criteria. Division of Cancer Treatment, National Cancer Institute, Bethesda, Maryland (USA) 1988.
Radbruch L, Ostgathe C, Elsner F et al. What is the profile of palliative care in Germany. Results of a representative survey. Schmerz 2004;18:179–188.
Radbruch L, Sabatowski R, Loick G et al. MIDOS — Validierung eines minimalen Dokumentationssystems für die Palliativmedizin. Schmerz 2000;14:231–239.
Rades D, Dunst J, Schild SE. A new scoring system to predict the survival of patients treated with whole-brain radiotherapy for brain metastases. Strahlenther Onkol 2008;184:251–255.
Rades D, Abrahm JL. The role of radiotherapy for metastatic epidural spinal cord compression. Nat Rev Clin Oncol 2010;7:590–598.
Reinfuss M, Mucha-Malecka A, Walasek T et al. Palliative thoracic radiotherapy in non-small cell lung cancer. An analysis of 1250 patients. Palliation of symptoms, tolerance and toxicity. Lung Cancer 2011;71:344–349.
Samant RS, Fitzgibbon E, Meng J et al. Barriers to palliative radiotherapy referral: A Canadian perspective. Acta Oncologica 2007;46:659–663.
Souchon R, Wenz F, Sedlmayer F, Budach W et al. DEGRO practice guidelines for palliative radiotherapy of metastatic breast cancer: bone metastases and metastatic spinal cord compression (MSCC). Strahlenther Onkol 2009;185:417–424.
Steinmann D, Schäfer C, van Oorschot B et al. Effects of radiotherapy for brain metastases on quality of life (QoL). Prospective pilot study of the DEGRO QoL working party. Strahlenther Onkol 2009;185:190–197.
Sperduto PW, Berkey B, Gaspar LE et al. A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 2008;70:510–514.
Sundstrom S, Brennes R, Aasebo U et al. Hypofractionated palliative radiotherapy (17 Gy per two fractions) in advanced non-small-cell Lung carcinoma is comparable to standard fractionation for symptom control and survival: a national phase III trial. J Clin Oncol 2004;22:801–810.
Toy E, Macbeth F, Coles B et al. Palliative thoracic radiotherapy for non-small-cell lung cancer: a systematic review. Am J Clin Oncol 2003;26:112–120.
Van der Linden YM, Dijkstra SP, Vonk EJ et al. Prediction of survival in patients with metastases in the spinal column: results based on a randomized trial of radiotherapy. Cancer 2005;103:320–328.
Voigtmann K, Köllner V, Einsle F et al. Emotional state of patients in radiotherapy and how they deal with their disorder. Strahlenther Onkol 2010;4:229–235.
Wai MS, Mike S, Ines H et al. Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy — a systematic review of the randomized trials. The Cochrane database of systematic reviews (2) 2004; CD004721.
Wong J, Hird A, Zhang L et al. Symptoms and quality of life in cancer patients with brain metastases following palliative radiotherapy. Int J Radiation Oncology Biol Phys 2009;75:1125–1131.
Wu JS, Wong R, Johnston M et al. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys 2003;55:594–605.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Oorschot, B., Schuler, M., Simon, A. et al. Patterns of Care and Course of Symptoms in Palliative Radiotherapy. Strahlenther Onkol 187, 461–466 (2011). https://doi.org/10.1007/s00066-011-2231-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-011-2231-9